Congenital Heart Disease-A Retrospective Study of 156 Cases in Senegal
Article Information
Idrissa Basse1*, Amadou L Fall2, Amadou Sow3, Mouhamed C Léye7, Alain Affangla8, Ndiaga Diakhaté1, Ndiogou Seck4, Lamine Thiam5, Ndiémé Ndiaye1, Ali Bido Sibabi1, Falikou Diaby1, Djibril Boiro3, Aliou A Ndongo6, Ndéye RD Guéye1
1Diamniadio Children’s Hospital Dakar, University of Thiès, Senegal
2Albert Royer National Children’s Hospital, Dakar, Senegal
3Abass Ndao Hospital Center, Dakar, Senegal
4Regional Hospital of Saint Louis, University of Saint Louis, Senegal
5Regional Hospital of Ziguinchor, University of Ziguinchor, Senegal
6Aristide Le Dantec Hospital Dakar, Cheikh Anta Diop University of Dakar, Senegal
7Regional Hospital of Thiès, University of Thiès, Senegal
8Saint Jean de Dieu Hospital Thiès, University of Thiès, Senegal
*Corresponding Author: Idrissa Basse, Diamniadio Children’s Hospital Dakar, University of Thiès, Senegal
Received: 28 September 2020; Accepted: 20 October 2020; Published: 30 October 2020
Citation:
Idrissa Basse, Amadou L Fall, Amadou Sow, Mouhamed C Léye, Alain Affangla, Ndiaga Diakhaté, Ndiogou Seck, Lamine Thiam, Ndiémé Ndiaye, Ali Bido Sibabi, Falikou Diaby, Djibril Boiro, Aliou A Ndongo, Ndéye RD Guéye. Congenital Heart Disease-A Retrospective Study of 156 Cases In Senegal. Journal of Pediatrics, Perinatology and Child Health 4 (2020): 111-116.
View / Download Pdf Share at FacebookAbstract
Introduction: Congenital heart disease (CHD) is the leading cause of congenital malformations. CHD is a real public health problem in our developing countries due to delays in diagnosis and medical and surgical treatment. The general objective of our work was to study the epidemiological, clinical, paraclinical and therapeutic profile of CHD in a university hospital in Dakar.
Methodology: We conducted a retrospective study for a period of 3 years (1st January 2015 to 31st December 2017).
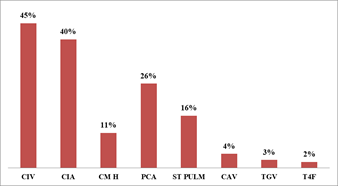
Results: During the study period, we retained 156 files with a hospital prevalence of 2.4%. The average pulse oxygen saturation of the patients was 89%. Ventricular septal defect (VSD) was the most frequent (45%), followed by atrial septal defect (ASD) (40%), patent ductus arteriosus (PDA) (26%), pulmonary stenosis (16%), atrioventricular septal defect (ASD) (4%) and Tetralogy of Fallot (2%). The sex ratio was 0.89. 93.10% of the patients were aged up to 24 months (n=148) against 6.90% aged over 24 months (n=11). The average pulse oxygen saturation of the patients was 89%. Ventricular septal defect (VIC) was the most frequent (45%), followed by atrial septal defect (ASD) (40%), patent ductus arteriosus (PCA) (26%), pulmonary stenosis (16%), atrioventricular septal defect (VAD) (4%) and Tetralogy of Fallot (2%).The sex ratio was 0.89. Among the patients, 93.10% were aged up to 24 months (n=148) compared to 6.90% aged over 24 months (n=11). The average age of children was 9 months.
Conclusion: CHD are a reality in Africa, their frequencies in all reported series are certainly underestimated due to the very limited means of diagnosis.
Keywords
Heart disease, Malformations, Congenital, Children, Senegal
Heart disease articles; Malformations articles; Congenital articles; Children articles; Senegal articles
Article Details
1. Introduction
Congenital heart disease (CHD) is a heart defect, abnormality of cardiac structure or function that is present from birth and can be discovered late [1]. They are the primary cause of congenital malformations; they may be isolated or form part of a poly malformative syndrome [2]. The etiologies are multiple and may be of maternal origin or result from an anomaly specific to the embryo. The estimated prevalence of 8 cases per 1000 live births in France is unknown in our regions due to the limited human, financial and technical resources available for reliable neonatal screening. The overall incidence is 2 to 11 cardiac malformations per 1000 live births [3]. There are now more than 200 different CHD, from the simplest to the most complex [4]. In these newborns, a delay in diagnosis increases the rate of morbidity and can even be fatal [5]. Today, antenatal diagnosis is possible thanks to the progress of fœtal cardiology through fetal ultrasound. According to data in the literature, the rate of antenatal diagnosis does not exceed 25% [6]. It should be noted that several studies have shown that the systematic use of a pulse oximeter on the first day of life is effective in the early detection of a cyanogenic heart defect [7, 8]. In Senegal, since the first study on CHD in 1971 by Sankalé, many other studies have focused on this subject. Multidisciplinary care is a real problem in developing countries and this makes the prognosis of CHD more difficult, as it is usually reserved for the long term. However, great progress has been made thanks to this. In spite of the notable progress in this field, CHD is a real public health problem in developing countries. This is linked to a delay in diagnosis due to several factors and to a problem of medical and surgical management. The general objective of our work was to study the epidemiological, clinical profile of CHD.
