Correlation of Clinical Characteristics and Selective Biochemical Marker in Adolescent PCOS
Article Information
Nur-E-Nazma1*
1Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, Bangladesh
*Corresponding Author: Nur-E-Nazma, Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, Bangladesh.
Received: 16 October 2023; Accepted: 20 November 2023; Published: 28 November 2023
Citation: Nur-E-Nazma. Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, Bangladesh. Obstetrics and Gynecology Research. 6 (2023): 275-280.
View / Download Pdf Share at FacebookAbstract
Background:
It is fundamental to comprehend the incidence of polycystic ovarian syndrome (PCOS) worldwide because geographic and ethnic variations might significantly affect the clinical state. This study aims to measure the correlation between clinical characteristics and specific biochemical markers in adolescents with PCOS.
Methods:
A cross-sectional study was conducted in the Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, from January 2015 to December 2015. Ninety-five suspected cases of adolescent PCOS patients were selected using purposive sampling.
Results:
More than one-third (35.8%) of the patients belonged to the age group of 17-18 years; most of them were unmarried (92.6%) with normal BMI (52.6%). Among them, 70.5% had oligomenorrhoea, and 40% had hirsutism; the mean value of FSH, LH, and testosterone was 4.04±1.42, 9.92±5.57 (IU/liter), and 1.92±0.48 (nmol/L) respectively. About 65% of adolescents had normal fasting glucose/insulin ratio, but insulin resistance was found in 35% of the participants. Serum FSH was not significant (p=0.756) among the categories of menstrual abnormality, but serum LH (P=0.010) and LH/FSH ratios (P=0.014) had significant association among the patients with amenorrhoea and oligomenorrhoea. FSH 0.756, LH 0.010* LH/FSH 0.014*
Conclusion:
The study found that adolescents' serum LH and LH/FSH ratios were significantly higher with amenorrhoea and oligomenorrhoea. Among the participants, no statistically significant difference was noted in fasting insulin levels. However, the fasting glucose/insulin ratio was higher in individuals with neuropathic hemorrhagic compared to those with amenorrhea and oligomenorrhea.
Keywords
Polycystic ovary syndrome; Biochemical marker; Glycaemic status; Adolescent
Polycystic ovary syndrome articles Polycystic ovary syndrome Research articles Polycystic ovary syndrome review articles Polycystic ovary syndrome PubMed articles Polycystic ovary syndrome PubMed Central articles Polycystic ovary syndrome 2023 articles Polycystic ovary syndrome 2024 articles Polycystic ovary syndrome Scopus articles Polycystic ovary syndrome impact factor journals Polycystic ovary syndrome Scopus journals Polycystic ovary syndrome PubMed journals Polycystic ovary syndrome medical journals Polycystic ovary syndrome free journals Polycystic ovary syndrome best journals Polycystic ovary syndrome top journals Polycystic ovary syndrome free medical journals Polycystic ovary syndrome famous journals Polycystic ovary syndrome Google Scholar indexed journals Biochemical marker articles Biochemical marker Research articles Biochemical marker review articles Biochemical marker PubMed articles Biochemical marker PubMed Central articles Biochemical marker 2023 articles Biochemical marker 2024 articles Biochemical marker Scopus articles Biochemical marker impact factor journals Biochemical marker Scopus journals Biochemical marker PubMed journals Biochemical marker medical journals Biochemical marker free journals Biochemical marker best journals Biochemical marker top journals Biochemical marker free medical journals Biochemical marker famous journals Biochemical marker Google Scholar indexed journals Glycaemic status articles Glycaemic status Research articles Glycaemic status review articles Glycaemic status PubMed articles Glycaemic status PubMed Central articles Glycaemic status 2023 articles Glycaemic status 2024 articles