The Effect of Admission Hypothermia on Newborn
Article Information
Ali Almudeer1*, Muneerah Najmi2, Easa Magfori2, Mohammed Salawi2
1Department of Pediatric- NICU, King Saud University Medical City, Riyadh, KSA
2Department of NICU, King Fahd Central Hospital, Jazan- KSA
*Corresponding Author: Ali Almudeer, Department of Pediatric- NICU, King Saud University Medical City, Riyadh, KSA.
Received: 06 June 2023; Accepted: 13 June 2023; Published: 21 June 2023
Citation:
Ali Almudeer, Muneerah Najmi, Easa Magfori, Mohammed Salawi. The Effect of Admission Hypothermia on Newborn. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 117-127.
View / Download Pdf Share at FacebookAbstract
Objective: Consequences of hypothermia is associated with higher mortality and morbidity therefore, thermal control following delivery is an essential of neonatal care. We decided to learn more about thermal regulating procedures in our unit. The goal of this study was to determine the temperature at the time of admission to our neonatal intensive care units (NICUs) and how it relates to death and other morbidity. We also interested to look into the newborn interventions after delivery to control temperature and see how these interventions affect thermal regulation.
Methods: Prospective cohort study using perinatal chart review data for all babies admitted to the NICU at King Fahd central hospital in Jazan. 300 babies through period of April 2021 to March 2022. Hypothermia was classified according to WHO definition as mild (36–36.5°C), moderate (32–35.9°C), or severe (32°C) when the temperature dropped below 36.5°C. We used a multivariable logistic regression analysis to investigate the adjusted effect of hypothermia on neonatal mortality and complications The regression analysis results were provided as crude/unadjusted odds ratios (OR) and adjusted odds ratios (AOR) with 95% confidence intervals (CIs).
Results: Of the infants included in the dataset Almost half of them (49.3%) had abnormal body temperature, 20.7%, 11.3%, and 17.3% had mild, moderate, and severe hypothermia respectively. Around 20% of newborns were given a bath 2 hours after birth, 36% their head covered with hats, and 21.7% had skin-to-skin contact. The adjusted model found that newborns with severe hypothermia were 0.53 (OR = 0.53; [95% CI: 0.15-1.83]) times likely to die and 2.04 (OR = 2.04; [95% CI: 0.76-5.46]) times likely to develop any complication when compared to newborns without hypothermia. Newborns with low birth weight (OR = 16.5; [95% CI: 1.47-185.7]) and without skin-to-skin contact (OR = 3.27; [95% CI: 1.33-8.04]) were more likely to develop any complication when compared to those with skin-to-skin contact.
Conclusion: Hypothermia, low birth weight, abnormal CBC, and absence of skin-to-skin contact all raise the risk of neonatal morbidity, according to this study. According to the study, thermal regulation techniques such as head coverings, skin-to-skin contact, and delayed bathing are not widespread in Saudi Arabian hospitals. These findings call for a review of the procedures or recommendations, as well as an assessment of how well the thermal regulation rules are being followed in NICUs.
Keywords
Hypothermia; Neonatal morbidity; Mortality; Temperature regulation; Saudi Arabia
Hypothermia articles; Neonatal morbidity articles; Mortality articles; Temperature regulation articles; Saudi Arabia articles
Article Details
1. Introduction
Monitoring temperature in the neonatal care units (NICUs) has been always considered a key component of neonatal care [1]. Without taking the necessary actions, a newborn can develop hypothermia, a condition characterized by a body temperature of less than the normal range of 36.5°C to 37.5°C as defined by the World health organization [2]. The burden of neonatal hypothermia varies across the countries and its incidence also differs in community-based and hospital-based studies [3]. Neonatal hypothermia is a contributing factor to neonatal morbidity, mortality, and rise in admissions to NICUs [4]. Hypothermic newborns are five times more likely to experience mortality than newborns with normal body temperatures [5]. Factors such as preterm delivery, lack of warm interfacility transportation, no hat or cap on newborn head, no skin-to-skin contact, and medical practices such as prolonged resuscitation can increase the probability of a newborn becoming hypothermic [6]. In addition, a newborn is prone to develop hypothermia due to the large body surface area and sudden exposure to changes in the temperature [7]. Without taking preventive measures, a hypothermic child can experience adverse and negative effects when exposed to the external environment [8,9]. This tendency to develop hypothermia is more in newborns with low birth weight or premature delivery than in babies with term deliveries and normal birth weight [10].
The importance of temperature in the NICUs has been reflected over time by the influx of machines such as heated mattresses and radiant warmers [11,12]. The need of maintaining the body temperature in newborns is also recognized by the development of novice models of incubators over the last two centuries [13]. Further, monitoring the temperature of the places where a newborn is delivered, such as the delivery room or operation theatre, is a crucial part of thermal regulation [14]. In addition, mothers of newborns are encouraged to follow healthy practices such as delayed bathing, wrapping the newborn’s head with warm linen, head hats, and skin-to-skin contact [3,15]. These practices prevent the newborn from developing hypothermia (<36.5°C) and associated complications. However, the goal of maintaining normal body temperature and avoiding hypothermia is not easily obtained due to either lack of compliance with the guidelines or policies [16].
Despite the enormous literature available on the risk factors and consequences of hypothermia, there is a need to understand the thermal regulation practices in hospitals in our country and gaps we need to work on. Besides, it is important to investigate how neonatal hypothermia is associated with mortality and other complications in newborns in Saudi populations. Therefore, we aimed to conduct this study to measure the temperature at admission to our NICU and how the newborn temperature is associated with mortality and other complications. We also aimed to audit the practices of neonatal interventions after delivery and how the interventions can affect thermal regulation.
