Gallbladder- associated ectopic liver tissue: Case Report
Article Information
Mohamad Rakka*, Sorin Cimpean, Pieter Demetter, Ion Surdeanu, Abdelilah Mehdi
Department of General and Digestive Surgery, Iris Hospitals South, Free University of Brussels, Belgium
*Corresponding author: Mohamad Rakka, Department of General and Digestive Surgery, Iris Hospitals South, Free University of Brussels, Belgium
Received: 14 July 2021; Accepted: 20 July 2021; Published: 21 July 2021
Citation: Mohamad Rakka, Sorin Cimpean, Pieter Demetter, Ion Surdeanu, Abdelilah Mehdi. Gallbladder- associated ectopic liver tissue: Case Report. Journal of Surgery and Research 4 (2021): 380-384.
View / Download Pdf Share at FacebookAbstract
Introduction: Ectopic liver tissue is a rare entity. It can be found in various organs of the body but the most common reported location is the gallbladder. The incidence is varying between 0.27% and 0.47%. Most of the cases are asymptomatic and diagnosed intra-operatively or during autopsy. We report a case of Gallbladder-Associated ectopic liver tissue that was encountered during a laparoscopic cholecystectomy.
Case presentation: A 40-year-old female patient was admitted to the hospital for laparoscopic cholecystectomy for symptomatic gallstones, intra-operatively we found an ectopic liver tissue attached to the gallbladder wall. Cholecystectomy was performed and the patient was discharged home the day after surgery in good condition. The histopathological examination of the specimen was confirmed to be an ectopic liver tissue without signs of malignant transformation.
Discussion: Ectopic liver tissue is a rare congenital anomaly. It is defined as the presence of liver tissue outside the native liver. It occurs due to a failure of embryological liver development and it can be found in various organs of the body but the most common reported location is the gallbladder. Ectopic liver tissue is found to be functionally handicapped and more vulnerable to carcinogens and it is strongly associated with the development of hepatocellular carcinoma.
Conclusion: Although it is a rare condition, ectopic liver tissue may pose a challenge to surgeons. When encountered, a surgical excision with histopathological examination is recommended because of its serious complications and the potential risk of malignant transformation.
Keywords
Ectopic liver, Hepatocellular carcinoma, Gallbladder
Ectopic liver articles; Hepatocellular carcinoma articles; Gallbladder articles
Ectopic liver articles Ectopic liver Research articles Ectopic liver review articles Ectopic liver PubMed articles Ectopic liver PubMed Central articles Ectopic liver 2023 articles Ectopic liver 2024 articles Ectopic liver Scopus articles Ectopic liver impact factor journals Ectopic liver Scopus journals Ectopic liver PubMed journals Ectopic liver medical journals Ectopic liver free journals Ectopic liver best journals Ectopic liver top journals Ectopic liver free medical journals Ectopic liver famous journals Ectopic liver Google Scholar indexed journals Hepatocellular carcinoma articles Hepatocellular carcinoma Research articles Hepatocellular carcinoma review articles Hepatocellular carcinoma PubMed articles Hepatocellular carcinoma PubMed Central articles Hepatocellular carcinoma 2023 articles Hepatocellular carcinoma 2024 articles Hepatocellular carcinoma Scopus articles Hepatocellular carcinoma impact factor journals Hepatocellular carcinoma Scopus journals Hepatocellular carcinoma PubMed journals Hepatocellular carcinoma medical journals Hepatocellular carcinoma free journals Hepatocellular carcinoma best journals Hepatocellular carcinoma top journals Hepatocellular carcinoma free medical journals Hepatocellular carcinoma famous journals Hepatocellular carcinoma Google Scholar indexed journals Gallbladder articles Gallbladder Research articles Gallbladder review articles Gallbladder PubMed articles Gallbladder PubMed Central articles Gallbladder 2023 articles Gallbladder 2024 articles Gallbladder Scopus articles Gallbladder impact factor journals Gallbladder Scopus journals Gallbladder PubMed journals Gallbladder medical journals Gallbladder free journals Gallbladder best journals Gallbladder top journals Gallbladder free medical journals Gallbladder famous journals Gallbladder Google Scholar indexed journals abnormal embryological development articles abnormal embryological development Research articles