Impact of the SARS-COV2 on Surgical Treatment of Acute Appendicitis: A Retrospective Cohort Multi-Centre Study
Article Information
Jeremi Bedard Ginchereau*, Marc-André Bellavance, Anthonie Hamel, Nicolas Tasse, Sebastien Drolet
Department of Surgery, Université Laval, 2325 Rue de l'Université Québec Quebec G1V0A6, Canada
*Corresponding Author: Jeremi Bedard Ginchereau, Department of Surgery, Université Laval, 2325 Rue de l'Université Québec Quebec G1V0A6, Canada
Received: 08 March 2022; Accepted: 16 March 2022; Published: 16 May 2022
Citation: Jeremi Bedard Ginchereau, Marc-André Bellavance, Anthonie Hamel, Nicolas Tasse, Sebastien Drolet. Impact of the SARS-COV2 on Surgical Treatment of Acute Appendicitis: A Retrospective Cohort Multi-Centre Study. Journal of Surgery and Research 5 (2022): 275-283.
View / Download Pdf Share at FacebookAbstract
Background
Since the pandemic begun, in March 2020, several observational studies attempted to demonstrate the impact of the pandemic on the management of acute appendicitis. As a result, the surgical management of acute appendicitis is still undefined.
Method
A retrospective, cohort, observational study design was used to collect data from electronic medical records between March 13 and June 30, 2020 and the prior year, i.e 2019. All patients over 18 years of age admitted for acute appendicitis and treated surgically were initially included in our study. Timeframes observed in strategic intervals of hospitalization, postoperative complications and 30-days re-consultation rate were collected for analysis.
Results
A total of 371 out of 384 patients were included in the final analysis, i.e. 191 in the PRECOV group and 180 in the COV group. The rate of complicated appendicitis was similar between COV and PRECOV groups (33.9% vs 36.2%, p = 0.6647). However, the LOS was increased in the COV group (1.45 days vs 1.25 days, p = 0.0378). Patients operated during pandemic presented a complication rate similar to patients surgically treated for acute appendicitis before the pandemic (12.8% vs 11.0%, p = 0.6322).
Conclusions
Rate of complicated cases of appendicitis remained similar during the pandemic compared to the pre-pandemic period. The LOS significantly increased during the pandemic, owing mainly to an extended time-to-surgery period. Thus the impact of the pandemic is real, the observed delays seem to be mostly related to the pressure exerted on the system rather than the intrinsic pathology.
Keywords
SARS-COV2; Surgical treatment; Acute appendicitis
SARS-COV2 articles SARS-COV2 Research articles SARS-COV2 review articles SARS-COV2 PubMed articles SARS-COV2 PubMed Central articles SARS-COV2 2023 articles SARS-COV2 2024 articles SARS-COV2 Scopus articles SARS-COV2 impact factor journals SARS-COV2 Scopus journals SARS-COV2 PubMed journals SARS-COV2 medical journals SARS-COV2 free journals SARS-COV2 best journals SARS-COV2 top journals SARS-COV2 free medical journals SARS-COV2 famous journals SARS-COV2 Google Scholar indexed journals Surgical treatment articles Surgical treatment Research articles Surgical treatment review articles Surgical treatment PubMed articles Surgical treatment PubMed Central articles Surgical treatment 2023 articles Surgical treatment 2024 articles Surgical treatment Scopus articles Surgical treatment impact factor journals Surgical treatment Scopus journals Surgical treatment PubMed journals Surgical treatment medical journals Surgical treatment free journals Surgical treatment best journals Surgical treatment top journals Surgical treatment free medical journals Surgical treatment famous journals Surgical treatment Google Scholar indexed journals Acute appendicitis articles Acute appendicitis Research articles Acute appendicitis review articles Acute appendicitis PubMed articles Acute appendicitis PubMed Central articles Acute appendicitis 2023 articles Acute appendicitis 2024 articles Acute appendicitis Scopus articles Acute appendicitis impact factor journals Acute appendicitis Scopus journals Acute appendicitis PubMed journals Acute appendicitis medical journals Acute appendicitis free journals Acute appendicitis best journals Acute appendicitis top journals Acute appendicitis free medical journals Acute appendicitis famous journals Acute appendicitis Google Scholar indexed journals postoperative complications articles postoperative complications Research articles postoperative complications review articles postoperative complications PubMed articles postoperative complications PubMed Central articles postoperative complications 2023 articles postoperative complications 2024 articles postoperative complications Scopus