Glycaemic status Scopus articles Glycaemic status impact factor journals Glycaemic status Scopus journals Glycaemic status PubMed journals Glycaemic status medical journals Glycaemic status free journals Glycaemic status best journals Glycaemic status top journals Glycaemic status free medical journals Glycaemic status famous journals Glycaemic status Google Scholar indexed journals Adolescent articles Adolescent Research articles Adolescent review articles Adolescent PubMed articles Adolescent PubMed Central articles Adolescent 2023 articles Adolescent 2024 articles Adolescent Scopus articles Adolescent impact factor journals Adolescent Scopus journals Adolescent PubMed journals Adolescent medical journals Adolescent free journals Adolescent best journals Adolescent top journals Adolescent free medical journals Adolescent famous journals Adolescent Google Scholar indexed journals endocrine disease articles endocrine disease Research articles endocrine disease review articles endocrine disease PubMed articles endocrine disease PubMed Central articles endocrine disease 2023 articles endocrine disease 2024 articles endocrine disease Scopus articles endocrine disease impact factor journals endocrine disease Scopus journals endocrine disease PubMed journals endocrine disease medical journals endocrine disease free journals endocrine disease best journals endocrine disease top journals endocrine disease free medical journals endocrine disease famous journals endocrine disease Google Scholar indexed journals reproductive age articles reproductive age Research articles reproductive age review articles reproductive age PubMed articles reproductive age PubMed Central articles reproductive age 2023 articles reproductive age 2024 articles reproductive age Scopus articles reproductive age impact factor journals reproductive age Scopus journals reproductive age PubMed journals reproductive age medical journals reproductive age free journals reproductive age best journals reproductive age top journals reproductive age free medical journals reproductive age famous journals reproductive age Google Scholar indexed journals infertility articles infertility Research articles infertility review articles infertility PubMed articles infertility PubMed Central articles infertility 2023 articles infertility 2024 articles infertility Scopus articles infertility impact factor journals infertility Scopus journals infertility PubMed journals infertility medical journals infertility free journals infertility best journals infertility top journals infertility free medical journals infertility famous journals infertility Google Scholar indexed journals oligomenorrhea articles oligomenorrhea Research articles oligomenorrhea review articles oligomenorrhea PubMed articles oligomenorrhea PubMed Central articles oligomenorrhea 2023 articles oligomenorrhea 2024 articles oligomenorrhea Scopus articles oligomenorrhea impact factor journals oligomenorrhea Scopus journals oligomenorrhea PubMed journals oligomenorrhea medical journals oligomenorrhea free journals oligomenorrhea best journals oligomenorrhea top journals oligomenorrhea free medical journals oligomenorrhea famous journals oligomenorrhea Google Scholar indexed journals hyperandrogenism articles hyperandrogenism Research articles hyperandrogenism review articles hyperandrogenism PubMed articles hyperandrogenism PubMed Central articles hyperandrogenism 2023 articles hyperandrogenism 2024 articles hyperandrogenism Scopus articles hyperandrogenism impact factor journals hyperandrogenism Scopus journals hyperandrogenism PubMed journals hyperandrogenism medical journals hyperandrogenism free journals hyperandrogenism best journals hyperandrogenism top journals hyperandrogenism free medical journals hyperandrogenism famous journals hyperandrogenism Google Scholar indexed journals polycystic ovaries articles polycystic ovaries Research articles polycystic ovaries review articles polycystic ovaries PubMed articles polycystic ovaries PubMed Central articles polycystic ovaries 2023 articles polycystic ovaries 2024 articles polycystic ovaries Scopus articles polycystic ovaries impact factor journals polycystic ovaries Scopus journals polycystic ovaries PubMed journals polycystic ovaries medical journals polycystic ovaries free journals polycystic ovaries best journals polycystic ovaries top journals polycystic ovaries free medical journals polycystic ovaries famous journals polycystic ovaries Google Scholar indexed journals
