NUSS Procedure in a Patient who had Traumatic Thoracic Aortic Dissection and Thoracolumbar Spine Fracture: A Simple Modification
Article Information
Ikram Ul Haq Chaudhry*, Ahsan Cheema, Chaudhry Aqeel, Yousif A Alqahtani, Zahra Alhaji, Sama M Al Suleiman, Makhdomi KR
Department of Thoracic and vascular surgery, King Fahad Specialist Hospital, Dammam, Saudi Arabia
*Corresponding Author: Ikram Ul Haq Chaudhry, Department of Thoracic and vascular surgery, King Fahad Specialist Hospital, Dammam, Saudi Arabia
Received: 29 July 2020; Accepted: 19 August 2020; Published: 21 August 2020
Citation: Ikram Ul Haq Chaudhry, Ahsan Cheema, Chaudhry Aqeel, Yousif A Alqahtani, Zahra Alhaji, Sama M Al Suleiman, Makhdomi KR. NUSS Procedure in a Patient who had Traumatic Thoracic Aortic Dissection and Thoracolumbar Spine Fracture: A Simple Modification. Journal of Surgery and Research 3 (2020): 272-277.
View / Download Pdf Share at FacebookAbstract
Nuss procedure, also known as minimally invasive repair of pectus excavatum (MIRPE), is a standard practice in modern surgery. Although initially, this procedure was recommended for the younger age group but nowadays, surgeons also practice in the older age group. Due to little modifications of the original Nuss procedure, the complications rate had markedly reduced. We report a case of 21 years male with pectus excavatum who had traumatic thoracic aortic dissection and fracture of the thoracic spine three years before presentation. He came to our hospital to correct pectus excavatum deformity. At the same time, he was refused by other hospitals due to previous aortic dissection treated with endovascular stent and thoracolumbar spines spine fixed with metallic bars. With a simple modification, MIRPE was performed safely, and the patient was discharged for follow up in outpatient with an excellent outcome.
Keywords
Pectus excavatum; MIRPE; Aortic dissection; Spine fracture; Surgery
Pectus excavatum articles, MIRPE articles, Aortic dissection articles, Spine fracture articles, Surgery articles
Pectus excavatum articles Pectus excavatum Research articles Pectus excavatum review articles Pectus excavatum PubMed articles Pectus excavatum PubMed Central articles Pectus excavatum 2023 articles Pectus excavatum 2024 articles Pectus excavatum Scopus articles Pectus excavatum impact factor journals Pectus excavatum Scopus journals Pectus excavatum PubMed journals Pectus excavatum medical journals Pectus excavatum free journals Pectus excavatum best journals Pectus excavatum top journals Pectus excavatum free medical journals Pectus excavatum famous journals Pectus excavatum Google Scholar indexed journals MIRPE articles MIRPE Research articles MIRPE review articles MIRPE PubMed articles MIRPE PubMed Central articles MIRPE 2023 articles MIRPE 2024 articles MIRPE Scopus articles MIRPE impact factor journals MIRPE Scopus journals MIRPE PubMed journals MIRPE medical journals MIRPE free journals MIRPE best journals MIRPE top journals MIRPE free medical journals MIRPE famous journals MIRPE Google Scholar indexed journals Aortic dissection articles Aortic dissection Research articles Aortic dissection review articles Aortic dissection PubMed articles Aortic dissection PubMed Central articles Aortic dissection 2023 articles Aortic dissection 2024 articles Aortic dissection Scopus articles Aortic dissection impact factor journals Aortic dissection Scopus journals Aortic dissection PubMed journals Aortic dissection medical journals Aortic dissection free journals Aortic dissection best journals Aortic dissection top journals Aortic dissection free medical journals Aortic dissection famous journals Aortic dissection Google Scholar indexed journals Spine fracture articles Spine fracture Research articles Spine fracture review articles Spine fracture PubMed articles Spine fracture PubMed Central articles Spine fracture 2023 articles Spine fracture 2024 articles Spine fracture Scopus articles Spine fracture impact factor journals Spine fracture Scopus journals Spine fracture PubMed journals Spine fracture medical journals Spine fracture free journals Spine fracture best journals Spine fracture top journals Spine fracture free medical journals Spine fracture famous journals Spine fracture Google Scholar indexed journals congenital chest wall articles congenital chest wall Research articles congenital chest wall review articles congenital chest wall PubMed articles congenital chest wall PubMed Central articles congenital chest wall 2023 articles congenital chest wall 2024 articles congenital chest wall Scopus articles congenital chest wall impact factor journals congenital chest wall Scopus journals congenital chest wall PubMed journals congenital chest wall medical journals