2. Material and Methods
2.1 Study design and settings
A prospective cohort study was undertaken in a tertiary hospital in Jazan from April 2021 to March 2022 in King Fahd central hospital. This hospital enrolls about 4 to 5 thousand newborn infants each year. We collected data on important variables on excel sheets and the data were fully anonymous.
2.2 Eligibility criteria and sample size
We included all newborns who were admitted to King Fahd Central Hospital in Jizan from April 2021 to March 2022. Any newborn who was delivered to another hospital was excluded from the study. In addition, any newborn who was admitted from some external hospital to King Fahd Central Hospital after three hours from the delivery room was excluded. Based on the monthly admission of about 50 to 60 babies in the NICU, we calculated a sample size of 300 admissions in the given time frame of about one year.
2.3 Data collection
Data on body temperature were collected in addition to collecting data on room temperature or the temperature where the newborn was born. The ideal range for newborn body temperature ranged between 36.5 and 37.5. According to the WHO, hypothermia was defined as temperature < 36.5 °C and was classified into mild (36–36.5°C), moderate (32–35.9°C), and severe (< 32°C). The body temperature of the newborn was taken from the rectal area using a sterile thermometer and by following the protocol. Further, oxygen saturation and heart rate were recorded within 2–3 hours after birth. In addition, data were collected on variables such as mode and location of delivery, maternal analgesia during delivery, cord clamping (CC) modality and time taken to cord cut, skin-to-skin contact, bathing during the first 2 hours of life, maternal body temperature and room temperature where the newborn was born and time of resuscitation and time taken to arrive at NICU. The primary outcome of neonatal mortality was collected and dichotomized into dead or (survived) cured. Besides, the secondary outcome of various complications was also collected. All newborns were followed until they recovered or developed the outcome of interest. The data on complications such as neonatal sepsis and other complications were collected. A binary variable of “any complication” and “no complication” was developed.
2.4 Statistical methods
To describe the characteristics of the study population, we reported frequencies and proportions. More specifically, we reported frequencies and proportions to describe the characteristics of the study population for the categorical variables such as gender, length of stay, mortality, complications, skin-to-skin contact, head hats, bathing within 2 hours, gestational age, and birth weight, etc. We reported mean and standard deviation for normally distributed variables and median with interquartile range for skewed data. We used a Chi-squared test or Fisher’s exact to assess the frequency distribution and the relationship between covariates and primary outcome of mortality and secondary outcome of any complication. We performed a univariable logistic regression analysis to determine the individual effect of primary exposure to hypothermia on newborn mortality and complications. We considered a p-value of less than 0.05 for significant results. Finally, we conducted a multivariable logistic regression analysis to determine the adjusted effect of hypothermia on newborn mortality and complications. We presented the results of regression analysis by crude/unadjusted Odds ratio (OR) and adjusted odds ratio (AOR) with 95% Confidence Intervals (CIs). We used SPSS 23.0 to analyze the data.
3. Results
3.1 Descriptive characteristics of newborns admitted to the hospital
We collected and analyzed data from 300 newborns. While analyzing the maternal characteristics at the time of labor, gestational age was less than 36 weeks for almost half of the mothers of newborns (49%) and an almost similar proportion of mothers (47.7%) did not get any type of anesthesia at the time of labor as sown in Table 1. The mean body temperature of mothers at the time of delivery was 36.75 with a standard deviation of 0.38. A little over half (52.3%) of the mothers delivered in the operation room, whereas 47.7% delivered in the labor or delivery room. Almost half of the mothers (45.3%) delivered spontaneously via normal vaginal delivery, whereas 51.7% delivered by C-section (Table 1).
