Cognitive behaviour therapy for adolescents with eating disorders: An effective alternative to the disease-based treatments
Riccardo Dalle Grave , Simona Calugi
Department of Eating and Weight Disorders, Villa Garda Hospital, Garda (VR), Italy
Abstract
Several clinical services offer eclectic multidisciplinary treatments with no evidence of efficacy and effectiveness for adolescents with eating disorders. These treatments are usually based on the ‘disease model’ of eating disorders. The model postulates that eating disorders are the result of a specific disease (i.e., anorexia nervosa, bulimia nervosa or other eating disorders), and patients are considered not to have control of their illness. Therefore, they need the external control of parents and/or health professionals. In this model, the patients adopt a passive role in the treatment. On the contrary, enhanced cognitive behaviour therapy (CBT-E) for adolescents is based on a ‘psychological model’ of eating disorders. Patients are helped to understand the psychological mechanisms that maintain their eating disorder and are ‘actively’ involved in the recovery process. Clinical studies showed that more than 60% of adolescent patients who complete the treatment achieve a full response at 12-month follow-up. The treatment is well accepted by young people and their parents, and its collaborative nature is well suited to ambivalent young patients who may be particularly concerned about control issues and for parents who cannot participate in all treatment sessions.
Keywords
Anorexia nervosa
Bulimia nervosa
Eating disorders
Treatment
Cognitive behaviour
Therapy
Family-based treatment
Multidisciplinary treatment
Outcome
Adolescents
Introduction
Eating disorders may have a profound negative effect on the psychosocial functioning and physical health of adolescents. Therefore, they must be treated early and effectively to avoid long-lasting and sometimes devastating adverse effects (Flynn et al., 2021). To date, most Italian clinical services for adolescents use an eclectic multidisciplinary treatment that, although recommended by the Italian recommendations of the Ministry of Health (Ruocco et al., 2017), has no evidence of efficacy and effectiveness. As the term itself says, the eclectic multidisciplinary interventions involve several professionals (usually child neuropsychiatrist, pediatrician, dietitian/nutritionist, psychologist) who do not follow a common theoretical model. Indeed, they typically deliver specific procedures and recommendations to pursue their professional role’s specific objective, often with discrepancies between them.On the other hand, there are treatments for adolescents with good empirical support, which Italian eating disorder professionals rarely use. The most relevant are a specific form of family therapy, termed “family-based treatment (FBT)” (Lock & Le Grange, 2013) and enhanced cognitive behavioral therapy (CBT-E) (Dalle Grave & Calugi, 2020).
The adoption of evidence-based treatments has several advantages for clinicians, clinical services, and patients. They are safe, consistent, and cost-effective (Pope, 2003).
Clinicians applying these treatments provides the patients and their families the best existing evidence treatment available while simultaneously offering the flexibility to individualize treatment (Cook, Schwartz, & Kaslow, 2017). Furthermore, knowing how many patients can achieve remission from the eating disorder helps to identify the limits of the treatment and, therefore, offers clinicians and researchers a starting point to develop complex treatment plans (Roberts & Yeager, 2004).
FBT is considered the most empirically supported
intervention for adolescents with anorexia nervosa. There is also some more limited support for its use in young people with other eating disorders. However, FBT has certain limitations. All families and patients do not embrace it because it requires parents to participate in sessions and control their child’s eating. It is also labour intensive and, most of all, less than 50% of young patients achieve full recovery (Lock et al., 2010). These considerations indicate that alternative approaches are needed.
The National Institute for Health and Care Excellence (NICE) has recommended cognitive behaviour therapy (CBT) for eating disorders in children and young people when family therapy is unacceptable, contraindicated, or ineffective (National Guideline Alliance, 2017). The recommendation was mainly based on reviewing the promising results achieved by the enhanced version of CBT (CBT-E) adapted for adolescents with eating disorders aged 11 to 19 years (Dalle Grave, Conti, Sartirana, Sermattei, & Calugi, 2021). As we will explain in this paper, the standard multidisciplinary models and FBT are based, albeit in different ways, on a classic “disease model” of the eating disorder. In contrast, CBT-E, starting from a different theoretical conceptualization, is based on a pure “psychological model”.
