Beyond Surgery: Reassessing Appendectomy in Uncomplicated Pediatric Appendicitis cases
Article Information
Mohammad Syfur Rashid1*, Abdul Hanif Tablu2, KM Shaiful Islam3, Mitali Hossain4, Shariful Alam5, Syeda Tamanna Tanjil6
1Department of Pediatric Surgery, Monno Medical College Hospital, Manikgonj, Bangladesh
2Department of Neonatal Surgery, Dhaka Medical College and Hospital, Dhaka, Bangladesh
3Department of Pediatric Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
4MBBS, MPH (NIPSOM), Dhaka, Bangladesh
5Department of Surgical Oncology, National Institutes of Cancer Research and Hospital, Dhaka, Bangladesh
6Consultant Clinical Pathologist, SIBL Foundation Hospital, Panthapath, Dhaka, Bangladesh
*Corresponding Author: Dr. Mohammad Syfur Rashid, Department of Pediatric Surgery, Monno Medical College Hospital, Manikgonj, Bangladesh.
Received: 15 December 2023; Accepted: 22 December 2023; Published: 28 December 2023
Citation: Mohammad Syfur Rashid, Abdul Hanif Tablu, KM Shaiful Islam, Mitali Hossain, Shariful Alam, Syeda Tamanna Tanjil. Beyond Surgery: Reassessing Appendectomy in Uncomplicated Pediatric Appendicitis cases. Journal of Pediatrics, Perinatology and Child Health. 7 (2023): 254-259.
View / Download Pdf Share at FacebookAbstract
Aim: The study aimed to reassess appendectomy in uncomplicated pediatric patients with conservative management.
Background: Pediatric appendicitis, prevalent with a 7-8% lifetime risk, often requires appendectomy, a traditional approach with inherent risks. Recent medical literature challenges this, advocating non-operative interventions like antibiotics or observational management. Surgical complications occur in over 10% of cases. Laparoscopic surgery and a low threshold for intervention contribute to unnecessary surgeries. Approximately 20% of cases are complicated, prompting exploration of non-operative approaches for early uncomplicated cases. Antibiotics, once seen as a prelude to surgery, can now be a safe primary treatment, with a 63% success rate. Limited literature on non-operative treatment in children suggests a 97% effectiveness, offering social and economic benefits, though recurrent appendicitis remains a concern.
Methods: This prospective observational study, conducted at Dhaka Medical College Hospital in Bangladesh from July 2017 to March 2019, focused on uncomplicated acute appendicitis in children up to 12 years. Informed consent was obtained, and an approved research protocol was followed. Inclusion and exclusion criteria were established. A questionnaire collected data on key variables and administered conservative antibiotic treatment. Patients were assessed and followed up over 6 months with clinical examinations and investigations. Data analysis using SPSS-22 included descriptive statistics. The study aimed to evaluate the effectiveness of conservative treatment for uncomplicated acute appendicitis in pediatric patients under 12 years old.
Result: The study, encompassing 62 pediatric appendicitis cases, reveals a concentrated age distribution (mean age: 8.95±2.10 years) in middle childhood. Males dominate (61.3%), suggesting a gender-related factor. Clinical findings exhibit prevalent symptoms of anorexia (80.65%), fever >38°C (80.65%), and acute abdomen triage (83.87%). Pain management, assessed through the Visual Analog Scale, demonstrates a progressive reduction from the first to the fifth day. The appendix diameter decreases significantly over time, indicative of treatment response. Observations underscore a median 16-month post-treatment period, 24-hour symptomto- management time, and 84-hour hospitalization. Successful conservative treatment is notable in 95.1% of cases, emphasizing its efficacy in managing uncomplicated pediatric appendicitis.
Conclusion: The evolving landscape of appendicitis management in pediatric patients suggests a reevaluation of the traditional surgical approach, with non-operative interventions showing promise in terms of safety and efficacy. Further research, particularly in the form of large randomized studies in children, is warranted to establish the long-term effectiveness and potential benefits of non-operative treatments for acute uncomplicated appendicitis.