|
Variable |
n |
% |
|
Maternal characteristics at the time of labor |
||
|
Gestational age |
||
|
< 36 weeks |
147 |
49 |
|
>= 36 weeks |
153 |
51 |
|
Maternal analgesia |
||
|
None |
143 |
47.7 |
|
GA |
23 |
7.7 |
|
Spinal |
134 |
44.7 |
|
Maternal body temperature (Mean ±SD) |
36.75 |
0.38 |
|
Location of delivery |
||
|
Delivery room |
143 |
47.7 |
|
Operating room |
157 |
52.3 |
|
Mode of Delivery |
||
|
Vaginal delivery |
136 |
45.3 |
|
C-Section |
155 |
51.7 |
|
Instrumental assisted vaginal delivery |
9 |
3 |
|
Newborn characteristics at the time of birth |
||
|
Gender of newborn |
||
|
Male |
190 |
63.3 |
|
Female |
107 |
35.7 |
|
Undetermined |
3 |
1 |
|
Birthweight (kgs) |
||
|
< 1 |
37 |
12.3 |
|
1 to 1.5 |
60 |
20 |
|
1.5 to 2.5 |
111 |
37 |
|
>2.5 |
92 |
30.7 |
|
Newborn birth temperature |
||
|
36.5 to 37.5°C |
152 |
50.7 |
|
36 to 36.5 °C |
62 |
20.7 |
|
32 to 35.9 °C |
34 |
11.3 |
|
<32 °C |
52 |
17.3 |
|
Complete blood count |
||
|
Leukocytosis>15000 |
56 |
18.7 |
|
Leukopenia<4000 |
3 |
1 |
|
Thrombocytopenia<150000 |
21 |
7 |
|
Anemia<12 |
2 |
0.7 |
|
Normal |
157 |
52.3 |
|
Combination of at least two |
61 |
20.3 |
|
Oxygen saturation (Mean ±SD) |
96.58 |
4.9 |
|
Heart rate (Mean ±SD) |
133.47 |
18.2 |
|
Practices to regulate newborn temperature |
||
|
Inotrope Support |
||
|
Yes |
70 |
23.3 |
|
No |
230 |
76.7 |
|
Respiratory support |
||
|
Yes |
263 |
87.7 |
|
No |
37 |
12.3 |
|
Respiratory support type |
||
|
CPAP |
105 |
35 |
|
NC |
103 |
34.3 |
|
CMV |
40 |
13.3 |
|
HFO |
15 |
5 |
|
Bathing during the first 2 hours |
||
|
yes |
59 |
19.7 |
|
No |
241 |
80.3 |
|
Head Hats |
||
|
yes |
108 |
36 |
|
No |
192 |
64 |
|
Skin to skin contact |
||
|
yes |
65 |
21.7 |
|
No |
235 |
78.3 |
|
Cord clamping time and modality |
||
|
DCC 60 sec |
133 |
44.3 |
|
ECC and LT 60 sec |
167 |
55.7 |
|
Complications and outcomes after staying in the hospital |
||
|
Mortality |
||
|
Survived to discharge (Cured) |
247 |
82.3 |
|
Died |
53 |
17.7 |
|
Length of stay |
||
|
≤ 14 days |
207 |
69 |
|
> 14 days |
93 |
31 |
|
Complications |
||
|
No complication |
163 |
54.3 |
|
NEC |
30 |
10 |
|
Sepsis |
28 |
9.3 |
|
BPD |
18 |
6 |
|
IVH |
17 |
5.7 |
|
PVL |
5 |
1.7 |
|
Required CPR |
38 |
13 |
|
PPHTN |
24 |
8 |
|
ROP |
9 |
3 |
|
Combination of at least two complications |
82 |
27.3 |
Table 1: Sociodemographic, clinical characteristics and the outcome of the enrolled newborns and their mothers (n=300).
Concerning the newborn characteristics, we found that 63.3% of the newborns were males and 35.7% were females. Almost one-third of the newborns (30.7%) were born with a birth weight of more than 2.5kg, and 12.3% had a birth weight of <1kg. Regarding temperature, almost half of the newborns (49.3%) had abnormal temperature at admission while other (50.7%) had a normal body temperature of 36.5°C to 37.5°C, meaning they were not hypothermic. In contrast, 20.7% had mild hypothermia, 11.3% had moderate hypothermia, and 17.3% had severe hypothermia as shown in Figure 1. Similarly, approximately half of the neonates had normal complete blood count, 18.7% had leukocytosis, and 20.3% had a combination of any pathology (anemia, thrombocytopenia, leucopenia, and or leukocytosis). The mean oxygen saturation level was 96.58 with a standard deviation of 4.9 and the mean heart rate was 133.5 with a standard deviation of 18.2 (Table 1).
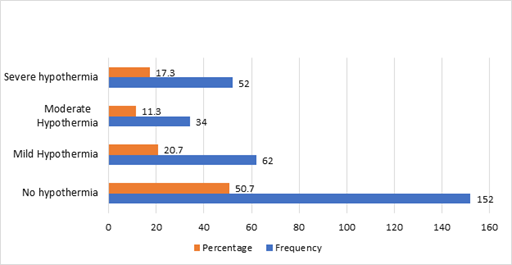
Figure 1: Temperature of newborn and burden of hypothermia among Saudi Children.
Regarding practices to regulate newborn temperature, we found that 23.3% of the newborns were given inotrope support and 87.7% were given respiratory support. Almost one-third of the neonates (35%) received CPAP as a method of respiratory support. With respect to the other practices to regulate newborn temperature, we found that 19.7% of newborns were given a bath within 2 hours of birth, 36% of heads were covered with hats, and 21.7% had skin-to-skin contact as shown in Table 1. Regarding neonatal morbidity and mortality, we found that 45.7 % did have some complications, 10% had NEC, 9.3% had sepsis, 6% had BPD, 5.7% had an intraventricular hemorrhage, 13% had CPR, 8% had PPHTN, 3% had ROP, and one-quarter of the newborns (27.3%) had a combination of at least two complications (Figure 2). Almost one-third of the newborns (31%) stayed longer in the hospital than 14 days (Table 1) and 17.7% died in the hospital (Figure 3).
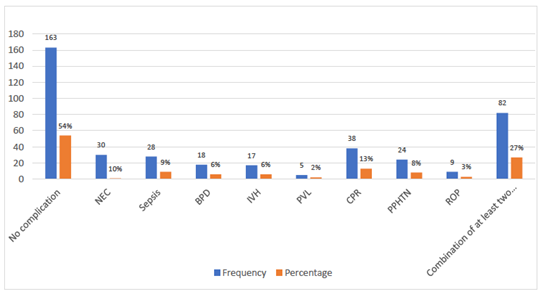
Figure 2: Number and proportion of neonates with complications.