2. Methodology
Our work took place at the Diamniadio Children’s Hospital (DCH) for a period of 3 years from 1 January 2015 to 31 December 2017. It is a retrospective study focusing on the epidemiological, clinical, paraclinical and therapeutic aspects of CHD. We have collected all the records of congenital heart diseases hospitalized during the study period. Included in the study were all children aged 0 to 15 years of age, who had a diagnosis of congenital heart disease confirmed by cardiac ultrasound and who required a stay in a paediatric emergency department, neonatology department or hospitalization during the study period. Data were entered and analyzed using sphinx and Microsoft office Excel 2010 software under Windows 7. Statistical analysis used the Chi 2 test.
3. Result
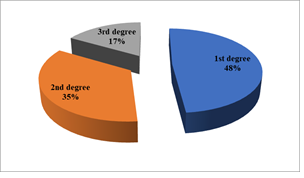
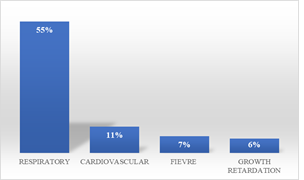
During the study period, we collected 172 files of children with congenital heart disease hospitalized at the Children's Hospital of Diamniadio (CHD), of which 156 were retained. Congenital heart disease represented 2.4% of the 6,562 children seen at the CHD, with a predominance from March to June and another peak in frequency from August to October. It was found that 93.10% of patients were aged 24 months or less (n=148) compared to 6.90% aged over 24 months (n=11). The average age of the children was 9 months with extremes of 0 days and 168 months (14 years). The sex ratio was 0.89. Consanguinity was identified in 35% of patients (n=55), 48% of whom were in the 1st degree (Figure 1). Respiratory and cardiovascular signs were the main reasons for hospitalization noted among children with congenital heart disease (Figure 2). Two (2) patients had a z-score > +2 or 1.26%, 70 patients had a z-score between -2< z-score <+2 or 44.02% and 87 patients had a z-score ≤ -2 or 54.72% (Table 1). Saturation was above 96% in 78 patients (49.05%), between 80 and 95% in 52 patients (32.70%), between 60 and 80% in 15 patients (9.4%) and below 60% in 14 patients (8.85%). The mean heart rate of the patients was 142 with a standard deviation ± 23 and extremes ranging from 65 to 273. The mean respiratory frequency of the patients was 53 with a standard deviation ± 15 and extremes ranging from 17 to 97. Table 2 shows the distribution of clinical signs. The chest X-ray detected cardiomegaly in 64% of patients (n=102) and abnormal pulmonary vascularity in 67% of patients (n=106). Out of the 159 patients, only 8% or 13 patients were able to have an electrocardiogram. Figure 3 gives the distribution of the heart diseases found. In addition, other abnormalities were noted on cardiac ultrasound with tricuspid atresia (n=3), i.e. 3.14%, a common arterial trunk (n=2), i.e. 1.26%, and a coronary artery anomaly (n=1), i.e. 0, 63%, pulmonary atresia (n=5) or 3.14%, septal hypertrophy (n=4) or 2.52%, pulmonary hypoplasia (n=1) or 0.63% and abnormal pulmonary venous return (n=1) or 0.63%. Only 11 patients were able to have curative surgical treatment, i.e. 6.9%. The evolution during hospitalization was favorable among the 128 patients (81%).
|
Weight/Height |
Number |
Percentage |
|
z-score ≤ -2 |
87 |
54.72% |
|
-2< z-score <+2 |
70 |
44.02% |
|
z-score > +2 |
2 |
1.26% |
|
Total |
159 |
100% |
Table 1: Distribution of weight/height indices according to z-score.
|
Clinical signs |
Number |
Percentage |
|
DYSPNEA |
131 |
82% |
|
RESPIRATORY DISTRESS |
116 |
73% |
|
HEART MURMUR |
77 |
48% |
|
HEPATOMEGALY |
53 |
33% |
|
DYSMORPHIA |
52 |
32% |
|
CYANOSIS |
30 |
19% |
|
OEDEME |
24 |
15% |
|
CLINICAL ANEMIA |
22 |
14% |
|
DIGITAL HIPPOCRATISM |
09 |
06% |
|
THORACIC DEFORMITY |
04 |
03% |
Table 2: Distribution of clinical signs.