congenital chest wall free journals congenital chest wall best journals congenital chest wall top journals congenital chest wall free medical journals congenital chest wall famous journals congenital chest wall Google Scholar indexed journals urinary catheter articles urinary catheter Research articles urinary catheter review articles urinary catheter PubMed articles urinary catheter PubMed Central articles urinary catheter 2023 articles urinary catheter 2024 articles urinary catheter Scopus articles urinary catheter impact factor journals urinary catheter Scopus journals urinary catheter PubMed journals urinary catheter medical journals urinary catheter free journals urinary catheter best journals urinary catheter top journals urinary catheter free medical journals urinary catheter famous journals urinary catheter Google Scholar indexed journals preoperatively articles preoperatively Research articles preoperatively review articles preoperatively PubMed articles preoperatively PubMed Central articles preoperatively 2023 articles preoperatively 2024 articles preoperatively Scopus articles preoperatively impact factor journals preoperatively Scopus journals preoperatively PubMed journals preoperatively medical journals preoperatively free journals preoperatively best journals preoperatively top journals preoperatively free medical journals preoperatively famous journals preoperatively Google Scholar indexed journals postoperatively articles postoperatively Research articles postoperatively review articles postoperatively PubMed articles postoperatively PubMed Central articles postoperatively 2023 articles postoperatively 2024 articles postoperatively Scopus articles postoperatively impact factor journals postoperatively Scopus journals postoperatively PubMed journals postoperatively medical journals postoperatively free journals postoperatively best journals postoperatively top journals postoperatively free medical journals postoperatively famous journals postoperatively Google Scholar indexed journals traumatic injuries articles traumatic injuries Research articles traumatic injuries review articles traumatic injuries PubMed articles traumatic injuries PubMed Central articles traumatic injuries 2023 articles traumatic injuries 2024 articles traumatic injuries Scopus articles traumatic injuries impact factor journals traumatic injuries Scopus journals traumatic injuries PubMed journals traumatic injuries medical journals traumatic injuries free journals traumatic injuries best journals traumatic injuries top journals traumatic injuries free medical journals traumatic injuries famous journals traumatic injuries Google Scholar indexed journals finger dissection articles finger dissection Research articles finger dissection review articles finger dissection PubMed articles finger dissection PubMed Central articles finger dissection 2023 articles finger dissection 2024 articles finger dissection Scopus articles finger dissection impact factor journals finger dissection Scopus journals finger dissection PubMed journals finger dissection medical journals finger dissection free journals finger dissection best journals finger dissection top journals finger dissection free medical journals finger dissection famous journals finger dissection Google Scholar indexed journals
Article Details
Introduction
The most common congenital chest wall anomaly is pectus excavatum, which is usually diagnosed in infancy. Sauer Bruch, in 1920 performed the first surgery for the correction of pectus excavatum. He resected bilateral costal cartilages and performed sternal osteotomy [1]. In 1940, Ravitch performed the first correction of pectus excavatum based on the same principle [2]. Donald Russ introduced in the late 1980s a new technique for the correction of pectus excavatum called Nuss procedure [3]. Then later on in 1997 at an American pediatric surgery meeting, he presented his technique of MIRPE [4]. Further modification was introduced by Croitoru et al. named as modified Nuss procedure [5].
Case
A 21year-old male known case of pectus excavatum since birth underwent a Road Traffic Accident (RTA) three years ago and sustained thoracic aortic dissection and fracture of the thoracic spine. Aortic dissection was managed with two endovascular stents, and thoracic spines fractures were fixed with screws and rods, He was referred to our hospital for correction of pectus excavatum. CT sac of the thorax showed severe pectus excavatum with a hilar index 4.6. Figure 1(A). Echocardiogram (ECHO) was normal. Our vascular surgeon advised for CT Angiography of chest preoperatively to evaluate the stent position Figure 1(B) Basic blood investigation total blood count, liver and renal panel were within the normal range.
