A Survey of Residency Directors in Academic Trauma Centers for Policies on Airway Management in the Trauma Ward
Article Information
George L Tewfik1, Michal Gajewski2, Jena Salem1, Neil Borad3, Michael Zales1, Gopal Govindaraj4*
1Department of Anesthesiology, Rutgers- New Jersey Medical School, Newark, NJ USA
2Department of Anesthesiology, CHRISTUS St. Vincent Regional Medical Center, Santa Fe, NM, USA
3Department of Anesthesiology, New York Presbyterian Hospital-Weill Cornell Medical Center, New York NY, USA
4Department of Anesthesiology, NYU Grossman School of Medicine, New York, NY, USA
*Corresponding Author: George Tewfik, Department of Anesthesiology, Rutgers- New Jersey Medical School, 185 South Orange Ave. Newark, NJ 07101, USA
Received: 13 September 2022; Accepted: 22 September 2022; Published: 24 October 2022
Citation: George L Tewfik, Michal Gajewski, Jena Salem, Neil Borad, Michael Zales, Gopal Govindaraj. A Survey of Residency Directors in Academic Trauma Centers for Policies on Airway Management in the Trauma Ward. Journal of Surgery and Research. 5 (2022): 576-584.
View / Download Pdf Share at FacebookAbstract
Background: Despite its presence as a critical procedure in the trauma setting, airway management is not performed uniformly, varying between institutions, particularly with personnel involved in decision-making. Past literature has noted a trend in which emergency medicine physicians assumed greater responsibility for primary management of airways in the trauma ward. Many institutions have adopted tiered activation systems for traumas in order to improve patient care, deploying resources more effectively.
Methods: In this study, a survey of residency directors was deployed to assess trends in airway management. A validated survey was distributed to residency directors in anesthesiology, general surgery and emergency medicine in 190 Level I trauma centers in the United States. Questions assessed personnel management, complication tracking and difficult airway prediction factors, amongst other considerations for airway management in the trauma bay.
Results: Respondents completed the survey at a rate of 23.8% of those solicited. A majority of respondents indicated that emergency medicine physicians are primary airway managers in the trauma bay and that their institutions utilize tiered trauma activation systems at 77.4% and 95.6% respectively. Anesthesia providers were immediately available in 81% of respondent institutions with inconclusive data regarding protocols for delineating anesthesia involvement in difficult airways. More than a third of respondents indicated their institution either does not track airway complications or they did not know if complications were tracked. Finally, nine different criteria were used in varying degrees by respondents’ institutions to predict the presence of a difficult airway, including such factors as head/face trauma, airway fluid and obesity.
Keywords
Airway management, Trauma anesthesia, Emergency intubations, Trauma intubations, Emergency department airways
Airway management articles; Trauma anesthesia articles; Emergency intubations articles; Trauma intubations articles; Emergency department airways articles
Airway management articles Airway management Research articles Airway management review articles Airway management PubMed articles Airway management PubMed Central articles Airway management 2023 articles Airway management 2024 articles Airway management Scopus articles Airway management impact factor journals Airway management Scopus journals Airway management PubMed journals Airway management medical journals Airway management free journals Airway management best journals Airway management top journals Airway management free medical journals Airway management famous journals Airway management Google Scholar indexed journals Trauma anesthesia articles Trauma anesthesia Research articles Trauma anesthesia review articles Trauma anesthesia PubMed articles Trauma anesthesia PubMed Central articles Trauma anesthesia 2023 articles Trauma anesthesia 2024 articles Trauma anesthesia Scopus articles Trauma anesthesia impact factor journals Trauma anesthesia Scopus journals Trauma anesthesia PubMed journals Trauma anesthesia medical journals Trauma anesthesia free journals Trauma anesthesia best journals Trauma anesthesia top journals Trauma anesthesia free medical journals Trauma anesthesia famous journals Trauma anesthesia Google Scholar indexed journals Emergency intubations articles Emergency intubations Research articles Emergency intubations review articles Emergency intubations PubMed articles Emergency intubations PubMed Central articles Emergency intubations 2023 articles Emergency intubations 2024 articles Emergency intubations Scopus articles Emergency intubations impact factor journals Emergency intubations Scopus journals Emergency intubations PubMed journals Emergency intubations medical journals Emergency intubations free journals Emergency intubations best journals Emergency intubations top journals Emergency intubations free medical journals Emergency intubations famous journals Emergency intubations Google Scholar indexed journals Trauma intubations articles Trauma intubations Research articles Trauma intubations review articles Trauma intubations PubMed articles Trauma intubations PubMed Central articles Trauma intubations 2023 articles