CIV=ventricular septal defect; CIA=auricular septal defect; PCA=persistent ductus arteriosus; ST PULM= pulmonary stenosis; CAV=common arterial trunk; TGV=Transposition of large vessels; T4F=Fallot Tetralogy
4. Discussion
In our study, the hospital incidence of CHD was 0.0024%, i.e. a prevalence of 2.4 per 1000 children hospitalized at the DHC. In Madagascar, one study found a prevalence of 4.63 per 1000 births and another study in Senegal found a prevalence of 1.8 per 1000 hospitalized children in 2005 [9, 10]. The average age of patients was 9 months in our series. Most CHD are diagnosed at an early age in 70% of cases between 0 and 2 years [11]. The sex ratio was 0.89 compared to other studies which showed different results [12, 6]. First degree parental consanguinity was found in 48%. BAH [6] identified parental inbreeding in 54.2% of patients and first degree in most cases. Isolated atrial septal defect (ASD) and ventricular septal defect (VSD) are the most common CHD as reported in the literature [6, 13-15, 16]. In our study, only 11 patients had undergone a complete cure for heart disease, i.e. 6.9%. Of these, 2 had tetralogy of Fallot (T4) type heart disease and the last had persistent ductus arteriosus (PDA). The same results were found in the work of Bah [6] where the indication for surgery was given in most cases and a surgical cure was made in only 45 patients with simple postoperative after-effects. The number of patients having undergone surgery remains very low compared to Western countries where more than 80% are operated on [17, 18]. The evolution during hospitalization was favorable among the 128 patients (80.5%). In our study, we reported 3 cases of death, 1.8% due to cardiorespiratory arrest by cardiac decompensation and 23 deaths secondary to a nosocomial infection, 14.4%. The death rate was 3.1% in the Bah series [6].
5. Conclusion
Our retrospective work allowed us to confirm that congenital heart disease was a reality in our regions. In spite of the weakness of our means, our study showed considerable efforts towards the early diagnosis of congenital heart disease. However, there is an important gap if we compare our results with those of developed countries. These studies make it possible to provide genetic counselling for high-risk situations, to make diagnostic means accessible, to improve technical platforms and to strengthen the human and technical capacities of cardio-paediatric clinics.
References
- Bodian M, Ngaide AA, Mbaye A, et al. Prevalence of congenital heart disease in Koranic schools (daara) in Dakar: cross-sectional study based on clinical and ultrasound screening of 2019 students. Bull Soc Pathol Exot 108 (2015): 32-35.
- Wallgren EI, Landtman B, Rapola J. Extracardiac Malformations Associated with Congenital Heart Disease (Statistical study of 1000 cases). European Journal of Cardiology 7 (1978): 15-24.
- Gnansia RE, Francannet C. Epidemiology, etiology and genetics of congenital heart disease. EMC-cardiology 11 (2004): 940-920.
- Griscelli C, Sidi D, Munnich A, et al. Congenital heart disease. Third debate of the Wyeth Foundation for the Care of the Child and Adolescent (2005).
- Wren C, Richmonds, Donaldson L. Presentation of congenital heart disease in infancy: implications for routine examination. Arch Dis Child F 80 (1999): 49-53.
- Bah Keyndou Acrachi. Congenital heart disease in pediatric settings: epidemiological, clinical, paraclinical and evolutionary aspects concerning 355 cases in Dakar hospital. Thèse Med (2007).
- Arlettaz R. Recommendations concerning neonatal screening for congenital heart disease. Paediatrica 16 (2005): 38-41.
- Meberg A, Brügmann-Pieper S, Due R, et al. First day of life pulse oximetry screening to detect congenital heart defects. J Pediatr 152 (2008): 761-765.
- Rakotoarimanana S, Rabearivony N, Rakotonirina H, et al. Prevalence of heart murmurs in newborns in Antsirabe- Madagascar Médecine d'Afrique Noire 5306 (2006): 379-382.
- Abdillahi Nour Abdirahman. Epidemiological aspects of congenital heart disease in pediatric settings in chnear / Dakar in relation to 249 cases. These (2011).
- Cloarec S, Magontier N, Vaillant MC, et al. Prevalence and distribution of congenital heart disease in Indre et Loire: evaluation of antenatal diagnosis: 19991-1994 Arch. Pediatr 6 (1999): 1059-1065.
- Leye BOMM. Management of congenital heart disease in Senegal by interventional catheterization: Experience of the cardiological clinic of the Aristide Le Dantec University Hospital: About 15 cases Thesis Med. Cheikh AntaDiop University of Dakar (2005).
- Aboussad Abdelmounaim. Management of congenital heart disease in pediatric settings. In Maghreb health. Tropical health (2002).
- Cardiopathies Congenitales. Sante tropicale.
- El Amrani. Épidémiologie des cardiopathies congénitales. Thèse de Med. Casablanca (1992).
- Diop IB, Ba SA, Ba K, et al. Congenital heart disease: anatomo-clinical, prognostic and therapeutic aspects of 103 cases observed at the cardiological clinic of the Dakar University Hospital. Dakar-Med 40 (1995): 181-186.
- Kociszewska-Najman B, Zacharska-Kokot E, Kulikowska-Matlosz J, et al. Echocardiographic abnormalies in infants with heart murmur Ginekol. Pol 75 (2004): 445-450.
- Stos B. Breath and rhythm: a start sometimes with a bang for newborns. Mt pediatrics 8 (2005): 362-366.


 Impact Factor: * 3.8
Impact Factor: * 3.8 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 