The origin of CBT-E for adolescents
CBT-E was initially developed to treat adults with eating disorders at the Centre for Research on Eating Disorders at Oxford (CREDO) (Fairburn, Cooper, & Shafran, 2003). CBT-E has been defined as “enhanced” because it uses a variety of innovative strategies and procedures to enhance the effectiveness of the original CBT for bulimia nervosa and addresses the psychopathology of eating disorders rather than a specific diagnosis of eating disorders. CBT-E has been evaluated in several clinical trials and is recommended by international guidelines for the treatment of all clinical forms of eating disorders in adults (National Guideline Alliance, 2017).
The idea of adapting CBT-E for the treatment of adolescents was raised ten years ago at the Department of Eating and Weight Disorders of Villa Garda Hospital, Italy, during a periodic supervision visit by Professor Fairburn, the undisputed “father” of CBT for eating disorders. Two main clinical observations led us to undertake this project. First, since young patients with eating disorders show the same specific psychopathology (i.e., overvaluation of shape and weight, strict dieting, excessive exercising, binge eating, and purging) of adults, they could benefit from CBT-E, a treatment specifically designed to address the psychopathology of eating disorders. Second, although young patients are often in an egosyntonic phase of their disorder, they can be actively engaged in individual psychological treatment, as my colleagues and I observed in many years of clinical practice.
Main adaptations of CBT-E for adolescents
CBT-E for adolescents was adapted considering three distinctive characteristics of young patients with eating disorders (Dalle Grave & Calugi, 2020). First, some medical complications associated with eating disorders (e.g., osteopenia and osteoporosis) are particularly severe in this age range, and periodic medical assessments and a lower threshold for hospital admission are integral parts of CBT-E for adolescents. Second, a particular effort is made to engage the young patient in treatment and change, as they are often unaware that they have a problem to address. Third, in most cases, parents need to be involved in treatment, given the age and circumstances of these patients.
CBT-E for adolescents with eating disorders: An overview
Structure
CBT-E for adolescents involves two assessment/preparatory sessions followed by three main steps, one or more review sessions, and three post-review sessions (see Figure 1). Treatment lasts 20 weeks in not underweight patients, while in underweight patients, the standard 40 weeks of adult CBT-E may be shortened to about 30 weeks, as adolescents tend to restore a normal body weight faster than adults (Calugi, Dalle Grave, Sartirana, & Fairburn, 2015). Parents are asked to participate alone in an interview lasting approximately 90 minutes during the first week of treatment. Subsequently, the patient and the parents are seen together in six to eight joint sessions of 15 to 20 minutes immediately after a patient session.
General treatment strategy
After the assessment, the patients are taught about the two main ways of understanding eating disorders, namely the so-called “disease” and “psychological” models, and the treatment approaches based upon them. Specifically:
- The disease model postulates that the characteristics of the eating disorder are the result of a specific disease (i.e., anorexia nervosa, bulimia nervosa, or other eating disorders). Therefore, a key strategy of the treatment is the “externalization” of the eating disorders with the aim to help patients to perceive the illness as a separate entity form them (Voswinkel, Rijkers, van Delden, & van Elburg, 2021). The patients are considered not to be in control of their illness and, thus, they need the external control of parents, as in FBT (Dalle Grave, Eckhardt, Calugi, & Le Grange, 2019), and/or health professionals, as in multidisciplinary treatments eclectic for adolescents. In this model, the patients adopt a passive role in the treatment.