Trauma intubations 2024 articles Trauma intubations Scopus articles Trauma intubations impact factor journals Trauma intubations Scopus journals Trauma intubations PubMed journals Trauma intubations medical journals Trauma intubations free journals Trauma intubations best journals Trauma intubations top journals Trauma intubations free medical journals Trauma intubations famous journals Trauma intubations Google Scholar indexed journals Emergency department airways articles Emergency department airways Research articles Emergency department airways review articles Emergency department airways PubMed articles Emergency department airways PubMed Central articles Emergency department airways 2023 articles Emergency department airways 2024 articles Emergency department airways Scopus articles Emergency department airways impact factor journals Emergency department airways Scopus journals Emergency department airways PubMed journals Emergency department airways medical journals Emergency department airways free journals Emergency department airways best journals Emergency department airways top journals Emergency department airways free medical journals Emergency department airways famous journals Emergency department airways Google Scholar indexed journals anesthesiologists articles anesthesiologists Research articles anesthesiologists review articles anesthesiologists PubMed articles anesthesiologists PubMed Central articles anesthesiologists 2023 articles anesthesiologists 2024 articles anesthesiologists Scopus articles anesthesiologists impact factor journals anesthesiologists Scopus journals anesthesiologists PubMed journals anesthesiologists medical journals anesthesiologists free journals anesthesiologists best journals anesthesiologists top journals anesthesiologists free medical journals anesthesiologists famous journals anesthesiologists Google Scholar indexed journals emergency medicine articles emergency medicine Research articles emergency medicine review articles emergency medicine PubMed articles emergency medicine PubMed Central articles emergency medicine 2023 articles emergency medicine 2024 articles emergency medicine Scopus articles emergency medicine impact factor journals emergency medicine Scopus journals emergency medicine PubMed journals emergency medicine medical journals emergency medicine free journals emergency medicine best journals emergency medicine top journals emergency medicine free medical journals emergency medicine famous journals emergency medicine Google Scholar indexed journals trauma centers articles trauma centers Research articles trauma centers review articles trauma centers PubMed articles trauma centers PubMed Central articles trauma centers 2023 articles trauma centers 2024 articles trauma centers Scopus articles trauma centers impact factor journals trauma centers Scopus journals trauma centers PubMed journals trauma centers medical journals trauma centers free journals trauma centers best journals trauma centers top journals trauma centers free medical journals trauma centers famous journals trauma centers Google Scholar indexed journals
Article Details
Background
Emergency airway intubation is a critical resuscitative procedure in the trauma setting. Failure to secure the airway in an acutely unstable patient greatly increases patient morbidity and mortality. Factors such as airway trauma, cervical spine immobilization and hemodynamic instability require urgent intervention [1,2]. These conditions, however, may concomitantly complicate the intubation process thereby requiring skilled laryngoscopy for appropriate management. Despite its clinical importance, the management of traumatic airways varies from one trauma center to another. No universally designated roles of the anesthesiologist, emergency medicine physician and trauma surgeon in the airway management of the trauma patient have been established3. What historically has been managed primarily by anesthesiologists has evolved to include a greater mix of emergency physicians at academic trauma centers throughout the United States [3].
Much research to date regarding intubation of the trauma patient has compared outcomes of emergency intubations managed by anesthesiologists and emergency physicians to find similar success and complication rates, suggesting both anesthesiologists and emergency physicians are equally qualified to manage traumatic airways [4]. The intubation success rates of physicians in the emergency department has been well studied [5], as has the prevalence of rapid sequence intubation, surgical airway management and alternate airway management techniques in rescue airway management. First pass success rates for intubation by Emergency Medicine physicians in the Emergency Department has been shown to be as high as 84.1% in a recent meta-analysis [5]. Less clear are the dynamics between emergency medicine physicians, anesthesiologists and trauma surgeons in managing patients with failed intubations and high priority traumas at academic level 1 trauma centers. More current information is needed that characterizes the role of each of these services in airway management in these critical situations. The utilization of specific strategies and algorithms when managing difficult airways, indicating pre-planning for such scenarios, has been considered a critical factor in improved patient outcomes [6].
