Juvenile Dermatomyositis: Case Report from the Albert Royer National Children's Centre in Dakar (Senegal)
Article Information
Yaay Joor Koddu Biigé DIENG1*, Amadou SOW2, Djénaba Fafa CISSE3, Fatime TALL1, Idrissa Demba BA1, Papa Moctar FAYE1, Ousmane NDIAYE1
Affiliation:
1National Children's Hospital Albert Royer, Dakar, Senegal
2Abass Ndao Hospital, Dakar, Senegal
3Pikine National Hospital, Dakar, Senegal
*Corresponding author:Yaay Joor Koddu Biigé DIENG, National Children's Hospital Albert Royer, Dakar.
Received: January 15, 2024;Accepted: January 20, 2024;Published: February 07, 2024
Citation: Yaay Joor Koddu Biigé DIENG, Amadou SOW, Djénaba Fafa CISSE, Fatime TALL, Idrissa Demba BA, Papa Moctar FAYE, Ousmane NDIAYE. Juvenile Dermatomyositis: Case Report from the Albert Royer National Children's Centre in Dakar (Senegal). Journal of Pediatrics, Perinatology and Child Health. 8 (2024): 15-18.
View / Download Pdf Share at FacebookAbstract
Juvenile dermatomyositis (JD) is a rare multi-systemic inflammatory idiopathic disease characterised by primary cutaneous and muscular involvement. There is a paucity of literature concerning children. We report the case of a 7-year-old girl. The diagnosis was made following hospitalisation for respiratory distress with a fever of 39°C and deterioration in general condition with general muscle wasting and relative functional impotence. Examination revealed flaccid quadriplegia, significant muscular amyotrophy and ankylosis with pain on mobilisation of the joints. Hypochromic macules associated with Gottron papules were also found. Biochemistry revealed elevated muscle enzymes and LDH. EMG revealed myogenic patterns and muscle biopsy revealed inflammatory infiltrates in the endomysium and connective tissue. Treatment included prednisone, methotrexate and folic acid. The short- and medium-term outcome was favourable. Death occurred 20 months later at home from an unclear cause.
Keywords
Dermatomyositis; Child; Diagnosis; Evolution
Article Details
Introduction
Juvenile dermatomyositis (JD) is a multi-systemic inflammatory idiopathic disease characterised by primary involvement of the skin (rash) and proximal muscles [1]. It is a diffuse idiopathic vasculopathy of the skin and muscles, uncommon in children, characterised by proximal muscle weakness and a typical skin rash that belongs to the group of inflammatory myositis [1,2]. Diagnosis is based on a set of five criteria established by BOHAN and PETER in 1975 [3,4] and reported in Table 1.
In our developing country context, diagnosis is often delayed and treatment is often limited by the lack of availability of these therapies in cases of corticoresistance. In paediatrics, there is little literature on this subject. We report the clinical case of a 7-year-old girl with DMJ diagnosed at the National Children's Hospital Albert Royer in Dakar. The aim was to describe the epidemiological, diagnostic, therapeutic and evolutionary aspects of DMJ in the Senegalese paediatric setting.
Observation
The patient was a 7-year-old girl admitted to hospital with respiratory distress and a fever of 39°C, in a context of altered general condition (AEG) and generalised muscle weakness. The symptoms dated back 6 months before this consultation and were marked by abnormal tiredness on returning home from school. This was gradually followed by exertional dyspnoea and an inability to climb stairs. This was followed by a rash around certain joints
Table 1: BOHAN and PETER diagnostic criteria for polymyositis and juvenile dermatomyositis (JD) [4].
|
Criteria |
Description |
| A |
Proximal and symmetrical muscle weakness of the pelvic and scapular girdle, anterior flexors of the neck, progressing for weeks to months, with or without dysphagia or involvement of respiratory muscles |
|
B |
Elevation of the serum levels of skeletal muscle enzymes: creatine kinase, aspartate aminotransferase, lactate dehydrogenase and aldolase |
|
C |
Electromyography characteristic of myopathy (short and small motor units, fibrillation, positive pointy waves, insertional irritability and repetitive high-frequency firing) |
|
D |
Muscle biopsy showing necrosis, phagocytosis, regeneration, perifascicular atrophy, perivascular inflammatory exudate |
|
E |
Typical cutaneous changes: 1) Heliotrope rash with periorbital oedema and violaceous erythema 2) Gottron's sign: vasculitis in the elbow, metacarpophalangeal and proximal interphalangeal joints |
|
Polymyositis |
1) Definite - all of A−D 2) Probable - any three of A−D 3) Possible - any two of A−D |
|
Dermatomyositis |
1) Definite - E plus and three of A−D 2) Probable - E plus and two of AD 3) Possible - E plus and one of A−D |
(interphalangeal, elbow and knee), on the forehead and the back of the neck; all this occurred against a backdrop of low-grade fever, physical asthenia and widespread muscle pain with arthralgia. The parents consulted a traditional practitioner, where a topical treatment was prescribed without success. The patient was initially admitted to hospital with the diagnosis of inflammatory myopathy, and a course of corticosteroids based on prednisone 20mg/day was started. However, the patient was lost to follow-up after 2 months.