- The psychological model adopted by CBT-E is based on a psychological explanation of the patient’s eating disorder; specifically, the young person has difficulties seeing dieting and low weight as a problem because their self-evaluation scheme is predominantly based on shape, weight, eating and their control (Fairburn et al., 2003). This explains why being able to diet and achieving a low weight is often associated with a sense of realization, despite its negative consequences. However, according to this stance, patients can be helped to understand the psychological mechanisms maintaining their eating disorder and that their self-evaluation system is dysfunctional. They can ‘actively’ decide to find other, more functional solutions for reaching a stable and balanced self-evaluation scheme and, therefore, recover from their eating disorder (Dalle Grave & Calugi, 2020).
The psychological model adopted by CBT-E explains why treatment never asks the patient to do things they do not agree to do because this may increase their resistance to change (Dalle Grave & Calugi, 2020). For example, in the two assessment/preparation sessions, patients are asked to think about the pros and cons of starting Step One (not to change) for having the opportunity to improve the understanding of the psychological function and maintenance mechanisms of their eating problem and to reach a better position to evaluate the implication to change. Furthermore, the goal of Step One of CBT-E for low-weight patients is not weight regain but to help them understand the psychological nature of their eating problem and actively decide to address weight regain. This strategy is also used to address other egosyntonic features of eating-disorder psychopathology (e.g., dietary restraint, excessive exercising). To this end, a key strategy of CBT-E is to collaboratively create with patients a personalized formulation of the main processes that maintain their eating