articles postoperative complications impact factor journals postoperative complications Scopus journals postoperative complications PubMed journals postoperative complications medical journals postoperative complications free journals postoperative complications best journals postoperative complications top journals postoperative complications free medical journals postoperative complications famous journals postoperative complications Google Scholar indexed journals intrinsic pathology articles intrinsic pathology Research articles intrinsic pathology review articles intrinsic pathology PubMed articles intrinsic pathology PubMed Central articles intrinsic pathology 2023 articles intrinsic pathology 2024 articles intrinsic pathology Scopus articles intrinsic pathology impact factor journals intrinsic pathology Scopus journals intrinsic pathology PubMed journals intrinsic pathology medical journals intrinsic pathology free journals intrinsic pathology best journals intrinsic pathology top journals intrinsic pathology free medical journals intrinsic pathology famous journals intrinsic pathology Google Scholar indexed journals surgical management articles surgical management Research articles surgical management review articles surgical management PubMed articles surgical management PubMed Central articles surgical management 2023 articles surgical management 2024 articles surgical management Scopus articles surgical management impact factor journals surgical management Scopus journals surgical management PubMed journals surgical management medical journals surgical management free journals surgical management best journals surgical management top journals surgical management free medical journals surgical management famous journals surgical management Google Scholar indexed journals complicated appendicitis articles complicated appendicitis Research articles complicated appendicitis review articles complicated appendicitis PubMed articles complicated appendicitis PubMed Central articles complicated appendicitis 2023 articles complicated appendicitis 2024 articles complicated appendicitis Scopus articles complicated appendicitis impact factor journals complicated appendicitis Scopus journals complicated appendicitis PubMed journals complicated appendicitis medical journals complicated appendicitis free journals complicated appendicitis best journals complicated appendicitis top journals complicated appendicitis free medical journals complicated appendicitis famous journals complicated appendicitis Google Scholar indexed journals impact of the pandemic articles impact of the pandemic Research articles impact of the pandemic review articles impact of the pandemic PubMed articles impact of the pandemic PubMed Central articles impact of the pandemic 2023 articles impact of the pandemic 2024 articles impact of the pandemic Scopus articles impact of the pandemic impact factor journals impact of the pandemic Scopus journals impact of the pandemic PubMed journals impact of the pandemic medical journals impact of the pandemic free journals impact of the pandemic best journals impact of the pandemic top journals impact of the pandemic free medical journals impact of the pandemic famous journals impact of the pandemic Google Scholar indexed journals pre-COVID era articles pre-COVID era Research articles pre-COVID era review articles pre-COVID era PubMed articles pre-COVID era PubMed Central articles pre-COVID era 2023 articles pre-COVID era 2024 articles pre-COVID era Scopus articles pre-COVID era impact factor journals pre-COVID era Scopus journals pre-COVID era PubMed journals pre-COVID era medical journals pre-COVID era free journals pre-COVID era best journals pre-COVID era top journals pre-COVID era free medical journals pre-COVID era famous journals pre-COVID era Google Scholar indexed journals
Article Details
1. Introduction
On March 11, the World Health Organization (WHO) officially declared the COVID19 global pandemic [1]. The impact of the pandemic on existing health systems has been unprecedented. The leaders of these bodies have had to adapt on several levels in order to provide the best possible health care while limiting the spread of the virus. More specifically, the surgical field has not been spared by the COVID-19 pandemic. Among other things, triage protocols and prioritization of operating rooms had to be reviewed in several hospitals. Moreover, in order to guide the different affected bodies, Moletta, L. et al. published a systematic review that highlights guidelines and recommendations for managing operational priorities during the pandemic [2]. While these recommendations