Keywords
Reassessing; Appendectomy; Acute appendicitis; Children; Conservative treatment
Pediatric appendicitis articles Pediatric appendicitis Research articles Pediatric appendicitis review articles Pediatric appendicitis PubMed articles Pediatric appendicitis PubMed Central articles Pediatric appendicitis 2023 articles Pediatric appendicitis 2024 articles Pediatric appendicitis Scopus articles Pediatric appendicitis impact factor journals Pediatric appendicitis Scopus journals Pediatric appendicitis PubMed journals Pediatric appendicitis medical journals Pediatric appendicitis free journals Pediatric appendicitis best journals Pediatric appendicitis top journals Pediatric appendicitis free medical journals Pediatric appendicitis famous journals Pediatric appendicitis Google Scholar indexed journals Pediatric surgery articles Pediatric surgery Research articles Pediatric surgery review articles Pediatric surgery PubMed articles Pediatric surgery PubMed Central articles Pediatric surgery 2023 articles Pediatric surgery 2024 articles Pediatric surgery Scopus articles Pediatric surgery impact factor journals Pediatric surgery Scopus journals Pediatric surgery PubMed journals Pediatric surgery medical journals Pediatric surgery free journals Pediatric surgery best journals Pediatric surgery top journals Pediatric surgery free medical journals Pediatric surgery famous journals Pediatric surgery Google Scholar indexed journals Neonatal surgery articles Neonatal surgery Research articles Neonatal surgery review articles Neonatal surgery PubMed articles Neonatal surgery PubMed Central articles Neonatal surgery 2023 articles Neonatal surgery 2024 articles Neonatal surgery Scopus articles Neonatal surgery impact factor journals Neonatal surgery Scopus journals Neonatal surgery PubMed journals Neonatal surgery medical journals Neonatal surgery free journals Neonatal surgery best journals Neonatal surgery top journals Neonatal surgery free medical journals Neonatal surgery famous journals Neonatal surgery Google Scholar indexed journals Surgical appendectomy articles Surgical appendectomy Research articles Surgical appendectomy review articles Surgical appendectomy PubMed articles Surgical appendectomy PubMed Central articles Surgical appendectomy 2023 articles Surgical appendectomy 2024 articles Surgical appendectomy Scopus articles Surgical appendectomy impact factor journals Surgical appendectomy Scopus journals Surgical appendectomy PubMed journals Surgical appendectomy medical journals Surgical appendectomy free journals Surgical appendectomy best journals Surgical appendectomy top journals Surgical appendectomy free medical journals Surgical appendectomy famous journals Surgical appendectomy Google Scholar indexed journals General anesthesia articles General anesthesia Research articles General anesthesia review articles General anesthesia PubMed articles General anesthesia PubMed Central articles General anesthesia 2023 articles General anesthesia 2024 articles General anesthesia Scopus articles General anesthesia impact factor journals General anesthesia Scopus journals General anesthesia PubMed journals General anesthesia medical journals General anesthesia free journals General anesthesia best journals General anesthesia top journals General anesthesia free medical journals General anesthesia famous journals General anesthesia Google Scholar indexed journals Appendectomy articles Appendectomy Research articles Appendectomy review articles Appendectomy PubMed articles Appendectomy PubMed Central articles Appendectomy 2023 articles Appendectomy 2024 articles Appendectomy Scopus articles Appendectomy impact factor journals Appendectomy Scopus journals Appendectomy PubMed journals Appendectomy medical journals Appendectomy free journals Appendectomy best journals Appendectomy top journals Appendectomy free medical journals Appendectomy famous journals Appendectomy Google Scholar indexed journals Healthcare articles Healthcare Research articles Healthcare review articles Healthcare PubMed articles Healthcare PubMed Central articles Healthcare 2023 articles Healthcare 2024 articles Healthcare Scopus articles Healthcare impact factor journals Healthcare Scopus journals Healthcare PubMed journals Healthcare medical journals Healthcare free journals Healthcare best journals Healthcare top journals Healthcare free medical journals Healthcare famous journals Healthcare Google Scholar indexed journals Antibiotics articles Antibiotics Research articles Antibiotics review articles Antibiotics PubMed articles Antibiotics PubMed Central articles Antibiotics 2023 articles Antibiotics 2024 articles Antibiotics Scopus articles Antibiotics impact factor journals Antibiotics Scopus journals Antibiotics PubMed