problem, which will become the target of treatment (see Figure 2). The patients are educated about the processes reported on the formulation and are actively involved in addressing each of them. If they do not conclude that they have a problem to address, treatment cannot start or must be postponed for a time, but this is not a common occurrence.
Once the patient is engaged, they are encouraged to observe how the processes in their formulation operate in real life. For this purpose, they are asked to monitor in real-time their eating, and events, thoughts, and feelings that have influenced eating. Then, they are asked if they agree to make gradual behavioural changes and analyse the associated effects and implications on their way of thinking. This approach usually produces a gradual reduction in their shape, weight, and eating concerns. In the later stages of the treatment, when the main maintenance processes have been disrupted, and the patient reports experiencing periods free from shape, weight and eating concerns, the treatment focuses on helping them to recognize the early warning signs of eating-disorder mindset reactivation, and to de-centre from it quickly, thereby averting relapse.
Parents of adolescent patients are actively involved in creating an optimal family environment to facilitate the patient’s change and, in agreement with the young person, support them in implementing some procedures of CBT-E.
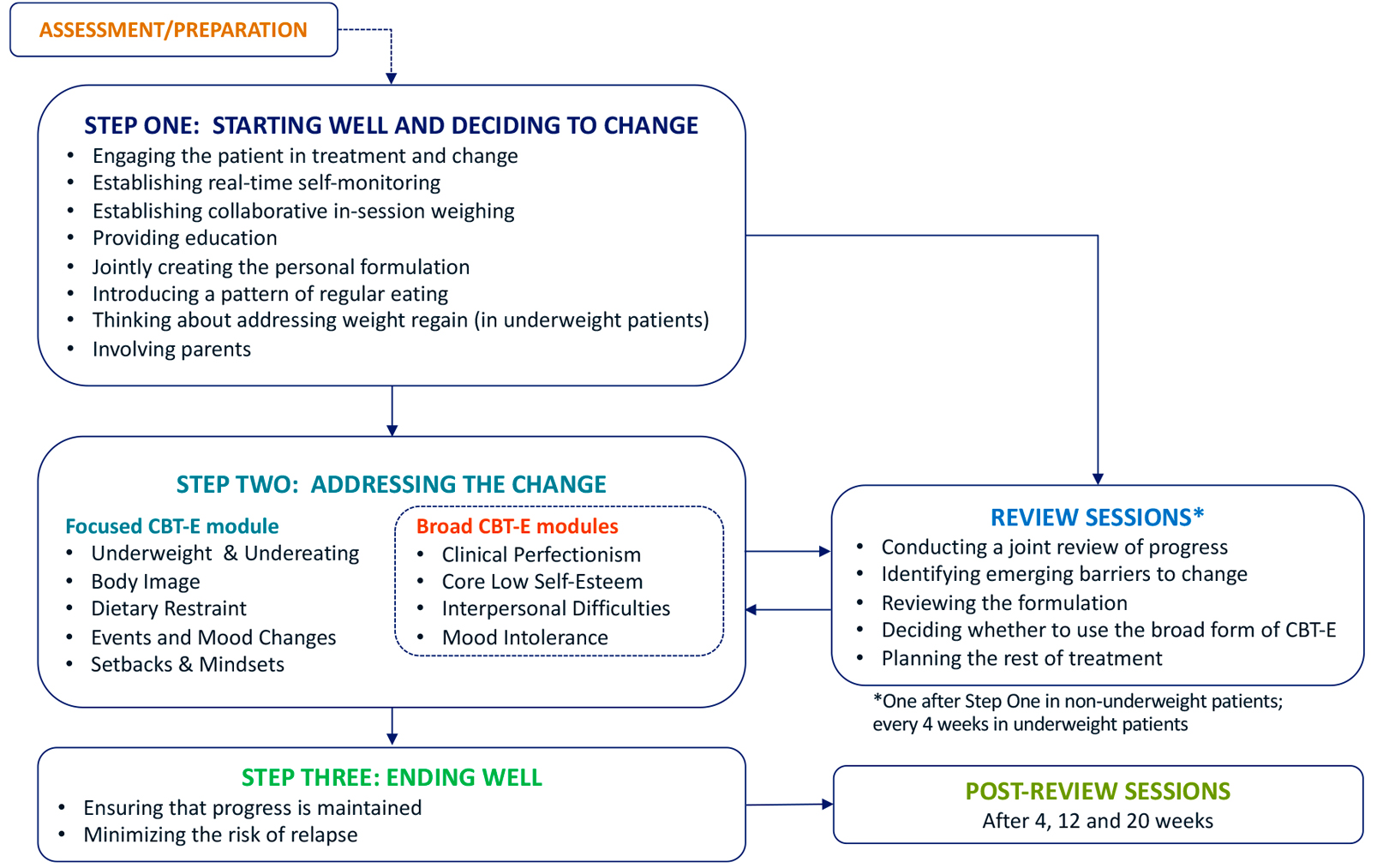
Figure 1. The CBT-E map for adolescents with eating disorders
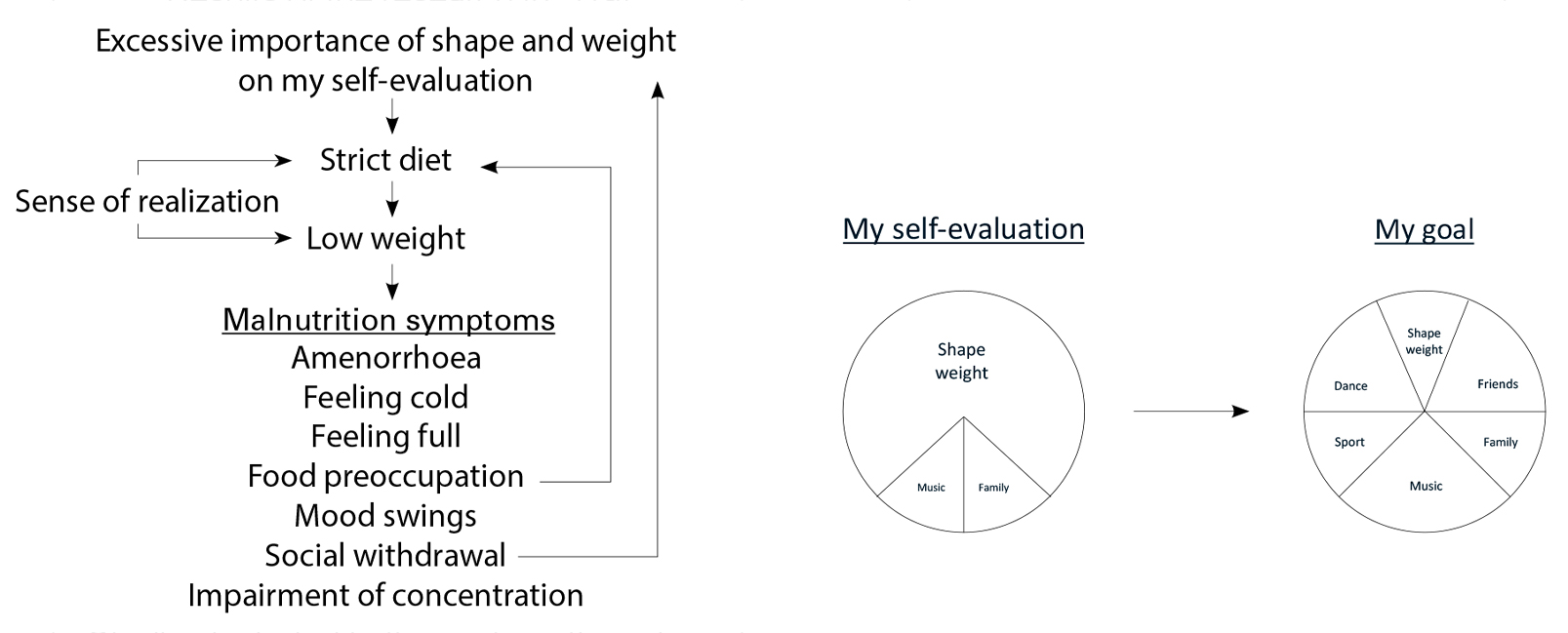
Figure 2. The personal formulation of a young patient with anorexia nervosa treated with CBT-E
How effective is CBT-E for adolescents?