Also of interest is the use of tiered trauma activation protocols at trauma centers throughout the United States. The benefit of such systems on patient outcomes is well demonstrated in the literature, showing more. Several studies highlight the efficacy of a tiered trauma activation system in reducing under triage rates, increasing over triage rates and reducing resources spent per trauma patient [7,8]. Statistically significant differences in injury severity have been demonstrated between patients in minor trauma versus major trauma groups, suggesting such systems are appropriately allocating time and resources to maximize patient outcomes [9]. The literature also demonstrates an association between lack of compliance to tiered trauma protocols and increased under triage rates, demonstrating the importance of such a system. While the benefits of tiered trauma activation systems is well demonstrated, an understanding of how prevalent such systems are throughout the United States is useful but lacking. Such information, in conjunction with other data obtained in the survey, may demonstrate associations between the presence of tiered trauma systems and patient outcomes.
The purpose of this study is to identify the intubation and trauma activation protocols at academic trauma centers throughout the United States. This study will provide insight into the evolving roles of anesthesiology, emergency medicine and surgical practitioners in the academic trauma setting regarding airway management. It has the potential to highlight disparities in emergency airway management complication rates as well as allocation of hospital resources to trauma activations across American trauma centers, ultimately improving patient outcomes in the trauma setting.
Methods
After obtaining Institutional Review Board approval from Rutgers University, an internally validated survey was developed to assess intubation practices in trauma departments. This survey was targeted for completion by practitioners in anesthesiology, trauma surgery and emergency medicine at academic centers. Demographic questions begin the survey including name of trauma center and level of traumas seen. Subsequent questions assessed the following information: primary airway management team of each center, the presence of a tiered activation system, the use of a protocol in trauma intubations that delineate responsibilities to different teams, criteria for anesthesiology involvement, availability of the anesthesiology team, criteria for determining a difficult airway, institutional tracking of airway complications as well as the presence or absence of a residency program at each institution.
A list was then created of all Level 1 trauma centers in the United States, using available data on the American College of Surgeons website [10]. These include 190 Level 1 centers. These centers were then evaluated to determine if they were affiliated with an ACGME residency program, using publicly available data on the ACGME website, www.acgme.org. A list of residency directors’ emails was created yielding 155 anesthesia, 240 emergency medicine and 318 general surgery contacts at these institutions. A number greater than the total number of trauma centers is present due to an inability to determine a definitive contact for each residency director; often multiple emails were present on websites for residencies, and 2-3 different email addresses used for the study for the same institution’s residency program. Only one response would later be accepted per institution, and duplicates would be removed.
The validated survey was uploaded onto Google Forms, and the survey was distributed via email using a standard solicitation. The survey developed for this study is provided as Survey Supplemental file 1. Follow up emails were sent on a half dozen occasions to recruit additional respondents. Analysis of results was conducted in both Google Forms, as well as Microsoft Excel.
Results
A total of 713 residency directors were emailed requesting completion of the survey to assess intubation patterns in trauma wards. 170 survey responses were received from these trauma centers meeting the aforementioned inclusion criteria, for a respondent rate of 23.8%. Of these entries, 49 were duplicate entries from 39 institutions. Elimination of duplicate entries identified 121 original survey responses.
In the survey’s responses, the Emergency Department (ED) physicians were identified as the primary team managing the airway in the trauma bay at 77.4% (Figure 1a). Physician anesthesiologists were the primary team in only a minority of cases (5.8%), compared to adopting a collaborative approach between all involved teams (13.9%). In very few cases, the primary team responsible for the trauma bay airway were trauma surgeons (1.5%) or a system of alternating between ED physicians and anesthesiologists (1.5%). Note that these respondents also indicated that their institutions implemented a formal scheduling that defined this responsibility as alternating between for ‘odd’ vs ‘even’ days, or an informal understanding between the departments to switch.
Institutions of 95.6% of those surveyed utilize a tiered trauma activation system, while only 4.4% do not (Figure 1b). Participants were also asked if an anesthesia team member comes to the trauma bay in the setting of highest priority traumas. There was only a small difference between respondents who indicated that anesthesia providers respond to highest priority traumas versus those that do not, 48.1% versus 46% respectively. The remainder of responses indicated more nuanced situations – for 3.6%, an anesthesia team member comes to the trauma bay for high priority traumas only when requested for back-up or ‘as-needed’. In addition, one respondent (0.7%) indicated that anesthesia responds depending on who is on-call from the anesthesia team. Finally, 2 respondents (1.5%) noted that anesthesia responds in order to assess operating room needs and for operative planning.