journals Antibiotics medical journals Antibiotics free journals Antibiotics best journals Antibiotics top journals Antibiotics free medical journals Antibiotics famous journals Antibiotics Google Scholar indexed journals Non-operative treatment articles Non-operative treatment Research articles Non-operative treatment review articles Non-operative treatment PubMed articles Non-operative treatment PubMed Central articles Non-operative treatment 2023 articles Non-operative treatment 2024 articles Non-operative treatment Scopus articles Non-operative treatment impact factor journals Non-operative treatment Scopus journals Non-operative treatment PubMed journals Non-operative treatment medical journals Non-operative treatment free journals Non-operative treatment best journals Non-operative treatment top journals Non-operative treatment free medical journals Non-operative treatment famous journals Non-operative treatment Google Scholar indexed journals Neutrophilia articles Neutrophilia Research articles Neutrophilia review articles Neutrophilia PubMed articles Neutrophilia PubMed Central articles Neutrophilia 2023 articles Neutrophilia 2024 articles Neutrophilia Scopus articles Neutrophilia impact factor journals Neutrophilia Scopus journals Neutrophilia PubMed journals Neutrophilia medical journals Neutrophilia free journals Neutrophilia best journals Neutrophilia top journals Neutrophilia free medical journals Neutrophilia famous journals Neutrophilia Google Scholar indexed journals Leukocytosis articles Leukocytosis Research articles Leukocytosis review articles Leukocytosis PubMed articles Leukocytosis PubMed Central articles Leukocytosis 2023 articles Leukocytosis 2024 articles Leukocytosis Scopus articles Leukocytosis impact factor journals Leukocytosis Scopus journals Leukocytosis PubMed journals Leukocytosis medical journals Leukocytosis free journals Leukocytosis best journals Leukocytosis top journals Leukocytosis free medical journals Leukocytosis famous journals Leukocytosis Google Scholar indexed journals Visual Analog Scale articles Visual Analog Scale Research articles Visual Analog Scale review articles Visual Analog Scale PubMed articles Visual Analog Scale PubMed Central articles Visual Analog Scale 2023 articles Visual Analog Scale 2024 articles Visual Analog Scale Scopus articles Visual Analog Scale impact factor journals Visual Analog Scale Scopus journals Visual Analog Scale PubMed journals Visual Analog Scale medical journals Visual Analog Scale free journals Visual Analog Scale best journals Visual Analog Scale top journals Visual Analog Scale free medical journals Visual Analog Scale famous journals Visual Analog Scale Google Scholar indexed journals Anorexia articles Anorexia Research articles Anorexia review articles Anorexia PubMed articles Anorexia PubMed Central articles Anorexia 2023 articles Anorexia 2024 articles Anorexia Scopus articles Anorexia impact factor journals Anorexia Scopus journals Anorexia PubMed journals Anorexia medical journals Anorexia free journals Anorexia best journals Anorexia top journals Anorexia free medical journals Anorexia famous journals Anorexia Google Scholar indexed journals Diarrhea articles Diarrhea Research articles Diarrhea review articles Diarrhea PubMed articles Diarrhea PubMed Central articles Diarrhea 2023 articles Diarrhea 2024 articles Diarrhea Scopus articles Diarrhea impact factor journals Diarrhea Scopus journals Diarrhea PubMed journals Diarrhea medical journals Diarrhea free journals Diarrhea best journals Diarrhea top journals Diarrhea free medical journals Diarrhea famous journals Diarrhea Google Scholar indexed journals Intravenous antibiotic therapy articles Intravenous antibiotic therapy Research articles Intravenous antibiotic therapy review articles Intravenous antibiotic therapy PubMed articles Intravenous antibiotic therapy PubMed Central articles Intravenous antibiotic therapy 2023 articles Intravenous antibiotic therapy 2024 articles Intravenous antibiotic therapy Scopus articles Intravenous antibiotic therapy impact factor journals Intravenous antibiotic therapy Scopus journals Intravenous antibiotic therapy PubMed journals Intravenous antibiotic therapy medical journals Intravenous antibiotic therapy free journals Intravenous antibiotic therapy best journals Intravenous antibiotic therapy top journals Intravenous antibiotic therapy free medical journals Intravenous antibiotic therapy famous journals Intravenous antibiotic therapy Google Scholar indexed journals
Article Details
1. Introduction