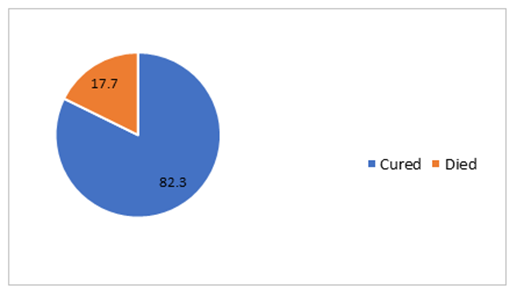
Figure 3: Neonatal Mortality in NICU.
3.2 Distribution of complications by newborn birth temperature
Table 2 below shows the Distribution of complications by newborn birth temperature. The data shows that 25% of the newborns with NEC had normal temperature, whereas 22% had severe hypothermia. Likewise, 32% of the newborns with sepsis had severe hypothermia, whereas 48% of the newborns with sepsis had normal temperature. In contrast, almost one third of newborns diagnosed with PPHN had normal temperature, and 41.7% of the newborns with PPHN had severe hypothermia. The pattern of temperature for ROP was consistent and almost 33.3% of the newborns with ROP had severe hypothermia. Approximately one third (33.3%) of the newborns with IVH had normal temperature and 20% had each moderate and severe hypothermia as shown in Table 2.
|
Newborn birth temperature |
No Complication |
Complications |
|||||||
|
NEC |
Sepsis |
BPD |
IVH |
PVL |
CPR |
PPHTN |
ROP |
||
|
36.5 to 37.5°C |
105 (64.8) |
8 (25.0) |
12 (48.0) |
3 (17) |
5 (33.3) |
1 (20.0) |
14 (36.8) |
7 (29.2) |
2 (22.2) |
|
36 to 36.5 °C |
28 (17 .3) |
9 (28.1) |
2 (8.0) |
7 (39) |
4 (26.7) |
2 (40.0) |
14 (36.8) |
4 (16.7) |
2 (22.2) |
|
32 to 35.9 °C |
12 (7.4) |
8 (25.0) |
3 (12.0) |
6 (33) |
3 (20.0) |
2 (40.0) |
3 (7.9) |
3 (12.5) |
2 (22.2) |
|
<32 °C |
17 (10.5) |
7 (21.9) |
8 (32.0) |
2 (11) |
3 (20.0) |
0 |
7 (18.4) |
10 (41.7) |
3 (33.3) |
Table 2: Distribution of complications by newborn birth temperature.
3.3 The newborn temperature at birth and thermal regulation practices by newborn morbidity
Table 3 describes the newborn temperature at birth and thermal regulation practices by newborn morbidity. We found that a higher proportion of the newborns who had any complication (47.4%) were given the inotrope support when compared with only 3.1% of the newborns without any complication. Similarly, 97% of the newborns with any complications were given respiratory support compared to 79.8% of those the newborns without any complications (p-value: <0.001). A significantly lower proportion of newborns with any complication (5.8%) were given bathing within two hours compared with newborns without any complication (31.3%; p-value: <0.001). About 64% of the newborns with any complication had head hats when compared with only 13% of newborns without any complication (p-value: <0.001) as shown in Table 3. Around 89% of the newborns with any complication did not receive any skin-to-skin contact service as opposed to 68 % of the newborns without any complication (p-value: <0.001). A significantly higher proportion of the newborns (25.5%) with any complication suffered from severe hypothermia as opposed to 10.4% of the newborns without any complication (p-value: <0.001). Similarly, a higher proportion of the newborns (62.8%) with any complication had a longer length of stay of more than 14 days as opposed to 4.3% of the newborns without any complication (p-value: <0.001) as shown in Table 3.
|
Variable |
Neonatal Mortality |
Neonatal Morbidity |
||||||||
|
Cured |
Died |
P-value |
No complication |
Any complication |
P-value |
|||||
|
n |
% |
n |
% |
n |
% |
n |
% |
|||
|
Inotrope Support |
||||||||||
|
Yes |
33 |
13.4 |
37 |
69.8 |
<0.001 |
5 |
3.1 |
65 |
47.4 |
<0.001 |
|
No |
214 |
86.6 |
16 |
30.2 |
158 |
96.9 |
72 |
52.6 |
||
|
Respiratory support |
||||||||||
|
Yes |
210 |
85 |
53 |
100 |
0.003 |
130 |
79.8 |
133 |
97.1 |
<0.001 |
|
No |
37 |
15 |
0 |
0 |
33 |
20.2 |
4 |
2.9 |
||
|
Bathing during first 2 hours |
||||||||||
|
yes |
56 |
22.7 |
3 |
5.7 |
0.005 |
51 |
31.3 |
8 |
5.8 |
<0.001 |
|
No |
191 |
77.3 |
50 |
94.3 |
112 |
68.7 |
129 |
94.2 |
||
|
Head Hats |
||||||||||
|
yes |
70 |
28.3 |
38 |
71.7 |
<0.001 |
21 |
12.9 |
87 |
63.5 |
<0.001 |
|
No |
177 |
71.7 |
15 |
28.3 |
142 |
87.1 |
50 |
36.5 |
||
|
Skin to skin contact |
||||||||||
|
yes |
61 |
24.7 |
4 |
7.5 |
0.006 |
51 |
31.3 |
14 |
10.2 |
<0.001 |
|
No |
186 |
75.3 |
49 |
92.5 |
112 |
68.7 |
123 |
89.8 |
||
|
Cord clamping time and modality |
||||||||||
|
DCC 60 sec |
124 |
50.2 |
9 |
17 |
<0.001 |
102 |
62.6 |
31 |
22.6 |
<0.001 |
|
ECC and LT 60 sec |
123 |
49.8 |
44 |
83 |
61 |
37.4 |
106 |
77.4 |
||
|
Maternal analgesia |
||||||||||
|
None |
117 |
47.4 |
26 |
49.1 |
0.051 |
88 |
54 |
55 |
40.1 |
0.02 |
|
GA/Spinal |
130 |
52.6 |
27 |
50.9 |
75 |
46 |
82 |
59.9 |
||
|