Article Details
Introduction
Polycystic ovarian syndrome (PCOS) is the greatest prevalent endocrine disease affecting women of reproductive age [5,16]. It is a complex disease in which endocrine, genetic, environmentally friendly, and behavioral factors interact to produce a diverse heterogenous phenotype with reproductive, metabolic, and psychological traits [8]. Principal clinical appearances of the disease include lengthy erratic menstrual bleeding, menstrual deformity, hirsutism, infertility or subfertility, amenorrhea, oligomenorrhea, oligo/anovulation, hyperandrogenism, and polycystic ovaries [11]. One of the common diagnoses for women with infertility is PCOS. According to a current meta-analysis, the prevalence of PCOS amongst adolescents was 11.04% grounded on the Rotterdam criteria, 3.39% based on the National Institutes of Health Criteria, and 8.03% based on the Androgen Excess and Polycystic Ovary Syndrome Society criteria [7]. In Bangladesh, the prevalence of PCOS was found in 6.11% of adolescents and 35.39% of infertile women [4]. PCOS has an autosomal dominant inheritance pattern, and there is a substantial genetic association between developing the condition. If one of a woman's family members has PCOS, there is often a 30–50% risk that she will also set it [13]. As per the World Health Organization (WHO), "adolescence" refers to the period between 10 to 19 years of age. Additionally, this age group includes individuals within a gynecological age of 8 years or less from the time of their menarche. Due to the confluence of typical pubertal physiological changes such as irregular menstrual cycles, acne, and polycystic ovarian morphology, pelvic ultrasound is the diagnostic criterion of adult PCOS. But the diagnostic criteria of PCOS in adolescents are both contentious and challenging [15]. Challenges include the threat of under-diagnosis, slow down and deprived diagnosis experiences, over-diagnosis, and the extra risk of using unpredictable nonevidence-based methods in the diagnosis and management of PCOS among specialists, general practitioners, along with associated health professionals [12]. More robust evidence is needed to overcome these challenges. The study helps determine the association between clinical manifestations and a particular biochemical marker in adolescent PCOS.
Methodology
A cross-sectional study was conducted in the Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, from January 2015 to December 2015. Ninety-five suspected cases of adolescent PCOS patients were selected according to standard criteria of PCOS from the OPD. A non-probability sampling technique called purposive sampling was used to select participants for the study. Data collection was carried out using a pre-tested semi-structured questionnaire. The study included adolescent patients aged between 13 and 19 years who presented with hyperandrogenism, hirsutism, acne, polycystic ovaries, acanthosis nigricans, oligomenorrhea/ amenorrhea, and obesity. Patients suffered from chronic/acute diseases such as genetic syndromes, coeliac disease, renal disease, liver or cardiac disease, undernourishment, or taking any drugs that could interfere with the hormone and metabolic functions, and those patients who refused to participate were excluded from the study. SPSS 26 version was used for statistical analysis. Frequencies and percentages documented the quantitative observation. The Chi-square test was used to analyze the categorical variables. Student t-test, ANOVA test was used to analyze the continuous variables, shown with mean and standard deviation. Ethical clearance was taken from The Local Ethical Committee of the Institute of Child and Mother Health, Matuail, Dhaka.