She had good psychomotor development and attended primary schools. Her parents reported that she had been hospitalised at the age of 3 for respiratory distress of unspecified aetiology. She was the second of six siblings, the others of whom were alive and in apparent good health. There was no consanguinity or known family defect. The socio- economic level was low.
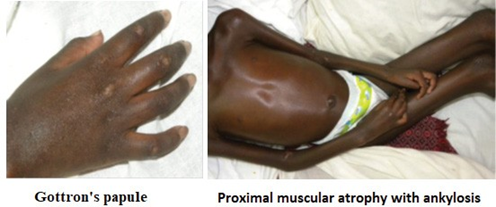
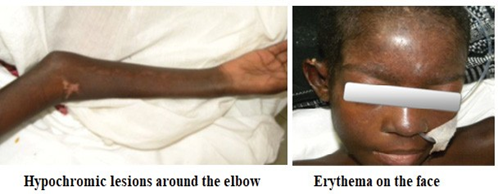
Two months after voluntary discontinuation of treatment, the patient was readmitted to hospital with a worsening of the picture and the appearance of global dysphagia and absolute functional impotence. The physical examination revealed severe malnutrition (BMI 11.42), fever at 39°C, polypnoea with condensation syndrome on the left, reduced cough reflex and desaturation of 93% in ambient air. Neuromuscular examination revealed a flaccid quadriplegia with reduced osteotendinous reflexes, significant muscle amyotrophy with ankylosis associated with pain on passive mobilisation of the joints. Consciousness was clear and there were no Babinski signs. Examination of the skin and skin appendages revealed Gottron papules (erythematous scaly lesions opposite the metacarpal and phalangeal joints) (Figure 1) and symmetrical hypochromic scaling macules located on the face, neck and joints (Figure 2). The rest of the physical examination was normal.
Paraclinical findings included a non-specific inflammatory syndrome (hyperleukocytosis, positive C-reactive protein (CRP) and increased sedimentation rate) with elevated muscle enzymes: CPK= 1612 IU/L (N = 30-200), membrane CPK = 169 IU/L (N < 24) with elevated LDH at 1240 IU/L (N = 120
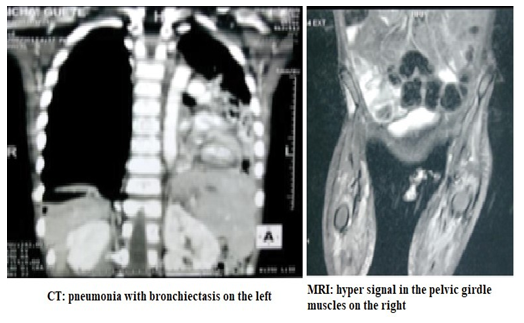
-320). Serum protein electrophoresis showed hyperalpha and gamma globulinaemia. Anti-native DNA, anti-Sm, anti-SSb and anti-phospholipid antibodies were negative. Rheumatoid factor was negative. HIV serology and tuberculosis work- up (IDRT, gastric tube, Genexpert) were negative. Chest X-ray and CT scan showed left-sided pneumonia with bronchiectasis. Magnetic resonance imaging (MRI) showed a hyper-signal in the pelvic girdle muscles (Figure 3).
Electromyography (EMG) revealed myogenic patterns in the muscles of the upper and lower limbs strongly suggestive of generalised myopathy. Muscle biopsy showed inflammatory infiltrates in the endomysium and connective tissue, made up of small lymphocytes, which appeared to be associated with a few macrophages. These infiltrates are predominantly perivascular, and sometimes diffuse in the
endomysium without penetrating the muscle fibres.