Location of delivery |
||||||||||
|
DR |
117 |
47.4 |
26 |
49.1 |
0.82 |
88 |
54 |
55 |
40.1 |
0.02 |
|
OR |
130 |
52.6 |
27 |
50.9 |
75 |
46 |
82 |
59.9 |
||
|
Newborn birth temperature |
||||||||||
|
36.5 to 37.5°C |
136 |
55.1 |
16 |
30.2 |
0.002 |
105 |
64.4 |
47 |
34.3 |
<0.001 |
|
36 to 36.5 °C |
48 |
19.4 |
14 |
26.4 |
29 |
17.8 |
33 |
24.1 |
||
|
32 to 35.9 °C |
28 |
11.3 |
6 |
11.3 |
12 |
7.4 |
22 |
16.1 |
||
|
<32 °C |
35 |
14.2 |
17 |
32.1 |
17 |
10.4 |
35 |
25.5 |
||
|
Birthweight (kgs) |
||||||||||
|
< 1 |
11 |
4.5 |
26 |
49.1 |
<0.001 |
1 |
0.6 |
36 |
26.3 |
<0.001 |
|
1 to 1.5 |
50 |
20.2 |
10 |
18.9 |
15 |
9.2 |
45 |
32.8 |
||
|
1.5 to 2.5 |
102 |
41.3 |
9 |
17 |
78 |
47.9 |
33 |
24.1 |
||
|
>2.5 |
84 |
34 |
8 |
15.1 |
69 |
42.3 |
23 |
16.8 |
||
|
Gestational age |
||||||||||
|
< 36 weeks |
107 |
43.3 |
40 |
75.5 |
<0.001 |
49 |
30.1 |
98 |
71.5 |
<0.001 |
|
>= 36 weeks |
140 |
56.7 |
13 |
24.5 |
114 |
69.9 |
39 |
28.5 |
||
|
Length of stay |
||||||||||
|
≤ 14 days |
182 |
73.3 |
25 |
47.2 |
<0.001 |
156 |
95.7 |
51 |
37.2 |
<0.001 |
|
> 14 days |
65 |
26.3 |
28 |
52.8 |
7 |
4.3 |
86 |
62.8 |
||
Table 3: Newborn temperature at birth and thermal regulation practices by neonatal mortality and complications.
3.4 The newborn temperature at birth and thermal regulation practices by newborn mortality
Table 3 describes the newborn temperature at birth and thermal regulation practices by newborn mortality. We found that a higher proportion of the newborns who died (69.6%) were given the inotrope support when compared with 30.0% of the newborns cured and recovered in the hospital. However, 100% of the newborns who died were given respiratory support compared to 85% of those who were cured and recovered in the hospital (p-value: 0.003). A significantly higher proportion of newborns who died (94.3%) were not given bathing within two hours compared with newborns cured and recovered in the hospital (77.3%; p-value: 0.005). About 71.7% of the newborns who died had head hats when compared with 28.3% of newborns cured and recovered in the hospital (p-value: <0.001) as shown in Table 3. Around 93% of the newborns who died did not receive any skin-to-skin contact service as opposed to 75.3 % of the newborns who were cured and recovered in the hospital (p-value: <0.001). A significantly higher proportion of the newborns (32.1%) who died suffered from severe hypothermia as opposed to 14.2% of the newborns cured and recovered in the hospital (p-value: <0.002). Similarly, a higher proportion of the newborns (52.8%) who died had a longer length of stay of more than 14 days as opposed to 26.3% of the newborns cured and recovered in the hospital (p-value: <0.001) as shown in Table 3.
3.5 Association between hypothermia and mortality: Results of multiple regression analyses
Table 4 shows the findings of factors associated with mortality with a special focus on the association between hypothermia and neonatal morbidity and mortality. We found that newborns with severe hypothermia were 0.53 (OR = 0.53; [95% CI: 0.15-1.83]) times more likely to die when compared to newborns without hypothermia (Table 4). Likewise, newborns with moderate hypothermia were 0.29 (OR = 0.29 [95% CI: 0.07-1.19]) times more likely to die when compared to newborns without hypothermia. Overall, the data did not find a significant relationship between neonatal hypothermia and mortality in our study after adjusting for other variables in the model. In contrast, newborns with any abnormality on CBC at admission were 3.79 times more likely to die when compared to the newborns without any pathology on CBC after adjusting for other variables in the model (OR = 3.79; [95% CI:1.49-9.66]). Furthermore, newborns without inotrope support were 0.18 times more likely to die when compared to those with inotrope support after accounting for other variables in the model (OR = 0.18; [95% CI: 0.07-0.45]). This suggests that newborns without intrope support were 82% less likely to die compared with intrope support. In addition, with one unit increase in oxygen saturation, the odds of death reduced by 11%, suggesting that optimal oxygen saturation prevented newborns death (OR = 0.89; [95% CI: 0.83-0.97]). Finally, newborns with an extreme low birth weight of < 1kg were 8.08 times more likely to die (OR = 8.08; [95% CI: 2.33-27.97]) than newborns with normal birth weight (Table 4).