Results
It was observed that 35.8% respondents were in the age group 17-18 years, and 28.4% were 13-14 years old. The mean age was (mean±SD= 16±1.8) years. Among them, 92.6% were unmarried, and the rest of the (7.4%) participants were married. More than half (52.6%) of respondents had normal BMI, followed by (25.3%) who were obese. The mean BMI was (mean±SD= 24.3±3.4 (kg/m2). Figure 1 revealed the menstrual abnormality of the participants. Most adolescents with PCOS had oligomenorrhoea (70.5%), 15.8% amenorrhea & rest of the 13.7% participants had metropathia haemorrhagica. In clinical irregularity of the patients, the mass had (40%) hirsutism, and 14.7% had acne, 6.3% had obesity, and simply 3.2% had acanthosis nigricans (Figure 2). It was stated that, in ultrasonography, 10 to 12 quantities of follicles were found in 82(86.3%) cases, followed by 13(13.7%) cases where the follicle was found more than 12 in number. In ovarian volume ≤ 10cc was documented for 51(53.7%) cases while >10cc was narrated for 44(46.3%) cases. Normal stromal echo was revealed in 30(31.6%) study population, and hyperechoic was reported by 65(68.4%) of the study subjects. In the hormonal profile, the mean value of FSH was reported as 4.04±1.42 (IU/liter), mean LH was 9.92±5.57 (IU/liter), mean testosterone was 1.92±0.48 (nmol/L), 58(61.1%) participants were reported as LH/FSH ratio ≤2.0 and 37(38.9%) was LH/FSH ratio >2.0. Only sixty patients performed insulin resistance due to the high investigation cost. More than half, 32(53.3%) of the participants had normal fasting blood glucose levels (70-100mg/dl), and 20(33.3%) had normal fasting insulin levels (3-18 IU/L). Among 39 (65%) patients had a normal fasting glucose/insulin ratio, but insulin resistance was found in 21(35%) of the participants (Table 3). Serum FSH did not differ significantly (p=0.756) among different categories of menstrual abnormality, but serum LH (p=0.010), as well as LH/FSH ratio (p=0.014), were significantly high among patients with amenorrhoea and oligomenorrhoea. Mean testosterone was significantly (p=0.009) high in patients with Amenorrhoea and Metropathia haemorrhagica. There was no significant alteration observed in fasting insulin levels among the patients. However, the fasting glucose/insulin ratio (indicative of insulin resistance) was upper in individuals with oligomenorrhea and amenorrhea compared to those with neuropathic hemorrhagic (Table 4). Seven patients, 7(12.1%), had amenorrhoea in normal LH/FSH ratio and 8(21.6%) in altered LH/FSH ratio. Forty-one 41(70.7%) patients had oligomenorrhoea in normal LH/FSH ratio and 26(70.3%) in altered LH/FH ratio. In the case of Metropathia hemorrhagic, 10(17.2%) had normal LH/FSH ratio, and only 3(8.1%) in changed LH/FSH ratio. The change between the groups was not found to be statistically substantial (p>0.05) (Table 5).
|
Age (in years) |
Frequency |
Percentage |
|
13-14 |
27 |
28.4 |
|
15-16 |
26 |
27.4 |
|
17-18 |
34 |
35.8 |
|
>18 |
8 |
8.4 |
|
Mean±SD |
16±1.8 (13-19) |
|
|
Marital status |
||
|
Married |
7 |
7.4 |
|
Unmarried |
88 |
92.6 |
|
BMI (kg/m2) |
||
|
18.5-22.9 (Normal) |
50 |
52.6 |
|
23.0-26.9 (Overweight) |
21 |
22.1 |
|
≥27.0 (obese) |
24 |
25.3 |
|
Mean±SD |
24.3±3.4 (19.2-31.1) |
|
Table 1: The socio-demographic attributes of the study population (n=95) were examined
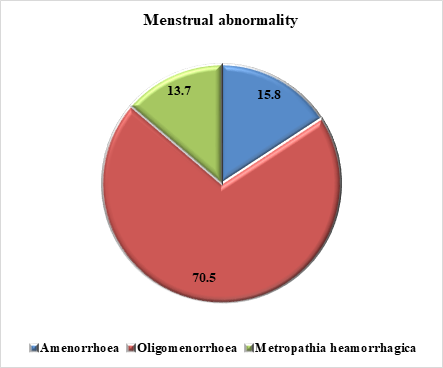
Figure 1: Menstrual abnormality of the study population (n=95)
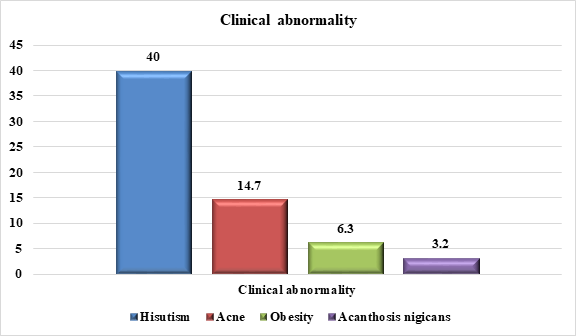
Figure 2: Clinical abnormality of the respondents (n=95)
|
Diagnostic procedure |
Frequency |
Percentage |
|
No of follicles (in ultrasonography) |
||
|
12-Oct |
82 |
86.3 |
|
>12 |
13 |
13.7 |
|
Ovarian volume |
||
|
≤ 10cc |
51 |