To date, four different cohort studies in patients between 11 and 19 years of age evaluated the effectiveness of CBT-E for adolescents (Calugi et al., 2015; Dalle Grave, Calugi, Doll, & Fairburn, 2013; Dalle Grave, Calugi, Sartirana, & Fairburn, 2015; Dalle Grave, Sartirana, & Calugi, 2019). About 72% of patients with anorexia nervosa completed outpatient CBT-E, and among completers, about 62% displayed a full response at follow-up. A recent not randomized effective effectiveness trial found that the CBT-E outcome was similar to FBT at 6 and 12 months of follow-up (Le Grange et al., 2020).
Comparably encouraging results have also been achieved when delivering treatment in real-world clinical settings (Dalle Grave, Sartirana, et al., 2019). Finally, approximately 70% of non-underweight patients displayed minimal residual eating disorder psychopathology, and half of those with previous episodes of binge eating or purging reported no longer having them (Dalle Grave et al., 2015).
Conclusions
CBT-E is a promising treatment for adolescents with eating disorders. It has several clinical advantages. It is acceptable to young people and their parents. Its collaborative nature is well suited to ambivalent young patients who may be particularly concerned about control issues and to parents who cannot participate in all treatment sessions. The transdiagnostic scope of treatment is an advantage as it allows to treat the full range of disorders that occur in adolescent patients. In conclusion, CBT-E provides a strong effective alternative to FBT and multidisciplinary eclectic treatments based on the disease model.
References
Calugi, S., Dalle Grave, R., Sartirana, M., & Fairburn, C. G. (2015). Time to restore body weight in adults and adolescents receiving cognitive behaviour therapy for anorexia nervosa. Journal of Eating Disorders, 3, 21. doi:10.1186/s40337-015-0057-z
Cook, S. C., Schwartz, A. C., & Kaslow, N. J. (2017). Evidence-based psychotherapy: advantages and challenges. Neurotherapeutics, 14(3), 537-545. doi:10.1007/s13311-017-0549-4
Dalle Grave, R., & Calugi, S. (2020). Cognitive behavior therapy for adolescents with eating disorders. New York: Guilford Press.
