Mindfulness as a tool for reducing stress in healthcare professionals: An umbrella review
Abstract
BACKGROUND:
Health care providers (HCPs) and health care students experience a huge amount of stress due to high workloads and pressure to perform and are likely to develop anxiety, depression and burnout.
OBJECTIVE:
The objective was to carry out an umbrella review of systematic and narrative reviews on the effectiveness of mindfulness-based interventions in reducing stress and improving well-being in HCPs and health care students.
METHODS:
Systematic and narrative reviews that examined the impact of mindfulness-based interventions on HCPs and healthcare students’ perceived stress were identified through a systematic search of three electronic databases: PubMed, Scopus and Web of Science.
RESULTS:
Fifteen articles were included in the analysis: eleven systematic and four narrative reviews. Studies’ quality varied from critically low to high. The different interventions showed positive results in reducing stress in both HCPs and students, with mindfulness-based stress reduction (MBSR) course having the major impact.
CONCLUSIONS:
MBSR techniques and other mindfulness based interventions resulted to be potentially effective in reducing stress. However, despite the vast amount of data collected by the studies and the promising results, several limitations affected the validity of the studies. Therefore, more research that considers the critical aspects of this field is required, in order to provide more reliable results.
1Introduction
Health care providers (HCPs) are particularly exposed to various determinants of work-related stress [1, 2]. Usually, they face with organizational issues, diagnostic and therapeutic duties, as well as have to face the suffering of people on a daily basis [3]. All these aspects are associated with the development of a progressive physical and psychological stressful status of HCPs, which consequently makes them more likely to develop anxiety, depression and burnout [4–6]. This can negatively have an impact on both patients and healthcare systems, by causing medical errors, longer patient hospital stay, and poorer patient care [7]. Attention has also been paid to healthcare students since they have to maintain clinical tasks and academic standards. These two stressors can affect their competency acquisition, and lead to depression and anxiety [8, 9]. In response to these concerns, several health and educational organizations started seeking possible solutions and strategies to reduce HCPs’ and healthcare students’ stress levels, as well as to improve well-being. One such strategy is mindfulness, through which HCPs and healthcare students learn to be purposefully alert and attentive to the present moment and to self-observe in an objective and detached manner. The first mindfulness intervention to be clinically evaluated was the mindfulness-based stress reduction (MBSR), a program that incorporates many types of meditation techniques and yoga postures [10, 11]. In recent years, other types of mindfulness-based interventions (MBIs) and meditation were evaluated. Results were promising, with most interventions showing a decrease in HCPs’ anxiety, depression, stress, and burnout symptoms [12, 13]; some studies also analysed indirect elements, highlighting positive results for example on patients’ satisfaction [13, 14]. There is evidence, based on systematic reviews already published, that MBSR and MBI interventions are useful tools able to reduce perceived stress symptoms, to improve mental health outcomes [9, 10, 15, 16] and positive results are reported on the prevention of burnout syndrome [17].
However, in many cases, several limitations do not allow studies providing statistically reliable results. Selection criteria, number of participants, duration of the intervention, lack of follow-up and other problems limit the robustness of evidences from these studies [4, 18, 19]. Moreover, the heterogeneity of the sample did not allow to objectively measure the outcomes. For these reasons, more research needs to be carried out, in order to better assess the methodology in this field. The present umbrella review aimed at:
A) providing an overview of systematic and narrative reviews focusing on MBSR, MBIs interventions in HCPs and healthcare students;
B) giving a summary and indicating implications for future research regarding mindfulness trainings and their impact on HCPs’ health and wellness.
2Materials and Methods
The umbrella review was performed during February 2020 following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement [20]. The study was based on a previously established protocol reviewed by a research team with expertise in knowledge synthesis and overview reviews. The study was not registered with PROSPERO or similar registers.
2.1Identification of relevant studies
Systematic and narrative reviews that examined the impact of MBSR and other MBIs on HCPs and healthcare students’ stress were identified through a systematic search of three electronic databases: PubMed, Scopus and Web of Science. All studies regardless time of publication were considered for inclusion. Moreover, we considered papers published in English, French and Italian. Eligible studies were selected by two researchers through a multi-step approach including title and abstract screening and full-text evaluation. The following search algorithm was used in both databases: “mindfulness AND (healthcare professionals OR nurse* OR doctor*) AND stress reduction AND review”.