53.7 |
|
>10cc |
44 |
46.3 |
|
Stromal echo |
||
|
Normal |
30 |
31.6 |
|
Hyperechoic |
65 |
68.4 |
|
Hormonal profile |
||
|
Mean ±SD |
||
|
FSH (IU/liter) |
4.04±1.42(2.15-8) |
|
|
LH (IU/liter) |
9.92±5.57(2.2-21.4) |
|
|
Testosterone (nmol/L) |
1.92±0.48 (1.1-3.1) |
|
|
LH/FSH ratio |
||
|
≤2.0 |
58 |
61.1 |
|
>2.0 |
37 |
38.9 |
Table 2: Different diagnostic procedures for PCOS (n=95)
|
Fasting Blood glucose (mg/dl) |
Frequency |
Percentage |
|
70-100 (normal) |
32 |
53.3 |
|
>100 |
28 |
46.7 |
|
Fasting insulin (IU/L) |
||
|
3-18 (normal) |
20 |
33.3 |
|
>18 |
40 |
66.7 |
|
Fasting glucose/insulin ratio |
||
|
Normal (≥4.5) |
39 |
65 |
|
Insulin resistance (<4.5) |
21 |
35 |
Table 3: Glycaemic status of the study population (n=60)
|
Parameter |
Menstrual abnormality |
P-value |
||
|
Amenorrhoea (n=15) |
Oligomenorrhoea (n=67) |
Metropathia hemorrhagic (n=13) |
||
|
FSH (IU/L) |
3.96±1.3 |
4.07±1.28 |
4.31±1.19 |
0.756 |
|
LH (IU/L) |
10.06±4.55 |
7.97±3.58 |
5.73±2.86 |
0.010* |
|
LH/FSH ratio |
2.67±1.23 |
2.11±1.10 |
1.44±0.84 |
0.014 * |
|
Testosterone (nmol/L) |
2.12±0.66 |
1.78±0.34 |
2.0±0.42 |
0.009 * |
|
Fasting insulin (IU/L) |
19.93±2.28 |
18.94±3.78 |
20.61±1.71 |
0.324 |
|
Fasting glucose/ insulin ratio |
5.27±1.08 |
5.68±1.26 |
4.06±0.27 |
0.001* |
*= Significant, p-value=<0.05 was the level of significance.
Table 4: Hormonal levels among the participants with different menstrual abnormality (n=95)
|
Menstrual abnormality |
LH/FSH ratio |
||||
|
≤2.0 (Normal) (n=58) |
>2.0 (Altered) (n=37) |
P-value |
|||
|
N |
% |
N |
% |
||
|
Amenorrhoea |
7 |
12.1 |
8 |
21.6 |
0.261 |
|
Oligomenorrhoea |
41 |
70.7 |
26 |
70.3 |
|
|
Metropathia haemorrhagica |
10 |
17.2 |
3 |
8.1 |
|
p-value was observed from χ2test
Table 5: Association of LH/FSH ratio with menstrual abnormality (n=65)
Discussion
PCOS is the main public health concern among adolescents. In this study, 95 adolescent with PCOS were nominated to control the association among PCOS patients' clinical appearance and biochemical markers. In the present study, majority of the participants (35.8%) fit to the age cluster 17-18 years with mean age was (mean±SD=16±1.8) years. Similar study was conducted by Shawna B Christensen et al. showed that the Adolescent's mean age was (mean±SD=17.7 ± 1.4) years [2]. In a study in the USA carried out by Kansra and Marquart, explored that the mean age was (mean±SD=15.5 ± 1.9) years. [1]. Both results were similar to the present study. Maximum adolescent women in the present study (92.6%) were unmarried. In an Indian study by Fauzia Tabassum & colleagues, a related result was revealed when most PCOS women were unmarried [14]. In the present study, most adolescent women (52.6%) had normal BMI, and 25.3% of participants had obesity. A study in Southern California revealed different findings where most adolescents were obese [2]. Among the participants of the present study, menstrual abnormality was quite common. A similar result was narrated in a study in Greece, where 72.2% of participants suffered from menstrual cycle disorders [3]. In the study, 40% of participants had hirsutism, followed by acne (14.7%). A prospective observational study found that 36% of the study population had androgenetic alopecia followed by acne (56.4%) [3]. The findings correlated with the present study. In the present study, follicles were the most common feature in ultrasonography, and less than ≤ 10 ccs ovarian volume was most commonly recorded 51(53.7%). Different results were observed in a study conducted in the Departments of Obstetrics and Gynecology of Hippokration Hospital in Thessaloniki, Greece, where the mean ovarian follicle was documented as 11.1 ± 4.9 and mean ovarian volume was recorded at 7.9 ± 3.6 among the participants [10]. The mean value of FSH was reported as 4.04±1.42 (IU/liter), LH was 9.92±5.57 (IU/liter), and testosterone was 1.92±0.48 (nmol/L) in the present study. A relatable result was revealed in a study where the mean