3.6 Association between hypothermia and morbidity: Results of multiple logistic regression
Regarding the association between hypothermia and neonatal morbidity, we found that newborns with severe hypothermia were 2.04 (OR = 2.04; [95% CI: 0.76-5.46]) times more likely to develop any complication when compared to newborns without hypothermia (Table 4). Likewise, newborns with moderate hypothermia were 1.92 (OR = 1.92 [95% CI: 0.59-6.19]) times more likely to develop any complication when compared to newborns without hypothermia. Overall, the data did not find a significant relationship between neonatal hypothermia and newborn morbidity in our study after adjusting for other variables in the model. On the contrary, newborns with any abnormality on CBC were 4.64 times more likely to develop any complication when compared to the newborns without any pathology on CBC after adjusting for other variables in the model (OR = 4.64; [95% CI:2.32-9.28]). Furthermore, newborns without intrope support were 0.1 times more likely to develop any complication when compared to those with intrope support after accounting for other variables in the model (OR = 0.10; [95% CI: 0.03-0.31]). This suggests that newborns without intrope support were 90% less likely to develop any complications compared with intrope support. Lastly, newborns with an extreme low birth weight of < 1kg were 16.5 times more likely to develop any complications (OR = 16.5; [95% CI: 1.47-185.7]) than newborns with normal birth weight (Table 4). Also, newborns without skin-to-skin contact were 3.27 times more likely to develop any complication when compared to those with skin-to-skin contact after accounting for other variables in the model (OR = 3.27; [95% CI: 1.33-8.04]) as shown in Table 4.
|
Variable name |
Neonatal mortality |
Neonatal morbidity |
||||
|
AOR |
95% CI |
AOR |
95% CI |
|||
|
Newborn birth temperature |
||||||
|
36.5 to 37.5°C |
1 |
1 |
||||
|
36 to 36.5 °C |
0.74 |
0.26 |
2.17 |
0.74 |
0.29 |
1.87 |
|
32 to 35.9 °C |
0.29 |
0.07 |
1.19 |
1.92 |
0.59 |
6.19 |
|
<32 °C |
0.53 |
0.15 |
1.83 |
2.04 |
0.76 |
5.46 |
|
CBC |
||||||
|
No CBC pathology |
1 |
1 |
||||
|
At least one CBC pathology |
3.79 |
1.49 |
9.66 |
4.64 |
2.32 |
9.28 |
|
Intrope Support |
||||||
|
Yes |
1 |
|||||
|
No |
0.181 |
0.073 |
0.45 |
0.1 |
0.03 |
0.31 |
|
Oxygen saturation |
0.89 |
0.83 |
0.97 |
NA |
||
|
Birthweight (kgs) |
||||||
|
< 1 |
8.08 |
2.33 |
27.97 |
16.5 |
1.47 |
185.7 |
|
1 to 1.5 |
1.41 |
0.43 |
4.67 |
3.45 |
1.16 |
10.22 |
|
1.5 to 2.5 |
1.26 |
0.39 |
3.99 |
0.89 |
0.38 |
2.07 |
|
>2.5 |
1 |
|||||
|
Heads hat |
||||||
|
Yes |
NA |
1 |
||||
|
No |
0.29 |
0.12 |
0.66 |
|||
|
Skin to skin |
||||||
|
Yes |
NA |
1 |
||||
|
No |
3.27 |
1.33 |
8.04 |
|||
Table 4: Association between hypothermia and neonatal morbidity and mortality
4. Discussion
We conducted this study to measure the temperature at admission to our NICU and how the newborn temperature is associated with mortality and other complications among newborns admitted to NICUs in Saudi Arabia. We also aimed to audit the practices of neonatal management after birth and how the practices can affect thermal regulation. Our study found that almost half of the newborns had some degree of hypothermia. Thermal regulation practices such as skin-to-skin contact, delayed bathing, and wearing of caps was also practiced in NICUs but not by every parent of the newborn. A little below a quarter of the newborns received bathing within 2 hours of birth, one-third of the newborns were found to wear caps, and almost a quarter was given skin-to-skin contact. While the study did not find a significant relationship between hypothermia and neonatal morbidity and mortality, the findings revealed that newborns with severe hypothermia were more likely to develop any complications as shown by the positive effect size of the adjusted odds ratio. Apart from hypothermia, we found that low birth weight babies were more likely to die or develop some complications than normal birth weight babies. Also, those newborns who did not have skin-to-skin contact were more likely to experience neonatal morbidity (complications) than those who were given skin-to-skin contact. Further, newborns with abnormal pathology on CBC at admission were at increased risk of morbidity and mortality. Increased oxygen saturation was observed to be protective for newborns and those who were not given intrope support were also less likely to die or develop any complications.
Although our study did not find a significant association between hypothermia and neonatal complications such as sepsis and intraventricular hemorrhage, the effect size suggests that hypothermia is positively associated with these complications. These findings are consistent with the existing literature, supporting the impact of hypothermia on neonatal morbidity as reflected by a range of complications. For example, a population-based cohort study of 8782 demonstrated that moderate hypothermia was positively associated with a higher risk of intraventricular hemorrhage and neonatal mortality [10]. These findings are further endorsed by previous studies suggesting that cold stress increases the susceptibility of a child to develop complications or to die [17,18]. The evidence suggests that similar to kangaroo mother care, preventing hypothermia is a well-established preventive strategy to prevent neonatal morbidity and mortality in resource-poor settings [19].