Dalle Grave, R., Calugi, S., Doll, H. A., & Fairburn, C. G. (2013). Enhanced cognitive behaviour therapy for adolescents with anorexia nervosa: an alternative to family therapy? Behaviour Research and Therapy, 51(1), R9-R12. doi:10.1016/j.brat.2012.09.008
Dalle Grave, R., Calugi, S., Sartirana, M., & Fairburn, C. G. (2015). Transdiagnostic cognitive behaviour therapy for adolescents with an eating disorder who are not underweight. Behaviour Research and Therapy, 73, 79-82. doi:10.1016/j.brat.2015.07.014
Dalle Grave, R., Conti, M., Sartirana, M., Sermattei, S., & Calugi, S. (2021). Enhanced cognitive behaviour therapy for adolescents with eating disorders: a systematic review of current status and future perspectives. IJEDO, 3, 1-11. doi:10.32044/ijedo.2021.01
Dalle Grave, R., Eckhardt, S., Calugi, S., & Le Grange, D. (2019). A conceptual comparison of family-based treatment and enhanced cognitive behavior therapy in the treatment of adolescents with eating disorders. Journal of Eating Disorders, 7(1), 42. doi:10.1186/s40337-019-0275-x
Dalle Grave, R., Sartirana, M., & Calugi, S. (2019). Enhanced cognitive behavioral therapy for adolescents with anorexia nervosa: outcomes and predictors of change in a real-world setting. International Journal of Eating Disorders, 52(9), 1042-1046. doi:10.1002/eat.23122
Fairburn, C. G., Cooper, Z., & Shafran, R. (2003). Cognitive behaviour therapy for eating disorders: a “transdiagnostic” theory and treatment. Behaviour Research and Therapy, 41(5), 509-528. doi:10.1016/s0005-7967(02)00088-8
Flynn, M., Austin, A., Lang, K., Allen, K., Bassi, R., Brady, G., . . . Schmidt, U. (2021). Assessing the impact of First Episode Rapid Early Intervention for Eating Disorders on duration of untreated eating disorder: a multi-centre quasi-experimental study. European Eating Disorders Review, 29(3), 458-471. doi:10.1002/erv.2797
Le Grange, D., Eckhardt, S., Dalle Grave, R., Crosby, R. D., Peterson, C. B., Keery, H., . . . Martell, C. (2020). Enhanced cognitive-behavior therapy and family-based treatment for adolescents with an eating disorder: a non-randomized effectiveness trial. Psychological Medicine, 1-11. doi:10.1017/s0033291720004407
Lock, J., & Le Grange, D. (2013). Treatment manual for anorexia nervosa: a family-based approach (2nd ed.). New York: Guilford Press.
Lock, J., Le Grange, D., Agras, W. S., Moye, A., Bryson, S. W., & Jo, B. (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Archives of General Psychiatry, 67(10), 1025-1032. doi:10.1001/archgenpsychiatry.2010.128
National Guideline Alliance. (2017). Eating disorders: recognition and treatment. London: National Institute for Health and Care Excellence (UK); 2017 May. (NICE Guideline, No. 69.) London.
Pope, C. (2003). Resisting Evidence: The study of evidence-based medicine as a contemporary social movement. Health, 7(3), 267-282. doi:10.1177/1363459303007003002
Roberts, A. R., & Yeager, K. R. (2004). Evidence-based practice manual. New York: Oxford University Press.
Ruocco, G., Andrioli Stagno, R., Ballardini, D., Cotugno, A., Dalla Ragione, L., Dalle Grave, R., . . . Vincenzi, M. (2017). Linee di indirizzo nazionali per la riabilitazione nutrizionale nei disturbi dell’alimentazione. Quaderni del Ministero della Salute, 29.
Voswinkel, M. M., Rijkers, C., van Delden, J. J. M., & van Elburg, A. A. (2021). Externalizing your eating disorder: a qualitative interview study. Journal of Eating Disorders, 9(1), 128. doi:10.1186/s40337-021-00486-6