FSH was 5.9 ± 2.2, LH was 6.9 ± 4.3, and testosterone was 1.98 (nmol/L) [3]. In the current study, average fasting blood glucose level (70-100mg/dl) was observed among 32(53.3%) participants, while 20(33.3%) PCOS adolescents had normal fasting insulin level (3-18 IU/L), usual fasting glucose/insulin ratio was reported among 65%. Insulin resistance was documented in 21(35%) participants. A different result was carried out in the gynecology and fertility clinic in Maternity Education Hospital In the Kurdish city of Erbil, Iraq, which indicated in their study that mean fasting insulin was (μU/ml) 15.98 ± 10.12, mean fasting glucose/ insulin ratio 7.74 ± 5.24, insulin resistance was shown in 112 (42.6%) of the PCOS women and no significant changes in the rate of insulin resistance and the PCOS phenotypes [6]. In the current study, no significant difference was observed in fasting insulin level, but fasting glucose/insulin ratio (insulin resistance) was higher among menstrual abnormality patients. Vasiliki Christodoulopoulou and colleagues observed dissimilar results that glucose displayed the strongest association with menstrual status [3]. In the present study, Serum FSH did not differ significantly among the different categories of menstrual abnormality, but serum LH and LH/FSH ratios were significantly high among PCOS patients. Another study found similar findings where significantly higher levels of LH in women with menstrual disorders were documented associated to individuals with normal menstrual cycles. Fasting glucose was also significantly more elevated among these patients [3]. In the present study, no statistically significant connection was establish between LH/FSH ratio and menstrual abnormality. Another study similarly observed that there was a significant difference in terms of the LH/FSH ratio among women with PCOS. The results also recommended that patients with PCOS therapy have bring down hyperinsulinemia and insulin resistance. There was also a significant correlation between hormone levels and LH/FSH ratio in their study participants [9].
Limitations of the study:
- The study's small sample size may boundary the generalizability of its results.
- The cross-sectional study strategy was the decrepit observational design.
Conclusion and Recommendations
The results of the study indicate that LH and LH/FSH ratios could serve as valuable markers to assess the severity of PCOS in adolescents. Nonetheless, supplementary research is necessary to validate these findings and identify the most optimal biochemical markers for the diagnosis and treatment of PCOS in this age group. Additional research is desirable to investigate the role of insulin resistance in the growth of neuropathic hemorrhage in youngsters with PCOS. Future research should use a longitudinal design to examine the association between clinical manifestations and biochemical markers in adolescents with PCOS. The study found that serum LH and LH/FSH ratios were significantly higher with amenorrhoea and oligomenorrhoea among adolescents. There was no significant change noticed in fasting insulin stages among the respondents. Nevertheless, the fasting glucose/insulin ratio (symptomatic of insulin resistance) was higher in individuals with neuropathic hemorrhagic compared to those with amenorrhea and oligomenorrhea.
Conflict of Interests:
The Author declare no conflicts of interests.
Funding:
None
Acknowledgments:
We express our open gratitude and gratefulness to all the individuals who have significantly completed this research. Our heartfelt thanks go to the Department of Obstetrics & Gynaecology, Institute of Child and Mother Health, Matuail, Dhaka, Bangladesh, for their invaluable support and provision of necessary facilities, which significantly contributed to the execution of this study. We extend our heartfelt gratitude to the study participants, as their cooperation and involvement were essential in facilitating the success of this research.