aid decision-making for elective surgeries, the challenge remains colossal when it comes to acute surgical care. Since appendicitis remains the most common condition in acute surgical care, several studies have looked at the non-surgical treatment of this condition in the context of the pandemic [3,4]. However, although medical treatment appears to show therapeutic benefits for a selected patient subgroup, appendectomy remains the standard of practice to address this pathology [5,6]. Accordingly, a few studies have attempted to demonstrate the impact of the pandemic on the initial presentation of patients with acute appendicitis. On the other hand, few of them measured the real impact of these delays on the surgical management of acute appendicitis and the rate of complications. Javier Romero et al. demonstrated from a small patient sample that there were a greater number of cases of complicated acute appendicitis during the pandemic compared to the pre-COVID era [7]. In this study, our objective was to evaluate the impact of the pandemic (COV) on the surgical management of acute appendicitis and to compare it to a pre-pandemic cohort (PRECOV) according to the rate of complicated appendicitis and LOS (length of stay).
2. Materials and Methods
2.1 Patients selection
All consecutive patients over 18 years-old of age admitted for acute appendicitis who undergone surgical treatment between March 13 and June 30, 2020 in one of the five university affiliated teaching hospitals of Quebec City metropolitan and surrounding area were identified through medical records and classified as the pandemic group. A pre-pandemic group was identified for the same time period one year prior and used as a comparison group. A standardized retrospective chart review was performed for the two groups. The exclusion criteria were patients having elective interval appendectomies and complementary appendectomy during another procedure. Also, all medically treated patients were excluded.
2.2 Data collection
Patient demographics, comorbidities, time lapsed prior to surgery, operative details, pathology reports, were retrieved for all identified patients. Diagnosis time was defined as the time of imaging confirmation of appendicitis. The admission time was defined when patients were triage at the hospital. The patient's discharge corresponds to the time when the medical team signed the discharge. Surgery time corresponded to the time of the skin incision. Postoperative complications were recorded including ileus, abscess, surgical site infection, pneumonia, urinary retention and others.
2.3 Outcomes
The main outcome was to evaluate the difference in rates of complicated acute appendicitis and the LOS between PRECOV and COV groups. Complicated appendicitis was define using the severity scoring developed by Carlos Augusto Comes et al. 2015 [8]. Secondary objectives included postoperative complications and timeframe observed in strategic interval of hospitalization defined as time between symptoms and admission, admission and surgery, diagnosis and surgery as well as the time between surgery and discharge. Post-operative complications, return to OR and 30-days reconsultation rate were collected. The Clavien–Dindo classification was used for grading complications. This study was reviewed and approved by the local ethics committee.
2.4 Statistical analysis
Mean and 95% confidence intervals, median, standard deviation and quartiles were calculated for quantitative variables and proportions are presented for qualitative variables. Data from the tow study groups (PRECOV et COV groups) were compared using the Chi-square test for categorical variables and the Wilcoxon Mann-Whitney test for continuous variables. Analysis has been performed in SAS 9.4 software.
3. Results
3.1 Patients
From all the 384 appendicitis admitted from the emergency over the study period, appendicectomy was performed in 191 (out of 199) and 180 (out of 185) cases identified respectively before and during the COVID19 pandemic met the inclusion criteria. There were no significant differences in the distribution of age, gender, BMI, smokers and ASA physical status (Table 1) between the two groups. Common and surgically relevant comorbidities such as COPD, type 2 diabetes, coronary heart disease, atrial fibrillation, peripheral atherosclerotic vascular disease (PAD) and chronic renal failure each had a similar prevalence amongst the pre-pandemic and pandemic cohorts. Both of those groups include statistically comparable numbers of patients with past surgical history for abdominal or gynecological procedures (either laparoscopic or by celiotomy).