2.2Study selection and eligibility criteria
The first selection was performed by filtering duplicated articles. Afterward, title and abstract screening was performed. Then full text assessment was performed. Systematic and narrative reviews were selected according to inclusion and exclusion criteria (Table 1) following the PICOS (Population, Intervention, Comparison, Outcomes and Study Design) search strategy tool.
Table 1
PICOS criteria for inclusion and exclusion of studies
| Include | Exclude | |
| Population | HCPs, healthcare students | Patients, general population |
| Interventions | MBSR, MBIs | None |
| Comparators | Any | None |
| Outcomes | Well-being, perceived stress, anxiety, burnout, performance | None |
| Context/settings | Healthcare environment | Other environments |
| Timing | Pre-post intervention, before-after study | None |
| Study types and designs | Systematic reviews, narrative reviews | Other study designs |
2.3Indicators of effectiveness
The effectiveness of the intervention was based on several outcome measures. The primary outcomes were the healthcare provider’s and student’s well-being and perceived stress, the secondary outcomes varied including mood, anxiety, burnout and performance.
2.4Data extraction and quality assessment
Data were extracted and qualitatively assessed using the AMSTAR 1 tool for systematic reviews and the INSA tool for narrative reviews [21, 22]. AMSTAR consists of 11 items and has good face and content validity for measuring the methodological quality of systematic reviews. The INSA tool consists of 7 criteria and includes a point system according to which each valid answer corresponds to one point. A review awarded a total of 5 points will be considered good. The following study characteristics were extracted:
– author name;
– publication year;
– study design of included studies in the article;
– type of intervention;
– number of studies included in the review;
– primary and secondary outcome;
– participants;
– follow-up (where applicable);
– results.
2.5Data synthesis
In order to organize the amount of data, results have been grouped on the basis of the type of intervention. Three main subcategories were finally identified: MBSR, MBIs, other techniques.
3Results
The search strategy initially resulted in a total of 54 references, of which 31 remained after deduplication. Another 10 articles were excluded after title and abstract screening. 21 full-text articles were then selected and read. Six papers were removed from the final review, since they were not reviews. Finally, 15 studies were included in the umbrella review, of which eleven were systematic reviews and four were narrative reviews (Fig. 1). Most reviews were conducted in the USA, Canada and Australia. One review was conducted in Ireland, and another in Lebanon. The characteristics of reviews are shown in Table 2.
Fig. 1
The PRISMA flowchart and the study selection process.
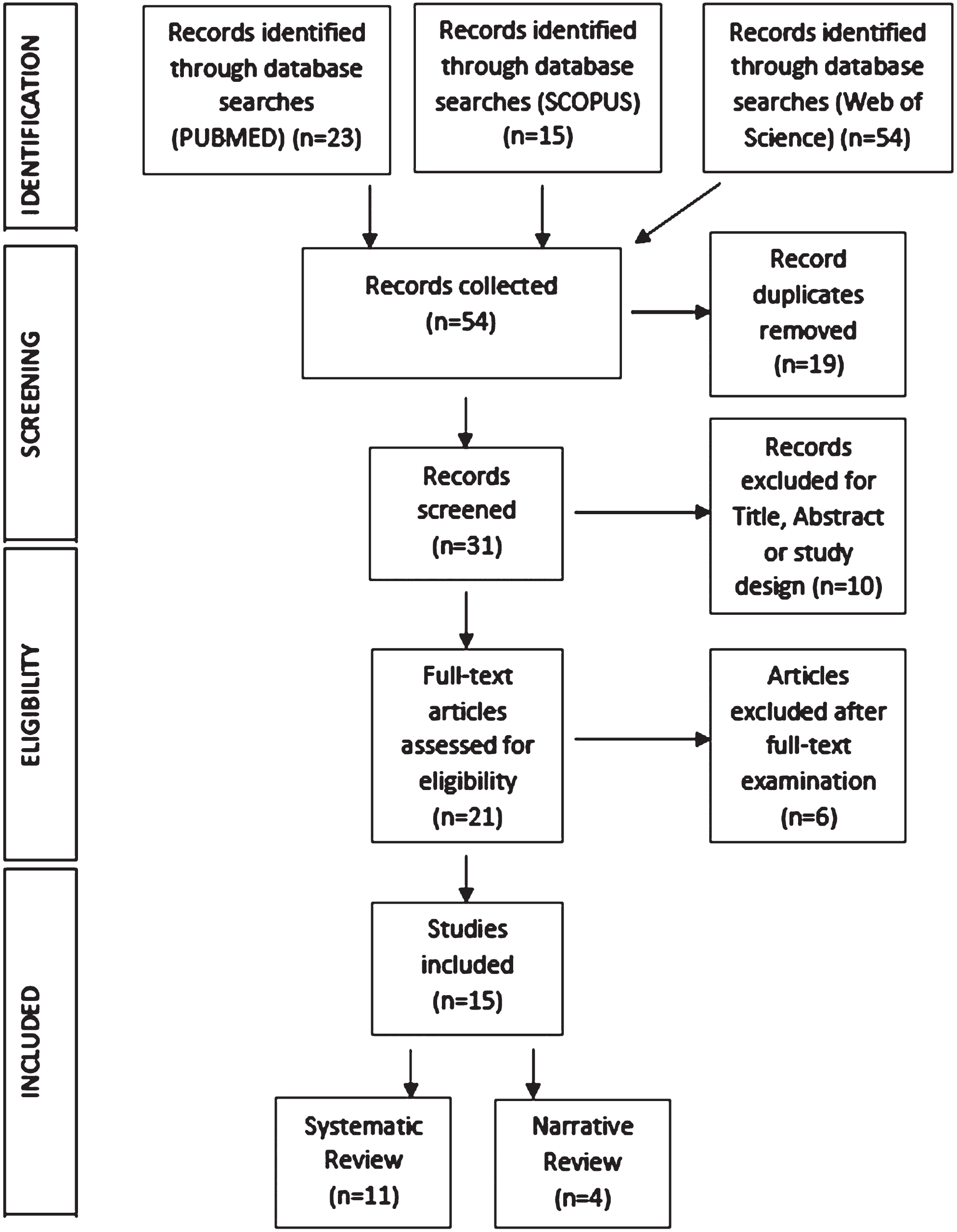
Table 2
Characteristics of the reviews included in the umbrella review
| First Author, Year | Review type | Study design of included studies in the Review | Type of intervention | Studies included in the Review | Primary outcome | Secondary outcome | Participants | Follow-up | Effectiveness | AMSTAR/INSA score |