References
- AR, K., & K, M. (2016). Comparison of Clinical and Biochemical Parameters in Adolescent Girls with Polycystic Ovary Syndrome in Different Clinical Settings. Journal of Women's Health Care 5 (2016): 2-5.
- Christensen, S. B., Black, M. H., Smith, et al. Prevalence of polycystic ovary syndrome in adolescents. Fertility and Sterility, 100 (2013): 470–477.
- Christodoulopoulou, V., Trakakis, E., Pergialiotis, V., et al. Clinical and biochemical characteristics in PCOS women with menstrual abnormalities. Journal of Family and Reproductive Health, 10 (2016): 184-190.
- Fatema, K., Das, T. R., Kazal, R. K., et al. Prevalence and characteristics of polycystic ovarian syndrome in women attending in outpatient department of obstetrics and gynecology of Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 10 (2021): 830.
- Guo, Z., Jin, F., Chen, S., et al. Correlation between biochemical and clinical hyperandrogenism parameter in polycystic ovary syndrome in relation to age. BMC Endocrine Disorders, 23 (2023): 89.
- Jamil, A.S., Alalaf, S.K., Al-Tawil, N.G., et al. A case-control observational study of insulin resistance and metabolic syndrome among the four phenotypes of polycystic ovary syndrome based on Rotterdam criteria Female Fertility. Reproductive Health, 12 (2015): 1-9.
- Kamrul-Hasan, A.B.M., Aalpona, F.T.Z., & Selim, S. Clinical, metabolic and hormonal profiles of bangladeshi adolescents with polycystic ovary syndrome. European Endocrinology, 1 (2021), 54-58.
- Louwers, Y.V., & Laven, J.S.E. Characteristics of polycystic ovary syndrome throughout life. Therapeutic Advances in Reproductive Health, 14 (2020): 263349412091103.
- Mitrašinovic-Brulic, M., Buljan, M., & Suljevic, D. Association of LH/FSH ratio with menstrual cycle regularity and clinical features of patients with polycystic ovary syndrome. Middle East Fertility Society Journal 1 (2021).
- Panidis, D., Tziomalos, K., Papadakis, E., et al. Uterine volume and endometrial thickness in the early follicular phase in patients with polycystic ovary syndrome. Endocrine Practice 20 (2014): 540-547.
- Ranathunga, I., Athukorala, T.G., Sumanatilleke, M.R., et al. Evaluation of socio-demographic and clinical characteristics of PCOS patients attending a tertiary care institute in Colombo. BMC Endocrine Disorders 22 (2022): 1-10.
- Sebastian, M. R., Wiemann, C. M., Bacha, F., et al. Diagnostic Evaluation, Comorbidity Screening, and Treatment of Polycystic Ovary Syndrome in Adolescents in 3 Specialty Clinics. Journal of Pediatric and Adolescent Gynecology 31 (2018): 367-371.
- Sharif, E. New markers for the detection of polycystic ovary syndrome. Obstetrics & Gynecology International Journal, 10(2019): 257–268.
- Tabassum, F., Jyoti, C., Sinha, H.H., et al. Impact of polycystic ovary syndrome on quality of life of women in correlation to age, basal metabolic index, education and marriage. PLOS ONE, 16 (2021): e0247486.
- Teede, H.J., Misso, M.L., Costello, M.F., et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Clinical Endocrinology, 89 (2018): 251-268.
- Tehrani, F.R., & Amiri, M. Polycystic ovary syndrome in adolescents: Challenges in diagnosis and treatment. International Journal of Endocrinology and Metabolism 17 (2019).
- Upadhya, J.P., Rai, S., & Acharya, S.V. Study of clinical characteristics of women with polycystic ovarian syndrome. International Journal of Reproduction, Contraception, Obstetrics and Gynecology, 9 (2020): 2424.


 Impact Factor: * 3.2
Impact Factor: * 3.2 CiteScore: 2.9
CiteScore: 2.9  Acceptance Rate: 11.01%
Acceptance Rate: 11.01%  Time to first decision: 10.4 days
Time to first decision: 10.4 days  Time from article received to acceptance: 2-3 weeks
Time from article received to acceptance: 2-3 weeks 