Appendicitis is a prevalent condition among pediatric patients, requiring prompt intervention to prevent potential complications [1-8]. The likelihood of developing appendicitis over a lifetime is approximately 7-8%, with the highest occurrence during the teenage years [2]. While appendectomy has traditionally been the primary treatment for acute appendicitis since its introduction by McBurney in 1889 [4], recent medical literature and evolving clinical practices have prompted a reevaluation of this conventional approach [8]. Surgical appendectomy has long been considered the gold standard for treating uncomplicated pediatric appendicitis [6]. Despite being generally perceived as a straightforward procedure, it involves general anesthesia and abdominal operation and carries inherent risks and potential complications. Complications related to surgery or anaesthesia occurs in over 10% of children within 30 days of appendectomy [7]. The emergence of non-operative interventions, such as antibiotic therapy and observational management, reflects a shift towards more conservative and patient-centred approaches [9]. The reconsideration of surgical intervention is underscored by its impact on patient outcomes, healthcare costs, and the overall experience for patients and their families [10]. The advent of laparoscopic surgery and the low threshold for operative intervention have led to a risk of high negative appendicectomy rates with unnecessary surgery-related morbidity [11,12]. Approximately 20% of patients present with complicated appendicitis, prompting exploration of non-operative approaches for early uncomplicated cases, often resulting in resolution [13,14]. While historically, antibiotics were seen as a prelude to surgery for suspected appendicitis, recent findings indicate that antibiotics can be a safe primary treatment for acute uncomplicated appendicitis [15]. Varadhan et al. (2012) concluded from their meta-analysis that antibiotics can be used safely as the primary treatment in patients presenting with acute uncomplicated appendicitis, with a 63% response rate to non-operative treatment [16]. Although the literature on non-operative treatment in children is limited, a recent systematic review and meta-analysis demonstrated that non-operative treatment is effective as the initial approach in 97% of cases of acute uncomplicated appendicitis in children [17]. This approach may offer social and economic benefits, reducing the time away from normal daily activities for children and families, including schooling and parental time off work. However, the issue of recurrent appendicitis arises as successful non-operative treatment leaves children with an appendix and a risk of recurrence.
2. Methodology and Materials
This was a prospective observational study. This study was conducted from July 2017 to March 2019 at the Department of Pediatric Surgery, Dhaka Medical College Hospital, Dhaka, Bangladesh. All patients were admitted with uncomplicated acute appendicitis in the Department of Pediatric surgery. After explaining the study objectives, purpose and potential risks of the procedure in details, informed written consent was collected from the patient’s guardian. Detailed history, clinical examination, and all information were taken in a predesigned dully pretested data collection form. Prior to the commencement of this study, the research protocol was approved by the Institutional Review Board (IRB) of DMCH, Dhaka.
Inclusion criteria:
- Patients of uncomplicated acute appendicitis
- Age up to 12 years in both sexes
Exclusion criteria:
- Patients of age >12years
- Patients with obstructed appendicitis- appendicitis with fecalith
- Patients with perforated appendix
- Patients with appendicular lump/abscess
2.1 Study procedure:
A questionnaire was prepared by the researcher considering key variables like age, sex, presenting complains, clinical findings, associated medical conditions, investigations, antibiotic and doses. The data were collected by researcher himself. The aims, objectives, procedures, risks and benefits of operation were explained to the gurdian of the selected patients. The patients were encouraged for voluntary participation. They were also assured about the secrecy of information and records. Then written informed consent was taken from each patient/parent. Then a conservative treatment started with admitted uncomplicated acute appendicitis patient combination by inj. ceftriaxone (100mg/kg/ day), inj. metronidazol (1.5mg/kg/tds) and inj. amikacin (7.5mg/kg/bd) therapy for five days with associated supportive management. The patients were assessed after 24 hours of treatment, who responded on above treatment continued same treatment at least five days then discharged and followed up and investigation (CBC, Ultrasonogram of whole abdomen) were done after 15 days, 1 month, 3 months and 6 months. Above all other necessary information was taken. Demographic and clinical information were recorded.