| Lamothe, 2015 | Systematic review | RCT, quasi-experimental, pre-post (no control) | Not speciffied | 39 | Mental health, physical health and physical well-being, Mindfulness | Sense of coherence | Healthcare students, HCPs | Not specified | MBSR is associated with favorable effects on HCPs’ mental health and levels of mindfulness. Nonetheless, no clear conclusion can be drawn, due to the lackness of an item-level analysis and the weight of specific items on scores and subscores. | 8 |
| Gilmartin, 2017 [24] | Systematic review | Any study design | MBSR, other MBIs Brief MBIs | 14 | Perceived stress, anxiety, depression | Burnout, resiliency | In hospital employed physicians, nurses, nursing students, medical trainees | Not specified | MBIs are mainly associated with improvement of stress and anxiety. Notably, interventions which were adapted to increase accessibility by providers, showed positive results in self-management of reactions to stressful work environments. However not all interventions improved study outcomes. | 7 |
| Everson, 2018 [25] | Systematic review | Not specified | Empathy and communication skills training, patient experience focused programs, film based training and mindfulness training | 15 | Empathic concern | None | Healthcare students, HCPs | Not specified | Some evidence for the effectiveness of MBSR, programs that incorporate the film Wit, and provision of empathy content over the full course of a healthcare degree has been seen. However, a clear impact on EC could not be identified. | 6 |
| Stillwell, 2017 [22] | Systematic review | Quasi-experimental, RCTs, quantitative studies | Stress management course, MBSR techniques | 8 | Perceived stress | None | Healthcare graduate students within USA | Not specified | In all studies, self-care interventions reduced perceived stress in graduate health science students. All studies had small sizes and were conducted in single-cite university settings, having the potential of bias. | 3 |
| Burton, 2017 [26] | Systematic review | RCTs | MBSR-M, other MBIs | 9 | Perceived stress | None | HCPs | Not specified | MBIs are able to significantly decrease stress levels for HCPs. The results of the meta-analysis revealed a significant value of r = 0.342 (CI = 0.202–0.468), showing a medium effect | 7 |
| Ghawadra, 2019 [27] | Systematic review | RCTs, Quasi-experimental | MBSR | 9 | Perceived stress, anxiety, depression | Burnout, life satisfaction | Nurses | Six weeks –four months | MBSR has a positive impact on the psychological well-being of nurses. The mindfulness interventions had effects on improvements of the primary outcomes, such as stress level, reduced in six studies, and anxiety and depression levels, reduced in three studies | 6 |
| Lomas, 2018 [28] | Systematic review | RCTs | MBIs | 81 | Burnout, distress, anxiety, depression, and stress. | None | HCPs | Not specified | Mindfulness based interventions are associated with positive outcomes in relation to the chosen measures, and especially for burnout | 7 |
| O’Driscoll, 2017 [9] | Systematic review | Randomized and non-randomized controlled trial | MBSR techniques | 11 | Stress, mood | Mindfulness levels | Health or social care undergraduate students | 6 months | Benefits have been reported in partecipants’ stress, mood and mindfulness levels, as well as anxiety, well-being, self-compassion and coping abilities. No significant relationship between the number of class hours and effect on psychological distress was reported. Follow-up made in two studies showed no sustained effect. Gender and personality have emerged as factors which potentially affect the results achieved through MBIs. | 4 |