|
Variable |
2019 (n = 191) |
2020 (n = 180) |
P-value1 |
|
Age, median (IQR) |
40 (27; 57) |
39 (27.5; 56.5) |
0.9521+ |
|
BMI, median (IQR) |
26.33 (23.53; 29.39) |
25.76 (23.07; 29.80) |
0.6539+ |
|
ASA status |
|||
|
I |
123 (64.4) |
110 (61.1) |
|
|
II |
58 (30.4) |
65 (36.1) |
0,2881 |
|
III |
10 (5.2) |
5 (2.8) |
|
|
Sex |
|||
|
Female |
104 (54.5) |
104 (57.8) |
0,5187 |
|
Male |
87 (45.5) |
76 (42.2) |
|
|
HTN |
24 (12.6) |
25 (13.9) |
0,76 |
|
COPD |
3 (1.6) |
2 (1.1) |
1 |
|
Type II diabetes |
|||
|
Insulin |
1 (0.5) |
2 (1.1) |
0,6131 |
|
ADO |
4 (2.1) |
8 (4.4) |
0,2473 |
|
Atrial fibrillation |
5 (2.7) |
2 (1.1) |
0,4496 |
|
DLPD |
18 (9.4) |
19 (10.6) |
0,7322 |
|
CVD |
4 (2.1) |
7 (3.9) |
0,3685 |
|
PAD |
3 (1.6) |
5 (2.8) |
0,4918 |
|
Chronic renal failure |
2 (1.0) |
1 (0.6) |
1 |
|
Smoking |
27 (14.1) |
19 (10.6) |
0,3453 |
|
Previous abdominal surgery |
48 (25.1) |
61 (33.9) |
0.0642T |
All data are expressed as a number (%) except for the age and BMI which are expressed as a median (IQR); (IQR): interquartile range; 1Based on a Pearson Chi Square Test, + Based on Wilcoxon Mann Whitney Test; T < 0.15
Table 1: Characteristic of the patients
3.2 Appendicitis severity and postoperative complications
Cases of complicated appendicitis (see Table 2) were not encountered more frequently in the COV group compared to the PRECOV group (61 cases vs. 61 cases, p = 0.66). Additionally, the spectrum of severity of complicated appendicitis also remained unchanged during the pandemic, as the occurrence of necrotic appendicitis (10 vs. 6, p = 0.4237), phlegmonous appendicitis (11 vs. 13, p = 0.4244), peri-appendicular abscesses (16 vs. 11, p = 0.6043) and purulent peritonitis secondary to appendicitis (41 vs. 32, p = 0.3275) were not statistically different between the two groups. A laparoscopic approach was initially performed in all patients and conversion to laparotomy was needed only once in both groups. Cases in which surgeons opted for a surgical stapling device rather than endoloops to control the appendix stump were also comparable before and after the outbreak of COVID-19. The technique used to seal the appendix stump was not reported for one patient of the pre-pandemic group. Twenty-one and twenty-three acute complications occurred after appendicectomy in patients belonging to the COV and PRECOV group, respectively (see Table 3). While the rate of postoperative complications remained stable despite the pandemic (11.0 vs. 12.8%, p = 0.6322), the severity of such complications may have increased marginally in the pandemic group. According to the Clavien-Dindo classification, grade II complications arose in 5 patients of the PRECOV group compared to 14 patients in the COV group. Two grade III complication were identified in the pre-pandemic cohort and one patient had to be taken back to the OR for surgical abscess drainage. On the other hand, one patient from the pandemic group suffered from a grade IV complication (postoperative hemoperitoneum) and 4 of them had to be transferred to the ICU. No statistical difference were found regarding the number of patients who had to be brought back to the OR during their hospital stay (3 vs. 1 patient, p = 0.6236) as well as the total of return visits to the ER within 30 days from their surgery.