69.3% of surveyed respondents’ institutions have a protocol for trauma bay intubations that delineates responsibilities for different providers, whereas 30.7% do not (Figure 2a). 33.6% of respondents indicated that their institution does not have a protocol or guidelines to determine when anesthesia should become involved for an intubation/airway management (Figure 2c). In addition, 32.8% of respondents indicate that the anesthesia team gets involved only by the request of the trauma surgeon or emergency department (ED) attending physician for encountered or anticipated difficult airways. Another significant portion (18.2%) of respondents described their criteria for anesthesia involvement as failure to intubate by the emergency medicine team, which includes the presence of multiple failed attempts. For 5.8% of respondents, anesthesia is involved for all highest-level trauma activations. Anesthesia is involved for trauma bay intubations on specific, scheduled days for 2.9% of cases, whereas for a similar portion (3.6%) the described airway management protocol does not involve the anesthesia service. For a minority of cases, anesthesia involvement is prompted in cases requiring operating room planning (1.5%). In one case each (0.7%), the protocol for anesthesia involvement is pediatric airways or for specific, defined characteristics of the patient and airway.

Figure 1: Answers to trauma intubation practice patterns survey. 1a- Assessment of primary service for airway management in the trauma bay. 1b- Assessment of presence of tiered trauma activation system. 1c- Presence or absence of anesthesia team for highest priority traumas.
The anesthesia team is immediately available in 81.0% of respondents’ institutions even when not managing the airway in the trauma bay, leaving only 19.0% of cases where they are not readily available (Figure 2b). For 38.7% of respondents, anesthesia at their institution takes over in the event that another team has a failed attempt at managing an airway (Figure 3a). However, for 27.7%, anesthesia does not take over in this situation. A similar portion (26.3%) indicate that anesthesia does not automatically take over in such a situation but are available to be requested by the emergency medical team. For 6.6% of surveyed respondents, anesthesia steps-in after two or more failed attempts, whereas for only 1 respondent (0.7%), anesthesia automatically steps-in for difficult pediatric airways.
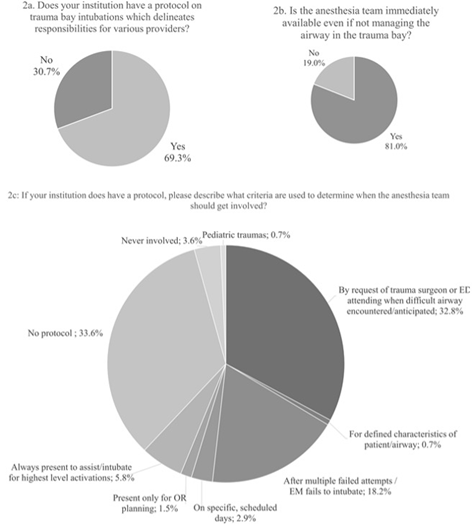
Figure 2: Answers to trauma intubation practice patterns survey (continued). 2a- Assessment of the presence of protocol of provider responsibility. 2b- Presence of anesthesia team to manage airways emergently. 2c- Assessment of criteria for anesthesia provider involvement in airways.
In this cohort of respondents, 61.3% of those surveyed indicated that their institution tracks airways complications encountered in the trauma bay (Figure 3b). However, 34.3% indicated that their institution does not track such complications, and 4.4% of respondents did not know if trauma bay airway complications were tracked or not.
Those surveyed were additionally asked which service specifically would be responsible for the majority of airway complications, to which 72 respondents that found the question applicable (Figure 3c). Of these respondents, 83.3% of respondents indicated that Emergency Medicine is responsible for the majority of airway complications in the trauma bay. 4.2% felt that anesthesia was responsible for the majority of such complications, and 5.6% indicated the surgical service. The remaining 6.9% indicated that none of these three services would be primarily held responsible for the majority of trauma bay airways complications.