Prior to the induction of general anesthesia patient had an epidural catheter, urinary catheter, an arterial line, and then was intubated using a single-lumen tube. The patient was positioned on the right side of the table in a supine position with both arms in an abducted position. Prophylactic intravenous antibiotics are administered preoperatively and continued for three days postoperatively. We use Tazocin 4.5gm at induction, and three doses postoperatively. As for standard MIRPE, midaxillary points and maximum points close to deformity were marked as shown in Figure 1. At the right lateral side of the chest wall just above the level of the nipples, a small incision is made for placement of a trocar for a 5-mm rigid thoracoscopy to gain optimal view during the whole procedure. The thoracoscope was inserted during apnea, and the deepest point of the pectus excavatum could not be identified because there were dense adhesions. Potential intercostal spaces for bar placement are marked on the skin just medially to the highest point of the deformity on both sides. A template bar was used to determine the optimal bar size and shape, and the bar was shaped accordingly. Incisions were made bilaterally, and a subcutaneous tunnel was created on each side of the chest wall as there were dense adhesions due to previous traumatic injuries we modified the technique. At the highest point, we made the incision and inserted an index finger on each side and dissected medially, so both fingers touch each other and then.
Then introducer was inserted through the incision made on the right side in the midaxillary line. It was passed subcutaneously through the chest wall into the pleural cavity through the intercostal space used for finger dissection. Under the guidance of the thoracoscope, the introducer was carefully passed retrosternal through the anterior mediastinal soft tissue to the left pleural cavity, very carefully in front of the pericardium to the subcutaneously tunneled left side. This maneuver was performed during apnea. The introducer was lifted while pressing down the caudal rib curvatures to reform the chest wall. A ribbon tape was inserted through the eyelet of the introducer, and introducer was retracted. The pectus bar was attached to the ligature and pulled through the tunnel in an upside-down position with the convex side facing the pericardium. The tap was removed. The bar was flipped 180 degrees to the correct location. The flipping was done in a clockwise direction for the surgeon on the right side and counterclockwise for the assistant on the left side of the patient. To avoid cardiac injury. The stabilizer was mounted on each side to stabilize rod, and pins were inserted in stabilizer to prevent Bar rotation in the future. Some surgeons use wires to fix the stabilizer for this purpose. The bar rests on two ribs on the right side, and on the left side, the stabilizer also rests on two ribs, thus ensuring stability and minimizing the risk of stripping the intercostal muscles. Figure 2 The incisions were then closed in 3 layers with a monofilament suture.
Through the camera, port pneumothorax was drained using chest drain in water seal while lungs were inflated and kept in expansion for a few seconds. Patient post-operative recovery was uneventful he was discharged for follow up in outpatient, his pre and post-operative photographs are shown in Figure 3 (A,B&CD).
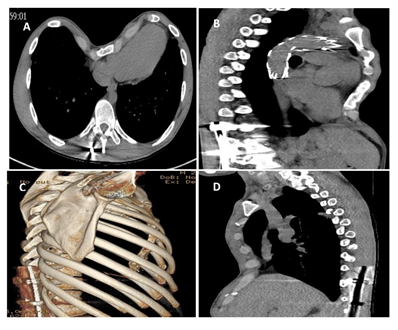
Figure 1: (A) Computed tomogram of the Thorax [Axial] view showing the severity of the Pectus Excavatum. Heller Index: 4.6 (B) Sagittal view showing post traumatic aortic dissection, endovascular stent. (C) 3-D reconstruction of the thoracic scan showing post traumatic thoracolumbar spine fixation with steel rods. (D) Another sagittal view of the thorax showing the severity of chest wall deformity.
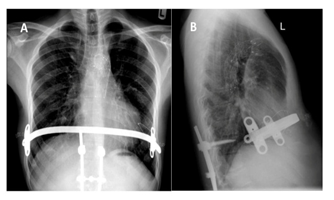
Figure 2: (A) & ( B), Post-operative Chest Radiographs Anterior and Lateral views showing the position of NUSS Bar and thoracolumbar spine fixation and endovascular graft in thoracic aorta.

Figure 3: (A) & (B) Digital photographs of the patient Front & side views prior to the MIRPE. (C) & (D) Digital photographs of the patient Front & side views after the MIRPE. [Informed consent obtained from the patient for publication purpose].
Discussion
There are many methods for remodeling of congenital chest wall deformity pectus excavatum chest wall. Initially, Ravitch and modified Ravitch gained popularity, but with the advent of MIRPE by Nuss, now the Ravitch operation is only used for selective cases.