| van der Riet, 2018 [26] | Systematic review | Quantitative, qualitative and mixed | Mindfulness meditation | 16 | Stress reduction, depression, anxiety and burnout | Well-being and empathy | Nursing students, nurses | Engagement in MM programs, especially when accompanied by regular practice, has a significant impact on stress, depression, anxiety, burnout, and well-being. MM has proven to be a protective strategy that builds emotional regulation. | 5 | |
| Smith, 2014 [12] | Systematic review | Randomized and non-randomized control trials, pre-post test, phenomenology and descriptive | MBSR courses | 13 | Stress | Burnout, anxiety, focus, self-improvement, empathy | Students, nurses | Not specified | MBSR has been found to decrease nurses’ stress and increase nurses’ ability to focus, increase attention, and decrease distractive, ruminative thoughts and behaviors. | 2 |
| Spinelli, 2019 | Systematic review | RCT, quasi-experimental, pre-post (no control) | MBSR, MBSR-M, other MBIs | 38 | Anxiety, burnout, depression, psychological distress, stress | Well-being, psychical health, performance, cognitive, clinical, mindfulness | HCPs, HCPs-IT | Not specified | Larger intervention effetcs were found with HCPs, MBSR intervention, and inactive controls. MBSR had the lagest effect on stress, MBIs-O on burnout and MBSR-M on anxiety, depression, and psychological distress. Well-being outcomes were most effected by meditation. | 8 |
| Romani, 2014 [5] | Narrative review | Not specified | Stress management courses, Balint sessions, streching exercise | 15 | Burnout, stress | Performance, well-being, others | Medical students, physicians | Not specified | Multidisciplinar actions such as changes in the work environmental factors and stress management programs that help people to cope better with stressful events, showed promising solutions to manage burnout. Yet, no rigorous studies could prove this. | 2 |
| Raab, 2014 [3] | Narrative review | Not specified | Mindfulness, MBSR | Not specified | Not specified | Not specified | HCPs | Not specified | Mindfulness interventions have potential to reduce stress and burnout and increase empathy and self-compassion, as well as clinical care outcomes, although more research in this field in required. | 1 |
| Irving, 2009 [23] | Narrative review | RCT, NRCT, pre-post, qualitative | MBSR, mindfulness meditation | 10 | Psychological symptoms, empathy, burnout, relaxation | Not specified | Nursing and medical students, HCPs | Not specified | Despite the promising findings for both clinical and non-clinical populations, research on mindfulness has been limited by several issues. Research initiatives with a combined focus upon process and outcome variables and diversified research methos are recommended. | 7 |
| West, 2018 [6] | Narrative review | Not specified | Not specified | Not specified | Burnout, stress | Not specified | Physicians | Not specified | Many gaps regarding burnout knowledge remain. Effective remedies should be taken from all stakeholders in healthcare delivery. | 5 |
3.1Quality of included reviews
Findings of the quality assessment are presented in Tables 3 and 4. None of the systematic reviews reached the maximum of the AMSTAR score. Moreover, all studies failed to satisfy AMSTAR items 4, 5, 11. In particular, the authors did not state whether they searched for reports regardless of their publication type (e.g., grey literature) (AMSTAR item 4), did not provide a list of included and excluded studies (AMSTAR item 5) and did not acknowledge any potential sources of support or cp (AMSTAR item 11).