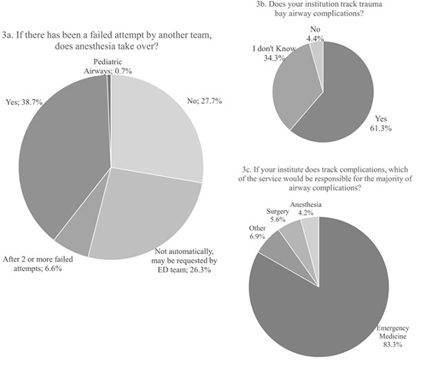
Figure 3: Answers to trauma intubation practice patterns survey (continued). 3a- Assessment of anesthesia involvement following failed attempt at securing airway. 3b- Tracking of airway complications. 3c- Service most often responsible for complications in the trauma bay.
When asked to select from residency programs - anesthesia, emergency medicine, surgery - that their institution has, most (67.2%) have all three (Figure 4). 23.4% have emergency medicine and surgery residencies without an anesthesia residency. A minority have surgery only (2.9%) or anesthesia and surgery without emergency medicine (6.6%). No institution of those surveyed had only anesthesia, only emergency medicine, or emergency medicine and anesthesia residencies without a surgery residency.
Respondents were asked to select, from a list of nine criteria (Mallampati Score; Presence of a C - Collar; Trauma to head/face; Fluid in Airway; Thyromental Distance; Neck Mobility; Obesity; Incisor Distance; Unsuccessful Intubation by paramedics) those factors that are incorporated into their institution’s protocol for defining a difficult airway (Figure 5). 114 of respondents’ institutions (83.2%) have a known, defined criteria for determining a difficult airway in the trauma bay that incorporates at least one of these nine criterium listed. The most often used criterium from these nine was ‘Trauma to head/face’ with 82.5% having this among their criteria, followed by ‘Fluid in the airway’ at 65.7%. ‘Obesity’ and ‘Unsuccessful intubation by paramedics’ each had 64.2% of respondents reporting these as included in their criteria. 58% of respondents’ institutions’ criteria incorporate the presence of a C-collar, followed by 51.1% for limited neck mobility and 39.4% for high Mallampati score. Of the nine criteria given, thyromental distance (32.1%) and incisor distance (26.3%) were least used. A minority of respondents (2.9%) used additional criteria not given (three respondents) or had a defined criteria that included none of the nine given (one respondent). For additional criteria not listed, one respondent each reported that their criteria include ‘King airway’, ‘difficult/unsuccessful intubation by surgery’, or ‘supraglottic airway’.
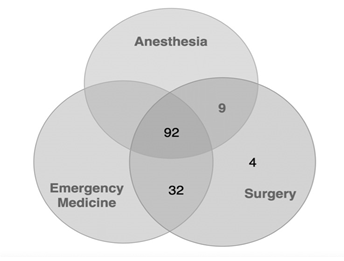
Figure 4: The presence of residency programs at respondents’ trauma institutions. Most respondents (92) had all 3 residency programs. Very few had only a surgical residency, or only anesthesia and surgery without emergency medicine.
Figure 5 also indicates that, of survey respondents, 5.8% indicated that they did not know if their institution has a defined criteria for trauma bay difficult airways, while 10.2% indicated that their institution lacks a standard set of criteria, which may reflect in variation in practice according to each physician. The responses were additionally analyzed according to how many criteria from the nine given, that each respondent selected, including any additional criteria provided by respondents in the three cases mentioned above.
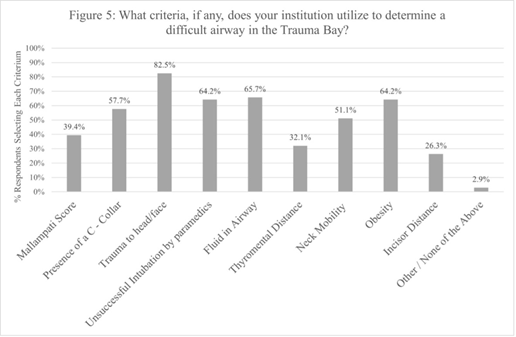
Figure 5: Assessment of criteria utilized by respondents to determine if patient has a difficult airway
The largest portion of respondents selected all nine criteria (15.3%), while 10.2% of respondents selected all but one of the criteria given. 8.0% of respondents selected 7/9 criteria while a similar portion (8.8%) selected 5/9 criteria. 13.1% selected 6/9 criteria and, similarly, 11.7% selected 4 criteria. One respondent that indicated 4 criteria as part of their institution’s protocol selected, including 3 of 9 from the given criteria, adding ‘difficult intubation/unsuccessful by surgery’ as an additional defined criterion. In addition, 2 other respondents, both selecting 2/9 from the given criteria, described supplementary criteria of a ‘King airway’ or the presence of a previously placed ‘supraglottic airway’. Including these two respondents, 10.9% of total respondents selected 3 criteria. A minority indicated only 2 criteria (1.5%), none of the given criteria (0.7%), or selected only one criterion (3.6%).