abnormal embryological development review articles abnormal embryological development PubMed articles abnormal embryological development PubMed Central articles abnormal embryological development 2023 articles abnormal embryological development 2024 articles abnormal embryological development Scopus articles abnormal embryological development impact factor journals abnormal embryological development Scopus journals abnormal embryological development PubMed journals abnormal embryological development medical journals abnormal embryological development free journals abnormal embryological development best journals abnormal embryological development top journals abnormal embryological development free medical journals abnormal embryological development famous journals abnormal embryological development Google Scholar indexed journals outpatient clinic articles outpatient clinic Research articles outpatient clinic review articles outpatient clinic PubMed articles outpatient clinic PubMed Central articles outpatient clinic 2023 articles outpatient clinic 2024 articles outpatient clinic Scopus articles outpatient clinic impact factor journals outpatient clinic Scopus journals outpatient clinic PubMed journals outpatient clinic medical journals outpatient clinic free journals outpatient clinic best journals outpatient clinic top journals outpatient clinic free medical journals outpatient clinic famous journals outpatient clinic Google Scholar indexed journals Cholecystectomy articles Cholecystectomy Research articles Cholecystectomy review articles Cholecystectomy PubMed articles Cholecystectomy PubMed Central articles Cholecystectomy 2023 articles Cholecystectomy 2024 articles Cholecystectomy Scopus articles Cholecystectomy impact factor journals Cholecystectomy Scopus journals Cholecystectomy PubMed journals Cholecystectomy medical journals Cholecystectomy free journals Cholecystectomy best journals Cholecystectomy top journals Cholecystectomy free medical journals Cholecystectomy famous journals Cholecystectomy Google Scholar indexed journals malignant transformation articles malignant transformation Research articles malignant transformation review articles malignant transformation PubMed articles malignant transformation PubMed Central articles malignant transformation 2023 articles malignant transformation 2024 articles malignant transformation Scopus articles malignant transformation impact factor journals malignant transformation Scopus journals malignant transformation PubMed journals malignant transformation medical journals malignant transformation free journals malignant transformation best journals malignant transformation top journals malignant transformation free medical journals malignant transformation famous journals malignant transformation Google Scholar indexed journals
Article Details
1. Introduction
Ectopic liver tissue is a rare entity [1]. It occurs due to abnormal embryological development that is represented by the presence of liver tissue outside the native liver. It can be found in various organs of the body but the most common reported location is the gallbladder [2]. Its incidence is varying between 0.27% and 0.47% [3]. To date, the total number of reported cases is 91 cases with the first case reported in 1925 [4,5]. Most of the cases are asymptomatic and are diagnosed at laparoscopy, laparotomy or during an autopsy [6]. Few reported cases are diagnosed preoperatively [7,8]. Herein we report a rare case of gallbladder-associated ectopic liver tissue that was found incidentally during laparoscopic cholecystectomy for symptomatic gallstones and we discuss the presentation, diagnosis and the options of management of this rare entity.
Case 1
A 40-year-old female patient, presented to our outpatient clinic with a 2-month history of recurrent, postprandial right upper quadrant abdominal pain with occasional episodes of nausea. Her past medical history was only remarkable for hypertension. She is nonsmoker, occasionally alcoholic, with no known food and drug allergies. Physical examination revealed a negative Murphy sign. The laboratory evaluations of patient were in normal range. Abdominal ultrasound showed multiple gallstones without evidence of acute cholecystitis. So, the patient was scheduled for laparoscopic cholecystectomy. Intra-operatively, an about 2 cm mass-like liver tissue was encountered. It was attached to the gallbladder wal (Figure 1).