2.2 Data collection and analysis:
Data collection procedure: After management patients were followed up after 15days, 1 month, 3 months and 6 months. Evaluation was performed by clinical examination, blood investigation and sonological test. All the data was checked and edited after collection. Then the data was entered into computer and statistical analysis of the results was obtained by using windows-based computer software Statistical Packages for Social Sciences (SPSS-22) (SPSS Inc, Chicago, IL, USA). The results were presented in tables and figures. Statistical significance was set at p<0.05 and confidence interval set at 95% level. Continuous variables were expressed as mean with standard deviation and categorical variables as frequency with percentage.
3. Result
Table 1 shows the age distribution of the study population (N=62), revealing a diverse representation, with a mean age of 8.95±2.10 years. Notably, the majority falls within the 6-10 years range (45.2%), followed by 11-12 years (41.9%), and 4-6 years (12.9%). This distribution highlights the concentration of subjects in the middle childhood years. Figure 1 illustrates that the gender distribution in the study population demonstrates a predominance of males, constituting 61.3%, while females account for 38.7%. This imbalance suggests a potential gender-related factor that may influence the study's findings, warranting further exploration or consideration in the analysis and interpretation of results. Table 2 provides an overview of the clinical findings and symptoms in the study population. Noteworthy observations include a high prevalence of anorexia (80.65%), fever exceeding 38? C (80.65%), and triage as acute abdomen (83.87%). Additionally, nausea/vomiting (64.52%), RLQ tenderness (64.52%), neutrophilia (74.19%), and leukocytosis (59.68%) are common, indicating a range of symptoms and clinical markers associated with the studied pediatric appendicitis cases. Table 3 presents the pain measurements of the study population based on the Visual Analog Scale (VAS). The mean pain scores decrease progressively over time, indicating a substantial reduction in pain from the first to the fifth-day post-intervention. Specifically, the mean pain scores are 9.42±0.92 on the first day, 7.13±1.00 on the second day, 4.77±0.98 on the third day, and a notable decrease to 0.77±0.98 on the fifth day. This suggests an effective and improving trend in pain management throughout the study period. Table 4 outlines the observations of the appendix diameter in the study population over time. The mean diameter decreases progressively, suggesting a reduction in inflammation and swelling. Specifically, the mean appendix diameter is 6.97±0.36 mm at admission, decreasing to 5.71±0.82 mm at day 15, 5.55±0.67 mm at day 30, and further diminishing to 5.05±0.76 mm at 3 months. This trend indicates a positive response to treatment and resolution of inflammation in the appendix. Table 5 provides insights into the patients' observation and treatment durations. The median observation period after initial treatment is 16 months, ranging from 12 to 18 months. Patients experienced a median duration of 22 hours of pain before hospitalization, with a range of 12 to 24 hours. The time from symptoms to management has a median of 24 hours, ranging from 15 to 28 hours. Hospitalization duration has a median of 84 hours, ranging from 72 to 126 hours. Additionally, the duration of antibiotic treatment (both intravenous and oral) averages 5.26±0.63 days, providing insight into the length of antimicrobial therapy administered to the study population. Figure 2 indicates that most patients (95.1%) in the study population experienced successful conservative treatment. Conversely, a small percentage (4.9%) had unsuccessful conservative treatment. This suggests that the conservative approach, as opposed to immediate surgery, was effective in a majority of cases for managing uncomplicated pediatric appendicitis in the studied population.
|
Age (years) |
Frequency (n) |
Percentage (%) |
|
45447 |
8 |
12.9 |
|
45571 |
28 |
45.2 |
|
45637 |
26 |
41.9 |
|
Mean±SD |
8.95±2.10 |
|
Table 1: Age distribution of the study population (N=62).
|
Finding |
Frequency (n) |
Percentage (%) |
|
Nausea/vomiting |
40 |
64.52 |
|
Anorexia |
50 |
80.65 |
|
Fever > 38°C |
50 |
80.65 |
|
Migration of pain |
25 |
40.32 |
|
Leukocytosis |
37 |
59.68 |
|
Neutrophilia |
46 |
74.19 |
|
RLQ tenderness |
40 |
64.52 |
|
Hopping/percussion/coughing |
31 |
50 |
|
Triaged as acute abdomen |
52 |
83.87 |
|
Diarrhea |
12 |
19.35 |
|
UTI symptoms |
6 |
9.68 |
Table 2: Clinical findings and symptoms.