Our findings regarding the positive relationship between low birth weight, lack of skin-to-skin contact, and CBC pathology with neonatal morbidity and mortality are analogous to other studies conducted across the world. For example, a study conducted in Egypt on 6701 live births demonstrated that newborns with low birth weight were more likely to admit to NICUS, develop complications such as jaundice at one month, and had a higher risk of mortality than babies with normal birth weight [20]. These findings are confirmed by a study in Bangladesh where authors followed 776 newborns in a cohort study up to one month of age [21]. The authors concluded that neonatal mortality was higher among infants with low birth weight than normal birth weight babies [21]. Likewise, a study conducted in Nigeria on 278 neonates in Special Baby Care Unit found similar results to our study regarding low birth weight as a strong predictor of neonatal morbidity [22]. These findings are not surprising as enormous data and literature support the fact that low birth weight babies tend to experience more deaths than their counterparts [23,24]. This calls for action to improve the nutrition of the mother before and during pregnancy and to address the causes of low birth weight before a newborn is delivered. Necessary measures should be taken by the health leader of in our country to allocate resources to address the burden of low birth weight in our setting.
Similarly, skin-to-skin contact is important to prevent neonatal morbidity. This is in consonance with the findings by some researchers who suggest that skin-to-skin contact provide an optimal environment to newborn and is a cost-effective temperature regulation strategy suitable for poor resource settings [25-27]. For example, findings from a randomized controlled trial revealed that newborns randomized to skin-to-skin contact were in a better position to transfer to extrauterine life than those who were not assigned to skin-to-skin contact [25]. Further, the same babies had less need for respiratory support, antibiotic use, and intravenous fluids during the hospital stay [25]. The evidence suggests that skin-to-skin contact is a well-established, simple, and cost-effective intervention that signifies an environment where a newborn is directly placed on the mother's chest or abdomen to get warmth and have direct ventral-to-ventral skin contact [28]. According to WHO, skin-to-skin contact should be commenced immediately within an hour of delivery of a baby to prevent hypothermia and associated complications [28]. The benefits of skin-to-skin contact have justified the fact that newborns with skin-to-skin contact are more likely to receive breastfeeding, be exclusively breastfed, and be breastfed for a longer duration [29-32]. Further, skin-to-skin contact also improves the autonomic and cognitive function of the baby, thereby reducing neonatal, infant, and childhood morbidity [33,34].
5. Strengths and Limitations
This is the first study to look into the thermal regulation practices and the association between hypothermia and neonatal morbidity and mortality in newborns admitted to NICUs in the south of Saudi Arabia. The findings provide valuable insights into an important clinical issue of hypothermia and its effects on newborn morbidity and mortality. This unique strength of the study may guide clinicians and neonatologists to be mindful of the effects of hypothermia and bad temperature regulation practices in NICUs. Another strength of the current study is that we objectively measured the temperature of the newborn by using a sterile thermometer rather than relying on self-reported data from parents. This would minimize the potential for misclassification bias in the exposure. Similarly, we kept our outcome variable (neonatal mortality) as a binary variable and because it is a hard outcome, the chances of misclassification bias in the outcome are negligible. Besides, we used standard laboratory methods to measure the blood parameters and identify the pathologies such as leukocytosis, anemia, thrombocytopenia, and leukopenia. Also, calibrated weight measurement scales were used to measure the birth weight of newborns and the standard proformas were used to collect the data. Besides, our study was a prospective cohort study that followed neonates prospectively to assess their outcomes. Hence the temporal relationship between hypothermia and neonatal morbidity and mortality can be established. However, there are some potential limitations to this study that must be acknowledged. One of the limitations of this study is our sample size was relatively smaller than other similar studies, which may have prevented us from studying the gender differences. Also, we did not follow newborns beyond one month to assess the long-term outcomes of thermal regulation practices and hypothermia on neonatal morbidity and mortality.
6. Conclusion
This study concludes that hypothermia, low birth weight, abnormal CBC at admission, and lack of skin-to-skin contact increase the risk of neonatal morbidity. Also, the study indicates that thermal regulation practices such as head hats, skin-to-skin contact, and delayed bathing is not universal in the hospitals of our NICU. These findings warrant revisiting the protocols or guidelines or to assess the extent to which the guidelines of thermal regulation are being followed in NICUs. Further, The Saudi health sector needs to coordinate with health representatives to develop programs that can help obstetricians and neonatologists to coordinate collectively to reduce the burden of neonatal mortality and morbidity. This can be done by implementing simple and cost-effective strategies such as kangaroo mother care, thermal regulation practices, using warm surfaces, keeping delivery rooms warm, and providing adequate nutrition to the mother during and before pregnancy to reduce the incidence of low birth weight and associated morbidity.
References
- Freer Y, Lyon A. Temperature monitoring and control in the newborn baby. Paediatrics Child Health 22 (2012): 127-130.
- Chen W, Dols S, Oetomo SB, et al. Monitoring body temperature of newborn infants at neonatal intensive care units using wearable sensors. Proceedings of the Fifth International Conference on Body Area Networks (2010): 188-194.
- Mullany LC. Neonatal Hypothermia in Low-Resource Settings. Seminars in Perinatology 34 (2010): 426-433.
- de Almeida MFB, Guinsburg R, Sancho GA, et al. Hypothermia and early neonatal mortality in preterm infants. The Journal of pediatrics 164 (2014): 271-275.