In terms of treatment, corticosteroid therapy was continued with prednisone 2mg/kg in addition to nutritional management and other symptomatic and supportive treatment. After a month of corticosteroid therapy, the patient showed no improvement and was given daily boluses of methyl prednisolone 15mg/m2 body surface area for 3 days, methotrexate 10mg/week and folic acid 1mg/day. Given the clinical improvement, multidisciplinary outpatient follow- up (paediatrics, dermatology and neurology) was proposed. The long-term outcome was marked by death at home at the age of 9 due to cardiorespiratory arrest, the cause of which remains unclear.
Discussion
JMD is a rare multisystem inflammatory disease. The overall incidence in children is estimated at 0.8 to 4.1 cases per million children each year [1-4]. In Senegal, studies of dermatomyositis have focused on adult patients, with Diallo et al. [5] reporting 17 cases and Dieng et al. [6] reporting 56 cases. DMJ affects more girls than boys and the average age described in the literature is around 7 years [7]. These data corroborate our patient, who is the first known paediatric case described in Senegal. The most common clinical manifestations of DMJ are proximal muscle involvement, Gottron's papules, skin ulcerations, oedema, fever, asthenia, myalgias, arthralgias/arthritis, dysphagia and skin ulcerations [8,9]. Cutaneous signs may reveal the disease in 50% of cases [9]. In our patient, the main reason for consultation was muscular involvement with increasing functional impotence. Our study shows the important contribution of EMG and muscle enzyme assays in orienting the diagnosis, given the poor availability of anatomopathological studies, often performed outside the country (France), as in our patient's case. In terms of treatment, our patient benefited from multidisciplinary follow-up (paediatrics, neurology, dermatology, physiotherapy). Immunosuppressive drugs (methotrexate, ciclosporin A, azathioprine) may be indicated as a second-line treatment in cases refractory to corticosteroid therapy. In our case, methotrexate was indicated because the disease did not progress favourably on corticosteroids alone. The case fatality rate in developed countries is low (< 1%) [8,9], compared with 11% in India [10]. The difference in mortality can be explained by a more advanced technical platform and early diagnosis. In our patient, the delay in diagnosis was due to wandering during consultations with traditional healers, but also to the limited technical resources; none of the specific tests for DMJ were available in the country. Death at home after 9 months of multidisciplinary follow-up could have been due to sepsis, a dietary error or the side-effects of corticosteroid therapy in a context of poverty and financial deprivation that often prevented emergency consultation in the event of complications due to a lack of financial resources.
Conclusion
DMJ is a rare and under-diagnosed disease in developing countries. The existence of a cutaneous picture associated with a motor deficit should make us think of the diagnosis in children.
Conflict of interests: None.
References
- Symmons DP, Sills JA, Davis The incidence of juvenile dermatomyositis: results from a nation-wide study. Br J Rheumatol 34 (1995): 732-736.
- Medsger TA Jr, Dawson WN Jr, Masi The epidemiology of polymyositis. Am J Med 48 (1970): 715- 723.
- Bohan A, Peter Polymyositis and dermatomyositis (first of two parts). N Engl J Med 292 (1975): 344-347.
- Bohan A, Peter JB. Polymyositis and dermatomyositis (second of two parts). N Engl J Med 292 (1975): 403-407.
- Diallo M, Fall AK, Diallo I, et al. Dermatomyosites et polymyosites : 21 cas au Sénégal. Med Trop 70 (2010): 166-168.
- Dieng MT, Diallo M, Dia D, et al. Dermatomyositis in Study of 56 cases. Dak med 50 (2005): 123-127.
- Khelifa E, Benmously R, Fenniche S, et Epidemioclinical aspects of dermatomyositis in the region of Tunis. Tunis Med 85 (2007): 655-658.
- McCann LJ, Juggins Maillard SM, et al. The juvenile Dermatomyositis National Registry and Repository (UK and Ireland) clinical characteristics of children recruited within the first 5 yr. Rheumatology (Oxford) 45 (2006): 1255-1260.
- Pachman Juvenile dermatomyositis. In Chernick V, Boat TF, Wilmott RW, Bush A Kendig’s disorders of respiratory tract in children. 7th edition. Philadelphia : WB Saunders –Elsevier (2007): 1019-1024.
- Singh S, Bansal A. Twelve years’ experience of juvenile dermatomyositis in North Rheumatol Int 26 (2006): 510-515.


 Impact Factor: * 3.8
Impact Factor: * 3.8 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 