Historically Ravitch procedure has good results, but its drawbacks are post-operative chest wall growth and instability due to extensive perichondral dissection and resection of abnormal cartilages. Also, it is a long surgical procedure and demands hospitalization for pain management. Physical activity is severely restricted for several months as the costal cartilages slowly grow back together [6]. The ideal age for the MIRPE is between 6-12 years because, in adults, there is more risk of bar displacement. But with the more refinements and new stabilizer, this problem is much resolved. Beatrix et al. did a prospective observational study about NUSS procedure in 129 adult patients between 2002-2014, 87.6% were male, and the median age at surgery was 21, and the media hilar index was 4.8. They reported overall morbidity was 14.7%, the most frequent complication was bar displacement (7%), and 97.6% of patients were satisfied with cosmetic results [7]. Ohno et al. in 2003 also reported that bar displacement is more in adults as compared to younger age group [8]. Colin et al. also reported in favor of NUSS procedure in adults can provide satisfactory results [9]. The Ravitch procedure is much recommended in selective adult patients as this provides reasonable physiologic and cosmetic satisfaction. Surgery of pectus excavatum (PE) is challenging and requires the insertion of a retrosternal metallic bar, which, in turn, demands blunt dissection in the mediastinum. The operation becomes even more taxing when there are adhesions in the chest, as was the case in our patient. The Aortic dissection was treated with Aortic stent-graft. Thirty-three percent of the patients who undergo thoracic aortic stent grafting develop Post Implantation Syndrome (PIS) [10-12], which is a clinical and biochemical expression of the inflammatory response following stent grafting. Apart from other injuries, including paraplegia from the RTA, he had a dissection of his Descending Thoracic Aorta, which was treated with Endovascular Stent Graft. Both the RTA and Stent graft can give rise to adhesions. It is well known that any amount of blood leaked; within or outside the arterial wall is a very strong irritant and causes intense inflammation. There are many series and papers about MIRPE in the medical literature about its efficacy, risks, and benefits in the younger and older age group.
Our patient had a dissection of the thoracic aorta that was treated with a thoracic aortic stent-graft, which causes (PIS), which is an additional cause of aortic wall inflammation. He also had surgery for thoracolumbar spine fractures leading to inflammation and adhesions. MIRPE in this patient was a real challenge, but simple two-finger blunt dissection made this procedure very safe. In conclusion, to the best of our knowledge, this is the first case of MIRPE in a patient with traumatic thoracic aortic dissection and thoracolumbar spine fracture. Using our simple modification technique, MIRPE can be performed safely in patients with thoracic aortic dissection and thoracic spine fracture.
References
- Sarbruch F. Die Chirurgie der Brustorgane. Berlin, Springer 1 (1928): 437
- Ravitch MM. The operative treatment of pectus excavatum. Annals of Surgery 129 (1949): 429.
- Kelly RE, Goretsky MJ, Obermeyer R, et al. Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Annals of Surgery 252 (2010): 1072-1081.
- Nuss D, Kelly Jr RE, Croitoru DP, et al. A 10-year review of a minimally invasive technique for the correction of pectus excavatum. Journal of Pediatric Surgery 33 (1998): 545-552.
- Croitoru DP, Kelly Jr RE, Goretsky MJ, et al. Experience and modification update for the minimally invasive Nuss technique for pectus excavatum repair in 303 patients. Journal of Pediatric Surgery 37 (2002): 437-445.
- Haller Jr JA, Colombani PM, Humphries CT, et al. Chest wall constriction after too extensive and too early operations for pectus excavatum. The Annals of Thoracic Surgery 61 (1996): 1618-1625.
- Hoksch B, Kocher G, Vollmar P, et al. Nuss procedure for pectus excavatum in adults: long-term results in a prospective observational study. European Journal of Cardio-Thoracic Surgery 50 (2016): 934-939.
- Ohno K, Morotomi Y, Ueda M, et al. Comparison of the Nuss procedure for pectus excavatum by age and uncommon complications. Osaka City Medical Journal 49 (2003): 71-76.
- Coln D, Gunning T, Ramsay M, et al. Early experience with the Nuss minimally invasive correction of pectus excavatum in adults. World Journal of Surgery 26 (2002): 1217-1221.
- Arnaoutoglou E, Kouvelos G, Papa N, et al. Prospective evaluation of post-implantation inflammatory response after EVAR for AAA: influence on patients' 30 day outcome. European Journal of Vascular and Endovascular Surgery 49 (2015): 175-183.
- Arnaoutoglou E, Kouvelos G, Koutsoumpelis A, et al. An update on the inflammatory response after endovascular repair for abdominal aortic aneurysm. Mediators of Inflammation (2015).
- Moulakakis KG, Alepaki M, Sfyroeras GS, et al. The impact of endograft type on inflammatory response after endovascular treatment of abdominal aortic aneurysm. Journal of Vascular Surgery 57 (2013): 668-677.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 