Table 3
Quality assessment of included systematic reviews according to AMSTAR
| Author, year | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Final rating |
| Lamothe, 2015 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Gilmartin, 2017 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
| Everson, 2018 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 6 |
| Stillwell, 2017 | 0 | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 3 |
| O’Driscoll, 2017 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 4 |
| van der Riet, 2018 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 5 |
| Smith, 2014 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 2 |
| Spinelli, 2019 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 8 |
| Burton, 2017 | 1 | 1 | 1 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 7 |
| Ghawadra, 2019 | 0 | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 6 |
| Lomas, 2018 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 |
Table 4
Quality assessment of included narrative reviews according to INSA
| Author, year | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Final rating |
| Romani, 2014 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| Raab, 2014 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Irving, 2009 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 7 |
| West, 2018 | 1 | 0 | 0 | 1 | 1 | 1 | 1 | 5 |
The final assessment of the systematic reviews varied from critically low to moderate. Among narrative reviews, the study carried out by Irving and colleagues reached all seven items of the INSA score, the study conducted by West five, the remaining two reached very low scores, hence being judged as very low-quality studies.
3.2Mindfulness-based stress reduction
Most of the reviews examined studies that evaluated the effect of MBSR techniques on HCPs and healthcare students. The MBSR program developed by Kabat-Zinn was mainly conducted, consisting in 8 weekly 2.5-h sessions and one full-day silent retreat between the 6th and 7th class [11]. There was a general agreement regarding the results, since they found out that MBSR has an effective role in reducing stress in a targeted sample. However, the overall high heterogeneity of the participants, between and within the reviews, represents a first obstacle to properly evaluate the results. Perceived stress and burnout were the most frequently evaluated outcomes, and their assessment was performed by using the Perceived Stress Scale (PSS) [23] and the Maslach Burnout Inventory (MBI) [24]. Lamothe et al. primarily evaluated perceived stress, finding that MBSR is able to decrease it, and similarly, positive findings regarding burnout, anxiety and mental well-being resulted from the analysis of the studies. Mindfulness outcomes were also evaluated through different questionnaires, showing similar results. Some variants of MBSR were also developed, since a need for adaptation was required in many cases, with shorter and more intensive MBSR courses [19]. Spinelli et al. used the Hedge’s to quantify the effect of various MBSR techniques on the measured outcomes, finding a significant moderate association for several parameters: anxiety, depression, psychological distress and perceived stress. They also analysed some studies that considered a follow-up ranged from 4 to 80 weeks after the intervention, finding small to moderate effect on stress [4]. Smith et al. evaluated different types of MBSR courses mainly for healthcare students and nurses, and measured different outcomes, again reporting positive effects on them [12]. Stillwell et al. focused on pre-post studies, specifically investigating the immediate effect of MBSR techniques and other stress management courses, and demonstrating a reduction in perceived stress after the intervention in all the analysed studies [25].
Burton et al. [26] performed a meta-analysis on 7 out of 9 papers included in their systematic review and found that MBSR, MBSR-M and MBIs are interventions that have a significant impact on decreasing stress levels for HCPs. The results of the meta-analysis shows a medium effect (r = 0.342; CI = 0.202–0.468).
Gilmartin et al. [16] performed a systematic review using the results of 14 papers, of which 50% were RCTs. 83% of the studies reported statistically significant improvements in stress score levels after completion of the intervention. Moreover, two thirds of the studies reveal positive changes in levels of anxiety, resiliency, and burnout symptoms.
A systematic review, performed by Ghawadra et al. [27] on papers on the effect of MBSR intervention on nurses, found the MBSR has a positive impact on the psychological well-being of these HCPs. These interventions are able to improve the primary outcomes, such as stress level, reduced in 66% of studies, and anxiety and depression levels, reduced in 33% of the studies.
O’Driscoll et al., in their review, accounted studies performing follow-up monitoring, but interestingly a lack of sustained effect was reported, suggesting that a continuous MBSR course should be followed to maintain the positive effects on stress reduction [9]. The two narrative reviews that analysed this type of intervention, published by Raab and Irving et al., also agreed that MBSR could represent a promising tool for HCPs and healthcare students to manage stress, burnout, and other mental and physical affections [3, 25]. In particular, Raab focused on the concept of self-compassion as an attitude enhanced by MBSR training, which eventually leads to a reduction in maladaptive cognitive coping tendencies and a better management of stress. Nonetheless, all these studies underlined difficulties in properly interpreting data. Apart from the consistent heterogeneity reported in many studies, a limited number of participants and contrasting results made it difficult to perform a sensitive analysis. Moreover, most reviews reported a high-risk bias in the primary studies.