|
Variable |
2019 |
2020 |
P-value1 |
|
Complicated appendicitis |
69 / 191 (36.1) |
61/180 (33.9) |
0,6647 |
|
Segmental necrosis |
10 (14.5) |
6 (9.8) |
0,4199 |
|
Phlegmon |
11 (15.9) |
13 (21.3) |
0,431 |
|
Abcess |
16 (23.2) |
11 (18.0) |
0,4696 |
|
Purulent peritonitis |
41 (59.4) |
32 (52.5) |
0,4247 |
|
Instrumentation |
|||
|
EndoGIA |
93/189 (49.2) |
105/180 (58.3) |
0.0947T |
|
Endoloop |
96/189 (50.8) |
75/180 (41.7)) |
|
|
Conversion to laparotomy |
1/191 (0.5) |
2/180 (1.1) |
0,6131 |
All data are expressed as a number (%); 1Based on an Exact Pearson Chi Square Test; T < 0.15
Table 2: Peroperative characteristics
|
Variable |
2019 |
2020 |
P-value1 |
|
Overall complication |
21/191 (11.0) |
23/180 (12.8) |
0,6322 |
|
Clavien-Dindo classification |
|||
|
I |
182/189 (96.3) |
164/180 (91.1) |
|
|
II |
5/189 (2.6) |
15/180 (8.3) |
0.0111* |
|
III |
2/189 (1.1) |
0/180 (0) |
|
|
IV |
0/189 (0) |
1/180 (0.6) |
|
|
Transfer to ICU |
1/190 (0.5) |
4/180 (2.2) |
0,2042 |
|
Reoperation |
3/191(1.6) |
1/180 (0.6) |
0,6236 |
|
30-days reconsultation |
8/191 (4.2) |
3/180 (1.7) |
0,1524 |
All data are expressed as a number (%).; 1Based on an Exact Pearson Chi Square Test; * <0.05; ** <0.01
Table 3: Postoperative complications
3.3 Length of stay (LoS) and time lapses in the management of acute appendicitis
The LOS was significantly longer in the COV group in comparison to the PRECOV group (1.25 vs. 1.48 days, p = 0.0378) (see Table 4). Sub-analysis of different time intervals revealed no differences in the number of days elapsed from symptoms onset to the moment at which patients were admitted to the emergency department, in both groups. However, the time period from patient admission to surgery (11.01 vs. 14.1 hours, p = 0.0002), from radiological diagnosis of acute appendicitis to surgery (6.95 vs. 8.65 hours, p = 0.0007) and from the surgical consultation to surgery (4.18 vs. 5.13 hours, p = 0.0275) were all significantly longer in the pandemic group. Whereas patients underwent surgery significantly faster after admission to the ED in the pre-pandemic era, the amount of time between surgery and discharge from the hospital remained similar in both groups (0.72 vs 0.74 days, p = 0.567).