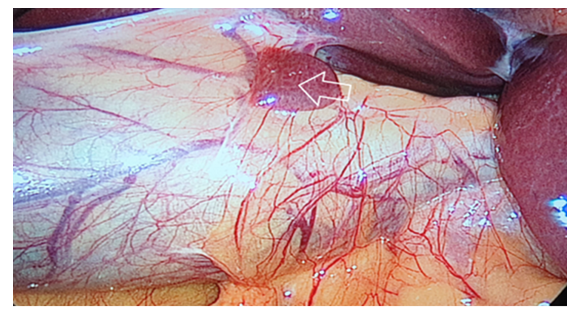
Figure 1: Laparoscopic view of gallbladder-associated ectopic liver tissue
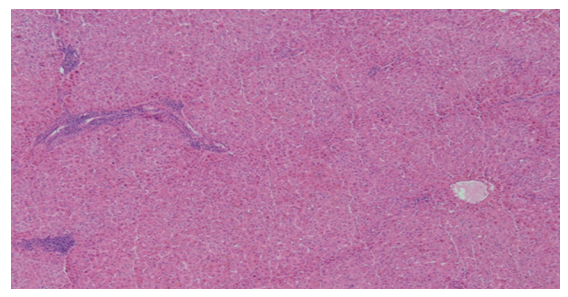
Figure 2: Microscopic view (Hematoxylin and Eosin staining, 20x) confirmed the ectopic liver tissue without pathological features
Cholecystectomy was performed using the standard procedure to include the mass and the specimen was removed and sent for histopathological examination. The postoperative course was uneventful and she was discharged home on the first postoperative day in good condition.The histopatological examination revealed this mass to be ectopic liver parenchyma with normal hepatocytes (Figure 2).
2. Discussion
Ectopic liver tissue is a rare congenital anomaly [1]. It is defined as the presence of liver tissue outside the native liver and is divided into four main types: Ectopic liver tissue that is not connected to the main liver, and is usually attached to the gallbladder wall (as it was in our case), microscopic liver tissue found in the gallbladder wall, a large accessory liver lobe connected to the main liver by a pedicle, small accessory liver lobe which is not connected to the main liver [9]. The incidence of ectopic liver tissue is varying between 0.27% and 0.47% [3]. It can be found in different body organs but the most common location is associated with the gallbladder [2]. Several theories have been proposed to explain the development of the ectopic liver tissue at different body sites; it may occurs as a result of regression or atrophy of the bridge to the main liver, or migration of ectopic liver during the embryological development [11]. Concerning the blood supply of gallbladder associated- ectopic liver tissue, three vascular patterns have been described in the literature: Artery arising from the cystic artery, vascular pedicle arising from the liver parenchyma, or in a form of a mesentery lying from the hepatic site to the ectopic liver tissue [12]. Therefore, if such tissue is encountered during laparoscopic cholecystectomy, the vascular pedicle should be dissected and clipped before the gallbladder dissection to prevent serious bleeding. Ectopic liver tissue-like the native liver tissue- usually has normal histological architecture and it is susceptible to the same pathologies such as fatty changes, cholestasis, hemosiderosis, cirrhosis and malignant transformation [13]. Several studies have been shown that the ectopic liver tissue is strongly associated with hepatocellular carcinoma [2-14]. It is theorized that the high incidence of HCC in the ectopic liver tissue is due to the defect in the functional structure which makes the ectopic liver tissue handicapped and more vulnerable to carcinogens [15]. The incidence of HCC is varying between 46% of ectopic liver tissue encountered outside the mother liver and 2.4% of gallbladder- associated ectopic liver tissue15. In fact, this difference in incidence is due to that the gallbladder- associated ectopic liver tissue occur later during the embryogenesis and therefore, it is well-differentiated than the other ectopic locations [16]. Gallbladder-associated ectopic liver tissue is rarely symptomatic and is usually encountered during laparoscopy (as it was in our case), laparotomy or autopsy [6]. Thus, preoperative diagnosis of ectopic liver tissue is rare and only a few cases have been reported [7,8]. However, when symptoms occur, the main complaint is recurrent right upper quadrant pain due to complications such as torsion, intra-peritoneal bleeding or obstruction [8]. Due its rarity, the small size and the lack of awareness, ectopic liver tissue is usually not recognized by the radiologist (as in the present case); however, it can appear as a soft tissues tumor on the imaging studies [17]. When it is suspected preoperatively, percutaneous biopsy should be avoided due to the risk of bleeding and malignancy [2]. Studies have recommended that when ectopic liver tissue is encountered, it should be excised and sent for histopathological examination because of its serious complications and the potential risk of malignant transformation [8]. Our specimen did not show any evidence of malignant degeneration when excised.