|
Pain (VAS) |
Mean±SD |
Range |
|
1st day |
9.42 ± 0.92 |
8.00-10.00 |
|
2nd day |
7.13 ± 1.00 |
6.00-8.00 |
|
3rd day |
4.77 ± 0.98 |
4.00-6.00 |
|
5th day |
0.77 ± 0.98 |
0.00-2.00 |
Table 3: Pain measurement of the study population based on VAS.
|
Diameter of appendix (mm) |
Mean±SD |
Range |
|
At admission |
6.97 ± 0.36 |
6.10-7.50 |
|
At day 15 |
5.71 ± 0.82 |
0.20-7.10 |
|
At day 30 |
5.55 ± 0.67 |
4.20-7.40 |
|
At 3 months |
5.05±0.76 |
3.60-7.00 |
Table 4: Observation of appendix diameter.
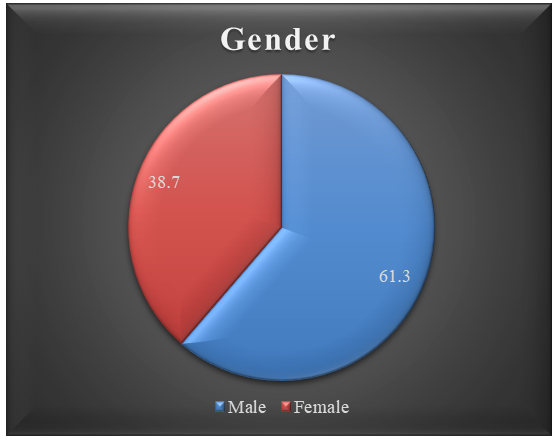
Figure 1: Gender distribution of the study population (N=62).
|
Observation |
Median |
Range |
|
Observation period after initial treatment (months) |
16 |
(12-18) |
|
Duration of pain before hospitalization (h) |
22 |
(12-24) |
|
Time from symptoms to management (h) |
24 |
(15-28) |
|
Hospitalization (h) |
84 |
(72-126) |
|
Duration of antibiotic treatment (IV and Oral) (days) |
5.26 ± 0.63 |
|
Table 5: Patients observation and treatments duration.
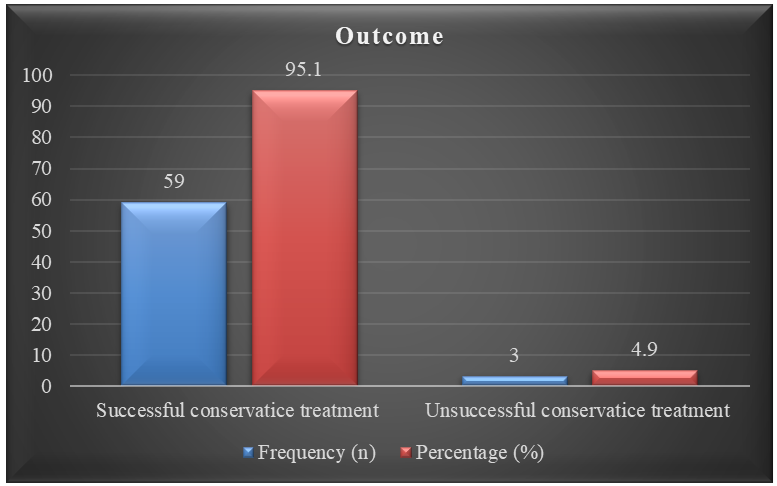
Figure 2: Outcome of the study (N=62).