Discussion
This investigation sought to characterize current trends in the approach to airway management in Level I trauma centers. Specific elements of interest were the way that responsibilities pertaining to this duty were delegated to particular services and the different ways of defining the difficult airway. Additionally, we sought to contextualize this inquiry within the framework of current established institutional guidelines and protocols. The institutions of those surveyed may be generally described as using a tiered trauma activation system (95.6%, Figure 1b) and maintaining residency programs in Emergency Medicine and Surgery (90.5%), with (67.1%) or without (23.4%) Anesthesia (Figure 4).
When asked which service is the primary team for airway management in the trauma bay at their institution, the majority of respondents (77.4%) selected Emergency Medicine (Figure 1a). This finding is paralleled by the 83.3% of respondents that believe Emergency Medicine would be held responsible for the majority of airway complications (Figure 3c). These figures are reflected in the way that the responsibility for airway management in the emergency and trauma settings has shifted over the last several decades from the anesthesia service to that of emergency medicine [3]. Indeed, a variety of literature has demonstrated that such a shift in responsibilities does not significantly impact intubation complication or failure rates [4,11,12], even when applied specifically to resident physicians, or in systems that utilize an alternating schedule between these two services [13], the latter of which was indicated in this study by 1.5% of respondents (Figure 1a). Nonetheless, despite a variety of literature evidencing this transition, this survey demonstrates that there continues to be a lack of a uniform approach in delegating the main responsibility for trauma bay airway management to a specific service.
A lack of uniformity was also revealed in this survey with respect to institutions’ approaches to establishing airway management protocols; 30.7% of respondents’ institutions have no protocol to delineate responsibilities for trauma bay intubations to various providers (Figure 2a) while 33.6% did not have a protocol to specify when anesthesia should become involved for an intubation/airway management (Figure 2c). In 2009, Casey et al. demonstrated the safety and efficacy of implementing a trauma airway protocol, which allowed a maximum of two failed attempts by emergency medicine to establish an airway before anesthesia was automatically called to assist within 5-10 minutes [14]. Further investigations have also demonstrated the high levels of success that an algorithmic or protocol-driven approach to emergency airway management can impart [2,15]. Conversely, disadvantages to such an approach that have been considered include the possible detriment to the individualization of patient care and departure from the ‘practice’ of medicine6. Perhaps in an effort to synthesize these approaches, 32.8% of respondents indicated that their institutions established protocols to specify the obligation for anesthesia involvement as according to the judgement of emergency medicine or trauma surgeon physicians (Figure 2c). In this way, an established guideline clarifies what necessarily elicits anesthesia to become involved, while also leaving the option for clinical judgment and situationally driven care individualized to the patient.
While the paradigm of Emergency Medicine assuming airway management in the trauma bay from Anesthesia has been well established and studied, the role of the surgery service in this setting has been less standardized and reviewed. It is less clear in the literature the effect of placing the primary responsibility for airway management, or liability for related complications, with trauma surgeons, although their role as primary airway manager was only reported by 1.5% of respondents (Figure 1a) and only 5.6% (Figure 3c) of respondents indicated that surgical services were responsible for the majority of complications in airway management.
Moreover, it was clear that the surgery service consistently contributes to airway management, beyond surgical airways. Despite not being the principal managers of the airway, they play a role in determining when to request anesthesia’s involvement for 32.8% of respondents (Figure 2c). In addition, the surgical services participate in a collaborative approach for primary airway management with all services for 13.9% of respondents (Figure 1a).
While airway management outcomes have been analyzed with respect to variables such as the primary service responsible (discussed above), the effect of other elements, such as implementation of criteria to standardized assessment of the difficult airway, are less clear. Out of nine criteria provided, each of them were instituted in 26.3% - 82.5% of surveyed institutions’ protocols (Figure 5a).