|
Variable |
2019 (n = 190) |
2020 (n= 179) |
P-value1 |
|
Overall length of stay, d |
1.25 (0.93; 2.12) |
1.48 (0.98; 2.95) |
0.0378* |
|
Preoperative |
|||
|
Time between symptoms and admission, d |
1 (1; 2) |
1 (1; 2) |
0,3595 |
|
Time between admission and surgery, h |
11.01 (7.25; 16.55) |
14.1 (8.55; 20.62) |
0.0002*** |
|
Time between diagnosis and surgery, h |
6.95 (5.13; 9.75) |
8.65 (7.73; 13.92) |
0.0009*** |
|
Time between surgical consultation and surgery, h |
4.18 (2.57; 7.08) |
5.13 (2.56; 10.27) |
0.0275* |
|
Postoperative |
|||
|
Time between surgery and discharge, d |
0.72 (0.51; 1.63) |
0.74 (0.45; 1.84) |
0,567 |
All data are expressed as a median (IQR); (IQR): interquartile range; 1 Based on Wilcoxon Mann Whitney Test; *** <0.001; * <0.05
Table 4: Outcomes
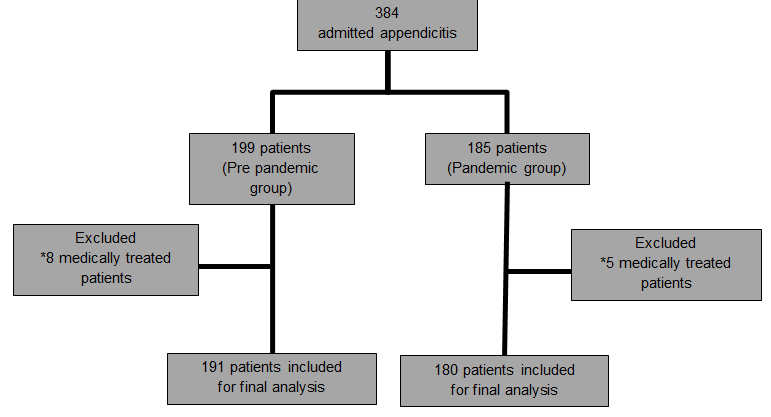
Figure 1: Flowchart of the patients recruitment and selection
4. Discussion
This study, carried out in high-volume centers, shows the real effect of the pandemic on the management of acute appendicitis. Although several studies assessed the efficacy of various non-surgical therapies of acute appendicitis in selected patients, the impact of the pandemic on the surgical care of this disease remains completely elusive [4,9,10]. We therefore sought to study the impact of the COVID-19 outbreak on the management of acute appendicitis with a specific focus on the outcomes of standard surgical care especially by assessing the surgical management of acute appendicitis, using severity score, LoS, and post-operative complications. Patel et al. observed a significant decrease in the number of cases of acute appendicitis during the pandemic and stipulated that this was due to patients being more reluctant to present at the hospital [11]. In contrast, in our study, the number of patients in the PRECOV and COV groups were statistically similar since the incidence of cases of acute appendicitis in our hospitals during the pandemic decreased by only 10%. This suggest that patients benefited from a comparable accessibility to the emergency department in spite of the pandemic situation. The rate of surgical management between PRECOV and COV (80% vs. 83%) was also similar, revealing that the standard acute surgical care could still be offered to patients despite significant constraints on surgical resources since the outbreak of COVID-19. As outlined by Di Saverio, S. et al. prehospital delay is a key independent predictor of complicated disease and can thus lead to greater morbidity and mortality [12]. Our data reveals that the rates of complicated appendicitis as well as the more severe forms of the complicated disease were comparable between the PRECOV and COV groups. These results may be explained in part by the fact that patients did not present later to the hospital after the onset of their symptoms, as also reported by James Tankel et al. [13]. The overall complication rate was also found to be similar between the two groups in the postoperative setting. Complication rates observed in this study are in accordance with the current literature, i.e. an overall complication rate of 4-18% [14,15]. According to the Clavien-Dindo classification, the distribution in the severity of postoperative complications appears to be slightly skewed towards more severe complications in the COV group. The relevance of this finding however remains to be determined, since the paucity of events prevented us from performing proper statistical analyses. Interestingly, the increased ratio of Grade II complications observed in the COV group may be related to a more liberal use of postoperative antibiotics by some surgeons during the pandemic. Such practice may have been motivated by the need to avoid any potential discharge delays at times in which hospital beds were in dire demand. In addition, our study shows that the LOS slightly increased during the pandemic, which is also consistent with the current emerging literature (1.25 vs 1.48, p = 0.0378) [16]. However, even if our results seem statistically significant, we can question their value in a clinical practice. In fact, the difference in LOS represent less than a day, we can therefore argue that they are not clinically significant. Even so, our study brings interesting insights into which steps in the surgical management of acute appendicitis are responsible for the increased LOS observed during the pandemic. Noteworthily, we note that the preoperative period is mostly accountable for the extended LOS observed during the pandemic. Several factors may have contributed to this delay. Waiting times resulting from batch polymerase chain reaction (PCR) analyses is certainly one of the most contributing factors. The modification of sorting protocols, the required personal protective equipment (PPE), the first generation of COVID-19 PCR test and the training of the staff are also all determinants that may have had an impact. There are some limitations to our study. The study design limits the collection of data. Indeed, some data were lacking such as specificities of the surgical technique and reasons behind the transfer of a patient to the ICU in the pre-pandemic group.