4. Discussion
In recent years, numerous studies have investigated alternative approaches to treating acute uncomplicated appendicitis in children through conservative methods. A UK feasibility trial randomized children based on a clinical presentation for suspected acute uncomplicated appendicitis, demonstrating that conservative treatment is safe and feasible. This development could open avenues for future randomized controlled trials (RCTs). Despite efforts to enroll only children with uncomplicated appendicitis, only 4.9% of those allocated for appendectomy in the study had complicated appendicitis. Of the 62 children initially assigned to nonoperative treatment, 95.1% did not undergo appendectomy by the end of the follow-up period, aligning with findings in a study by Stenier et al. in 2017 [18]. The study on conservative antibiotic therapy for uncomplicated acute appendicitis in children, with a mean age of 8.95±2.10 years, predominantly male (male-to-female ratio 1.6:1), echoed results from Bachur et al. [19], with a median age of 11.4 years and a male-to-female ratio of 1.5:1 [19]. Maini et al. [20] reported a mean age of 13.3 years and a male-to-female ratio of 2:1, showing slight variations. Abdominal pain was the primary complaint in 83.47% of cases, leading to triage as acute abdomen, while fever and anorexia were more common in severe appendicitis cases [21]. The mean diameter of the uncomplicated acute appendix at admission was 6.97±0.36 mm, aligning with findings from another study [22]. Analyzing 62 children eligible for conservative treatment and long-term follow-up, the study revealed that 95.1% of children with uncomplicated appendicitis were successfully managed with conservative treatment, including IV antibiotic treatment for 3-5 days, oral antibiotics for 5 days, and a median follow-up of 18 months. This outcome is consistent with Stenier's 2017 study [19]. Recognizing the frequent misdiagnosis of appendicitis and the associated unnecessary appendectomies, the study aimed to explore alternatives. Complications during conservative therapy were observed in 3 cases (4.9%), contrasting with an 11.9% complication rate in Maini et al.'s 2017 study [21]. Two patients (5.0%) required surgery after 12 and 24 hours, as reported by Malik and Bari in 2009 [23]. Styrud et al. [24] noted that only 12% of patients in the antibiotic treatment group underwent surgery within 24 hours [24]. The study suggests that antibiotics can successfully treat acute appendicitis, leading to a short hospital stay, minimal sick leave, and limited pain duration.
5. Limitations of the Study
Despite the valuable insights provided by this study on the effectiveness of conservative treatment for pediatric uncomplicated appendicitis, certain limitations should be acknowledged. Firstly, the study's sample size of 62 patients may limit the generalizability of findings to a broader population. Additionally, the single-centre nature of the study may introduce geographical and demographic biases. The exclusion of patients with obstructed appendicitis, perforated appendix, or appendicular lump/abscess may restrict the applicability of results to a specific subset of pediatric appendicitis cases. Moreover, the relatively short follow-up period of 18 months raises questions about the long-term efficacy and recurrence rates of conservative treatment. Further multicenter studies with larger and more diverse cohorts, extended follow-up periods, and consideration of a broader range of appendicitis presentations are warranted to enhance the robustness and external validity of the findings.
6. Conclusion and Recommendations
In conclusion, our prospective observational study demonstrates that conservative management, including intravenous antibiotic therapy followed by oral antibiotics, is a viable and effective approach for uncomplicated pediatric appendicitis. The majority of cases (95.1%) showed successful resolution without the need for surgical intervention. Our findings highlight the potential benefits of this non-operative strategy, such as shorter hospital stays, reduced pain duration, and limited disruption to daily activities for children and their families. Recommendations for future research include conducting randomized controlled trials to further validate the efficacy and safety of conservative management compared to traditional surgical appendectomy in pediatric patients with uncomplicated appendicitis. Additionally, exploring the long-term outcomes, including the risk of recurrent appendicitis and potential complications, will contribute to a more comprehensive understanding of non-operative approaches. As the medical community reevaluates treatment paradigms, our study supports considering conservative management as a primary option for uncomplicated pediatric appendicitis, emphasizing its potential benefits regarding healthcare resource utilization and patient well-being. However, research and consensus within the medical community are warranted before the widespread adoption of non-operative strategies in routine clinical practice.
Funding:
No funding sources.
Conflict of interest:
None declared.
References
- Peter SD, Sharp SW, Holcomb III GW, et al. An evidence-based definition for perforated appendicitis derived from a prospective randomized trial. Journal of Pediatric Surgery 43 (2008): 2242-2245.