- Mullany LC, Katz J, Khatry SK, et al. Risk of mortality associated with neonatal hypothermia in southern Nepal. Archives of Pediatrics Adolescent Medicine 164 (2010): 650-656.
- Bayih WA, Assefa N, Dheresa M, et al. Neonatal hypothermia and associated factors within six hours of delivery in eastern part of Ethiopia: a cross-sectional study. BMC Pediatrics 19 (2019): 1-10.
- Ellis J. Neonatal hypothermia. Journal of Neonatal Nursing 11 (2005): 76-82.
- Weirich TL. Hypothermia/warming protocols: why are they not widely used in the OR? AORN Journal 87 (2008): 333-344.
- De Mattia AL, Barbosa MH, Rocha ADM, et al. Hypothermia in patients during the perioperative period. Revista da Escola de Enfermagem da USP 46 (2012): 60-66.
- Miller S, Lee H, Gould J. Hypothermia in very low birth weight infants: distribution, risk factors and outcomes. Journal of Perinatology 31 (2011): S49-S56.
- Ibrahim C, Yoxall C. Use of self-heating gel mattresses eliminates admission hypothermia in infants born below 28 weeks gestation. European Journal of Pediatrics 169 (2010): 795-799.
- Pinheiro J, Furdon SA, Boynton S, et al. Decreasing hypothermia during delivery room stabilization of preterm neonates 133 (2014): e218-e226.
- Stern L. Thermoregulation in the newborn infant: historical, physiological and clinical considerations. Historical Review Recent Advances in Neonatal Perinatal Medicine (1980).
- Laptook AR, Watkinson M. Temperature management in the delivery room. Seminars in Fetal Neonatal Med 13 (2008): 383-391.
- Srivastava S, Gupta A, Bhatnagar A, et al. Effect of very early skin to skin contact on success at breastfeeding and preventing early hypothermia in neonates. Indian Journal of Public Health 58 (2014): 22-26.
- Moola S, Lockwood C. Effectiveness of strategies for the management and/or prevention of hypothermia within the adult perioperative environment. International Journal of Evidence-Based Healthcare 9 (2011): 337-345.
- Costeloe K, Hennessy E, Gibson AT, et al. The EPICure study: outcomes to discharge from hospital for infants born at the threshold of viability. Pediatrics 106 (2000): 659-671.
- Dincsoy M, Siddiq F, Kim Y. Intracranial hemorrhage in hypothermic low-birth-weight neonates. Child's Nervous System 6 (1990): 245-248.
- Lloyd LG, De Witt T. Neonatal mortality in South Africa: How are we doing and can we do better? South African Medical Journal 103 (2013): 518-519.
- Mansour E, Eissa A, Nofal L, et al. Morbidity and mortality of low-birth-weight infants in Egypt. EMHJ-Eastern Mediterranean Health Journal 11 (2005): 723-731.
- Yasmin S, Osrin D, Paul E, et al. Neonatal mortality of low-birth-weight infants in Bangladesh. Bulletin of the World Health Organization 79 (2001): 608-614.
- Onwuanaku CA, Okolo SN, Ige KO, et al. The effects of birth weight and gender on neonatal mortality in north central Nigeria. BMC Research Notes 4 (2011): 1-5.
- Uthman OA. Effect of low birth weight on infant mortality: analysis using Weibull hazard model. Int J of Epidemiol 6 (2008): 8.
- Ballot DE, Chirwa TF, Cooper PA. Determinants of survival in very low birth weight neonates in a public sector hospital in Johannesburg. BMC Pediatrics 10 (2010): 1-11.
- Chi Luong K, Long Nguyen T, Huynh Thi DH, et al. Newly born low birthweight infants stabilise better in skin-to-skin contact than when separated from their mothers: a randomised controlled trial. Acta Paediatrica 105 (2016): 381-390.
- Baley J, Watterberg K, Cummings J, et al. Skin-to-skin care for term and preterm infants in the neonatal ICU. Pediatrics 136 (2015): 596-599.
- Chan GJ, Valsangkar B, Kajeepeta S, et al. What is kangaroo mother care? Systematic Review of the Literature. Journal of Global Health 6 (2016).
- Organization WH. Guideline: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services: World Health Organization (2017).
- Marín Gabriel M, Llana Martín I, López Escobar A, et al. Randomized controlled trial of early skin-to-skin contact: effects on the mother and the newborn. Acta Paediatrica 99 (2010): 1630-1634.
- Mikiel-Kostyra K, Mazur J, Boltruszko I. Effect of early skin-to-skin contact after delivery on duration of breastfeeding: a prospective cohort study. Acta Paediatrica 91 (2002): 1301-1306.
- Mori R, Khanna R, Pledge D, et al. Meta-analysis of physiological effects of skin-to-skin contact for newborns and mothers. Pediatrics International 52 (2010): 161-170.
- Safari K, Saeed AA, Hasan SS, et al. The effect of mother and newborn early skin-to-skin contact on initiation of breastfeeding, newborn temperature and duration of third stage of labor. International Breastfeeding Journal 13 (2018): 1-8.
- Feldman R, Rosenthal Z, Eidelman AI. Maternal-preterm skin-to-skin contact enhances child physiologic organization and cognitive control across the first 10 years of life. Biological psychiatry 75 (2014): 56-64.
- Mother-baby package (WHO/RHT/MSM/97.2, Rev 1) Geneva: World Health Organization (1997).


 Impact Factor: * 3.8
Impact Factor: * 3.8 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 