However, the value of these criteria is indeterminate. In an investigation evaluating Cormack-Lehane grade, modified LEMON score, and Glasgow Coma Scale score versus intubation difficulty, only a thyroid-to-hyoid distance of <2 fingers was found as an independent variable to predict difficult intubation [16]. Notably, this study further determined the Mallampati classification as “not a useful tool in classifying the difficult intubation in the ED”. This reasoning may explain why 10.2% of those surveyed indicated that their institution lacked a standard set of criteria to define a difficult airway (Figure 5b), leaving more clinical discretion to individual providers.
Beyond predictive value, the utility of set criteria for airway assessment should also consider the relative ease with which it can be applied in practice. In one study, Mallampati score, neck mobility, and thyromental distance were only able to be measured in one third of non-cardiac arrest ED intubations [17]. These findings parallel, and perhaps explain, how these same three criteria constituted three out of the four least used criteria among surveyed institutional protocols (Figure 5a: 39.4% Mallampati, 51.1% Neck Mobility, 32.1% Thyromental Distance). An additional element to consider in evaluating the use of these criteria is the observed lack of consistent knowledge of the tracking of trauma bay airway complications. In this survey, 34.3% of respondents indicated that they were unaware if their institutions tracked complications. This phenomenon complicates efforts to correlate the effects of protocol implementation on airway management outcomes.
This investigation also provides information on how different institutions may dictate the availability of physician anesthesiologists for airway management, even when they are not the primary service responsible. In nearly half of respondents’ surveys (48.1%), an anesthesia team member was reported to automatically come to the trauma bay for the highest priority traumas (Figure 1c). This lies in contrast to the 19.0% of respondents that reported that the anesthesia service is not always immediately available in their respective institutions (Figure 2b). The availability of the anesthesia team may explain different institutions’ handling of guidelines for when anesthesia need take over in the event of failed airway management by another service. In 38.7% of respondents’ institutions, anesthesia automatically takes over a failed airway and another 26.3% report that anesthesia may take over at the request of the emergency medical team (Figure 3a).
However, those contexts reported where anesthesia is not always readily available may relate to the 27.7% of respondents that report anesthesia does not take over in the event of a failed intubation by another team (Figure 3a). Putting the availability of anesthesia in the context of previously described literature, trauma patients with difficult airways presenting at off-hours has been found to independently correlate with endotracheal intubation-related adverse events [18].
Ono et al. attributed these findings to differences in staffing - at the institution of study, ‘back-ups’ for airway management, head and neck surgeons and anesthesiologists, are available immediately in-house during business hours, but are off-site during after regular operating hours [18].
Interestingly, the 2014 The American College of Surgeons Committee on Trauma requires Level I trauma centers to have the anesthesia service readily available at all times [19]. As such, this study may raise concerns for not delineating that anesthesiologists should also be available for emergent airway management, in addition to providing anesthesia services for the operating room.
Conclusion
This investigation has given insight into different components of airway management in the contemporary trauma setting. Given the unique emphasis on airway management in their training, physician anesthesiologists assume responsibility for such oversight in the operating room according to standardized protocols. While a similar reasoning traditionally placed airway management in the hands of anesthesiologists in the trauma bay as well, institutions have recently remodeled the role of anesthesiologists in this setting according to varied approaches. This survey confirmed that Emergency Medicine has taken on a great deal of responsibility in airway management in the trauma ward, consistent with other recent literature.
Future inquiry may benefit from further exploring these issues within a greater sample of physicians and institutions as well as expanding the context of investigation, such as to Level II and III trauma centers. Future investigation may also seek to correlate institutions’ different approaches to airway management outcomes, with the goal of isolating any possible factors contributing to differences in quality of healthcare. It is critically important to track airway complications, especially in a hospital location that often sees the most difficult intubating conditions due to the critical nature of patients in the trauma bay. Continuous assessment of the efficacy of protocols such as airway management is a necessary tool for quality improvement.
Abbreviations
ACGME- Accreditation Council for Graduate Medical Education; ED- Emergency Department; C- Collar- cervical collar; LEMON- Look, Evaluate the 3-3-2 rule, Mallampati score, Obstruction, and Neck mobility
Declarations
Ethics approval and consent to participate: Study approved by the Rutgers Newark Health Sciences IRB (Ref. Pro2018000849); Written informed consent obtained from all participants.