5. Conclusion
We studied the impact of the COVID19 pandemic on the management of the most prevalent disease in the acute care surgery, which is the acute appendicitis. Rate of complicated appendicitis remain similar in comparison to a pre pandemic cohort. The rate of surgical management was similar during the pandemic period suggesting adequate preservation of OR access for acute surgical care. Length of stay was statistically increased during the pandemic mostly in relation to a prolong time-to-surgery period, but the clinical relevance of this results should be analyzed in more details. Despite this, time for obtaining negative preoperative COVID testing result, PPE and sorting protocols were probably responsible in part for these increased delays. In a future study, it would be interesting to measure the impact of the adjustment made by health authorities after this worldwide sanitary crisis on the acute care surgery.
References
- Organization WH. Coronavirus disease 2019 (COVID-19) Situation Report 51. World Health Organization (2020).
- Moletta L, Pierobon ES, Capovilla G, et al. International guidelines and recommendations for surgery during Covid-19 pandemic: A Systematic Review. Int J Surg 79 (2020): 180-188.
- Collard M, Lakkis Z, Loriau J, et al. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisis. J Visc Surg 157 (2020): S33-S42.
- Ganesh R, Lucocq J, Ekpete NO, et al. Management of appendicitis during COVID-19 pandemic; short-term outcomes. Scott Med J 12 (2020): 36-93.
- Salminen P, Paajanen H, Rautio T, et al. Antibiotic Therapy vs Appendectomy for Treatment of Uncomplicated Acute Appendicitis: The APPAC Randomized Clinical Trial. JAMA 313 (2015): 2340-2348.
- Collaborative C, Flum DR, Davidson GH, et al. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N Engl J Med (2020).
- Romero J, Valencia S, Guerrero A. Acute Appendicitis During Coronavirus Disease 2019 (COVID-19): Changes in Clinical Presentation and CT Findings. J Am Coll Radiol 17 (2020):1011-1013.
- Gomes CA, Sartelli M, Di Saverio S, et al. Acute appendicitis: proposal of a new comprehensive grading system based on clinical, imaging and laparoscopic findings. World J Emerg Surg 10 (2015): 60-70.
- Ielpo B, Podda M, Pellino G, et al. Global attitudes in the management of acute appendicitis during COVID-19 pandemic: ACIE Appy Study. Br J Surg 12 (2020).
- Kelly ME, Murphy E, Bolger JC, et al. COVID-19 and the treatment of acute appendicitis in Ireland: a new era or short-term pivot? Colorectal Dis 22 (2020): 648-649.
- Patel VK, Ye K, In H, et al. Non-operative Management for Acute Appendicitis During the COVID-19 Pandemic Does Not Increase the Rate of Complications. J Gastrointest Surg 25 (2021): 1327-1329.
- Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg 15 (2020): 27.
- Tankel J, Keinan A, Blich O, et al. The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-centre Study. World J Surg 44 (2020): 2458-2463.
- Tiwari MM, Reynoso JF, Tsang AW, et al. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg 254 (2011): 927-932.
- Dumas PR, Subramanian M, Hodgman E, et al. Laparoscopic Appendectomy: A Report on 1164 Operations at a Single-Institution, Safety-Net Hospital. Am Surg 84 (2018).
- Dick L, Green J, Brown J, et al. Changes in Emergency General Surgery During Covid-19 in Scotland: A Prospective Cohort Study. World J Surg 44 (2020): 3590-3594.


 Impact Factor: * 4.2
Impact Factor: * 4.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 