- Rashid MS, Islam KM, Alam MM, et al. Evaluation of Necessity of Appendectomy after Conservative Treatment of Uncomplicated Acute Appendicitis in Children. Annals of International Medical and Dental Research (AIMDR) 8 (2022): 206-215.
- Moris D, Paulson EK, Pappas TN. Diagnosis and management of acute appendicitis in adults: A review. Jama 326 (2021): 2299-2311.
- McBurney CM. Experience with early operative interference in cases of disease of the vermiform appendix. Ny state med J 50 (1889): 676-684.
- Thomas M. Infiltration of Appendix with Eosinophils in Acute Appendicitis (Doctoral dissertation, Rajiv Gandhi University of Health Sciences (India)).
- Hall NJ, Eaton S, Abbo O, et al. Appendectomy versus non-operative treatment for acute uncomplicated appendicitis in children: study protocol for a multicentre, open-label, non-inferiority, randomised controlled trial. BMJ Paediatrics Open 1 (2017).
- Tiboni S, Bhangu A, Hall NJ, et al. Outcome of appendicectomy in children performed in paediatric surgery units compared with general surgery units. Journal of British Surgery 101 (2014): 707-714.
- Ilves I. Epidemiological and clinical studies of acute appendicitis (Doctoral dissertation, Itä-Suomen yliopisto) (2017).
- Podda M, Di Saverio S, Cillara N, et al. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis: Time to change the goal of our research?. International Journal of Surgery 48 (2017): 264-265.
- Carrera PM, Kantarjian HM, Blinder VS. The financial burden and distress of patients with cancer: understanding and stepping?up action on the financial toxicity of cancer treatment. CA: A cancer journal for clinicians 68 (2018): 153-165.
- Coursey CA, Nelson RC, Patel MB, et al. Making the diagnosis of acute appendicitis: do more preoperative CT scans mean fewer negative appendectomies? A 10-year study. Radiology 254 (2010): 460-468.
- Ming PC, Yan TY, Tat LH. Risk factors of postoperative infections in adults with complicated appendicitis. Surgical Laparoscopy Endoscopy & Percutaneous Techniques 19 (2009): 244-248.
- Coldrey EJ. Five years of conservative treatment of acute appendicitis. J Int Coll Surg 32 (1959): 255-261.
- Campbell MR, Johnston III SL, Marshburn T, et al. Nonoperative treatment of suspected appendicitis in remote medical care environments: Implications for future spaceflight medical care1. Journal of the American College of Surgeons 198 (2004): 822-830.
- Varadhan KK, Humes DJ, Neal KR, et al. Antibiotic therapy versus appendectomy for acute appendicitis: a meta-analysis. World Journal of Surgery 34 (2010): 199-209.
- Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. Bmj 5 (2012): 344.
- Georgiou R, Eaton S, Stanton MP, Pierro A, Hall NJ. Efficacy and safety of nonoperative treatment for acute appendicitis: a meta-analysis. Pediatrics 139 (2017): e20163003.
- Steiner Z, Buklan G, Stackievicz R, et al. Conservative treatment in uncomplicated acute appendicitis: reassessment of practice safety. European Journal of Pediatrics 176 (2017): 521-527.
- Bachur RG, Lipsett SC, Monuteaux MC. Outcomes of nonoperative management of uncomplicated appendicitis. Pediatrics 140 (2017).
- Maini SK, Jain NK, Jain MG, et al. Conservative management of early uncomplicated appendicitis in children. International Surgery Journal 4 (2017): 1024-1027.
- ML N. Appendicitis in the young child: A continuing diagnotic challenge. Pediatr Emerg Care 16 (2000): 160-162.
- Park HC, Kim BS, Lee BH. Efficacy of short-term antibiotic therapy for consecutive patients with mild appendicitis. The American surgeon 77 (2011): 752-755.
- Malik AA, Bari SU. Retracted article: conservative management of acute appendicitis. Journal of Gastrointestinal Surgery 13 (2009): 966-970.
- Styrud J, Eriksson S, Nilsson I, et al. Appendectomy versus antibiotic treatment in acute appendicitis. a prospective multicenter randomized controlled trial. World Journal of Surgery 30 (2006): 1033-1037.


 Impact Factor: * 3.8
Impact Factor: * 3.8 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 