Consent for publication
Not applicable
Availability of data and material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
No outside funding for this study.
Authors' contributions
GT and MG contributed to the concept of this study. GT, MG, JS, NB, MZ, and GG contributed to the distribution of surveys, collection of data, analysis of data, interpretation of data, writing the paper and editing the manuscript.
Acknowledgements
Not applicable
Summary statement
This study involves the use of a survey of residency directors for anesthesiology, general surgery and emergency medicine to assess trends in airway management for patients presenting in the trauma ward.
Funding statement
No funding received
Conflicts of interest
The authors declare no competing interests.
Additional files
Survey Supplemental file 1. This file contains the survey utilized and distributed for this study via email and the use of Google Forms.
References
- Nolan J, Clancy M. Airway management in the emergency department. Br J Anaesth 88 (2002): 9-11.
- Stephens CT, Kahntroff S, Dutton RP. The success of emergency endotracheal intubation in trauma patients: a 10-year experience at a major adult trauma referral center. Anesth Analg 109 (2009): 866-872.
- Chiaghana C, Giordano C, Cobb D, et al. Emergency Department Airway Management Responsibilities in the United States. Anesth Analg 128 (2019): 296-301.
- Bushra JS, McNeil B, Wald DA, et al. A comparison of trauma intubations managed by anesthesiologists and emergency physicians. Acad Emerg Med 11 (2004): 66-70.
- Park L, Zeng I, Brainard A. Systematic review and meta-analysis of first-pass success rates in emergency department intubation: Creating a benchmark for emergency airway care. Emerg Med Australas 29 (2017): 40-47.
- Heidegger T, Gerig HJ, Henderson JJ. Strategies and algorithms for management of the difficult airway. Best Pract Res Clin Anaesthesiol 19 (2005): 661-674.
- Jenkins P, Rogers J, Kehoe A, et al. An evaluation of the use of a two-tiered trauma team activation system in a UK major trauma centre. Emerg Med J 32 (2015): 364-367.
- Plaisier BR, Meldon SW, Super DM, et al. Effectiveness of a 2-specialty, 2-tiered triage and trauma team activation protocol. Ann Emerg Med 32 (1998): 436-441.
- Thorsen K, Narvestad JK, Tjosevik KE, et al. Changing from a two-tiered to a one-tiered trauma team activation protocol: a before-after observational cohort study investigating the clinical impact of undertriage. Eur J Trauma Emerg Surg 12 (2021): 569-578.
- Surgeons ACo. 537 Verified Trauma Centers (2019).
- Omert L, Yeaney W, Mizikowski S, et al. Role of the emergency medicine physician in airway management of the trauma patient. J Trauma 51 (2001): 1065-1068.
- Varga S, Shupp JW, Maher D, et al. Trauma airway management: transition from anesthesia to emergency medicine. J Emerg Med 44 (2013): 1190-1195.
- Levitan RM, Rosenblatt B, Meiner EM, et al. Alternating day emergency medicine and anesthesia resident responsibility for management of the trauma airway: a study of laryngoscopy performance and intubation success. Ann Emerg Med 43 (2004): 48-53.
- Casey ZC, Smally AJ, Grant RJ, et al. Trauma intubations: can a protocol-driven approach be successful? J Trauma 63 (2007): 955-960.
- Jones JH, Weaver CS, Rusyniak DE, et al. Impact of emergency medicine faculty and an airway protocol on airway management. Acad Emerg Med 9 (2002): 1452-1456.
- Soyuncu S, Eken C, Cete Y, et al. Determination of difficult intubation in the ED. Am J Emerg Med 27 (2009): 905-910.
- Levitan RM, Everett WW, Ochroch EA. Limitations of difficult airway prediction in patients intubated in the emergency department. Ann Emerg Med 44 (2004): 307-313.
- Ono Y, Sugiyama T, Chida Y, et al. Association between off-hour presentation and endotracheal-intubation-related adverse events in trauma patients with a predicted difficult airway: A historical cohort study at a community emergency department in Japan. Scand J Trauma Resusc Emerg Med 24 (2016): 106.
- Banks SE, Sharp C, Fouche YL, et al. Considerations for anesthesia staffing in a trauma center: new standards, education, and safety. Curr Opin Anaesthesiol 28 (2015): 201-205.
Article Views: 507
Journal Statistics





Discover More: Recent Articles