3. Conclusion
To conclude, although it is a rare entity, ectopic liver tissue can be found in different body organs but the most common location is associated with the gallbladder and it may pose a challenge to surgeons when encountered. Surgical excision is strongly recommended with proper histopathological examination to exclude malignant transformation.
References
- Kubota, Keiichi, et al. Ectopic hepatocellular carcinoma arising from pancreas: a case report and review of the literature. World Journal of Gastroenterology 31 (2007): 42-70.
- Martinez, Carlos Augusto Real, et al. Gallbladder-associated ectopic liver: A rare finding during a laparoscopic cholecystectomy. International journal of surgery case reports 4 (2013): 312-315.
- Arslan, Yusuf, et al. Rare entity: ectopic liver tissue in the wall of the gallbladder-a case report. World Journal of Clinical Cases 12 (2014): 924.
- Akbulut, Sami, et al. Ectopic liver tissue (choristoma) on the gallbladder: A comprehensive literature review. World Journal of Gastrointestinal Surgery 12 (2020): 534.
- Cullen, Thomas S. Accessory lobes of the liver: an accessory hepatic lobe springing from the surface of the gallbladder. Archives of Surgery11 (1925): 718-764.
- Avdaj, Afrim, et al. Case report of ectopic hepatic tissue, a rare finding during a laparoscopic cholecystectomy. International journal of surgery case reports68 (2020): 100-103.
- Lundy J, Johnson E, Edwards K, et al. Laparoscopic management of gallbladder associated ectopic liver 9 (2005): 485-487.
- Termos, Salah, et al. Gallbladder-associated symptomatic hepatic choristoma: Should you resect?. International journal of surgery case reports 41 (2017): 243-246.
- Collan Y, Hakkiluoto A, Hästbacka J. Ectopic liver. Annales Chirurgiae et Gynaecologiae 67 (1978): 18-25.
- Sakarya Y, Erhan H, Aydede E, et al. Ectopic liver(choristoma) associated with the gallbladder encountered during laparoscopic cholecystectomy: a case report, Surg Endosc 16 (2002): 11-16.
- Triantafyllidis L, Papapavlou N, et al. Ectopic liver tissue attached to the gallbladder wall: a case report, Cases J 2 (2009): 67-86.
- Bal S, Yilmaz B, Yavas, et al. A rare condition: ectopic liver tissue with itsunique blood supply encountered during laparoscopic cholecystectomy. Int J Surg Case Rep 9 (2015): 47-50.
- Dettmer, Matthias, Gieri C, et al. Alpha 1-antitrypsin retention in an ectopic live. Diagnostic pathology 6 (2011): 1-4.
- Liu KL, Ho MC, Chen PJ. Ectopic liver with hepatocellular carcinoma in the peritoneum. Am J Roentgenol 188 (2007): 206-217.
- Arakawa, Masahiro, et al. Propensity of ectopic liver to hepatocarcinogenesis: case reports and a review of the literature. Hepatology 29 (1999): 57-61.
- Griniatsos, John, Ali R, et al. Two cases of ectopic liver attached to the gallbladder wall. HPB 4 (2002): 191-194.
- Hamdani, Sandra D, Richard L. Ectopic liver simulating a mass in the gallbladder wall: imaging findings. American journal of roentgenology 162 (1994): 647-648.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 