3.3Mindfulness-based interventions
Apart from the main MBSR intervention other mindfulness-based interventions were evaluated to analyze the effect on stress in the targeted population. Van der Riet et al. mainly focused on nurses and nursing students and considered various mindfulness meditation (MM) techniques to reduce stress. The results of this review identified that MM can have positive impact on stress, anxiety, depression and burnout among nurses and nursing students [17]. However, the authors also put forward that the majority of papers included in the review described small scale localized studies which limit the generalizability of the results [17]. Spinelli et al. considered some other MBIs among the studies. It was reported that while MBSR intervention had the largest effect on stress, other MBIs were more effective on burnout [4, 28]. Gilmartin et al. included studies that incorporated different MBIs, some focusing only on mindfulness, others including mindfulness within multifaceted resiliency programs to reduce medication errors, others used a combination of lecture, discussion, and group or independent practice sessions. The dose, duration, and settings of the different interventions also varied. Outcomes regarding the providers’ mental and physical health were measured through different scores, and most of the studies reported statistically significant improvements; no significant improvement on medical errors reduction was reported [16]. Moreover, Raab et al. also considered other MBIs along with MBSR courses as instruments for HCPs to face stress, burnout, depression. They also underlined the importance of empathy and compassion as fundamental characteristics for working with the suffering of people and argued that both MBSR and other MBIs also contribute to balance these aspects [3].
3.4Other techniques
Different approaches to reduce stress, burnout, and generally to improve HCPs and students’ mental and physical health, as well as to enhance their attitude and competence to work or study, were examined by some other studies. Apart from MBSR and MBIs, other types of courses were evaluated to verify the efficacy that they may have had. In particular, Romani et al. considered studies that analyzed various stress management courses:
– sociopsychological training;
– sessions of open discussions and problem solving within a flexible, group-determined set of agenda items;
– single, all-day stress management workshop;
– meditation and breathing exercises [5].
Some of them resulted in positive effects, others, such as the second, demonstrated no improvement in the measured outcomes. Other included studies by Romani et al. analysed Balint sessions, showing an important improvement in patient-centred care and self-esteem among general practitioners. Similar results were obtained for studies that evaluated some exercises, especially stretching exercises in the workplace. Finally, some occupational interventions were considered to verify the improvement of the practitioner’s well-being, in particular giving priority to physicians’ well-being as much as the quality of care, or identifying factors that produce stress, and trying to reduce them. Everson et al. focused mainly on programs that promote health professional students’ empathic concern [29]. The interventions were divided into four categories: empathy and communication skills training, patient experience focused programs, film-based training and mindfulness training. Again, contrasting results did not allow the studies to provide a statistically significant conclusion.
4Discussion
This umbrella review examined eleven systematic and four narrative reviews focusing on MBSR and MBI techniques to reduce stress among HCPs and healthcare students. Hilton et al. [30] already created an evidence map summarizing the impact of mindfulness interventions, also for HCPs. However, they did not perform a systematic review.
4.1Stress
The results suggest that the techniques evaluated can be effective in helping this target population to cope with stress. Due to high demand and workplace stress, HCPs and healthcare students may experience high levels of stress, and mindfulness-based interventions were generally found to reduce symptoms and to improve mental health outcomes [14, 25–27]. Other MBIs and stress management interventions also led to a better mental health state in participants [15, 16]. The most overall evaluated outcome was perceived stress,that was most often measures using the PSS. In most studies perceived stress decreased after the intervention. Comparison among interventions showed different outcomes, with MBSR having the largest effect on stress reduction.
4.2Burnout
Burnout was also frequently measured, mainly using Maslach Burnout Inventory, which reported positive results. Van der Riet et al demonstrated that mindfulness meditation has proven to be a protective strategy that builds emotional regulation, and this can have a preventive impact on burnout development [17].
4.3Anxiety, depression and well-being
Beyond these two major aspects (stress and burnout), various measurements of well-being, physical health, performance, empathy, or even patients’ satisfaction were performed, showing less positive results.
As far as concerns anxiety and depression, O’Driscoll et al. [9] and Raab et al. [3] underline the potential benefit of MBSR through the mediation of compassion and self-compassion. These effects are of particular interest for the HCPs, for improving work relationships (i.e., job satisfaction) and increasing perceived comfort with patients.
van der Riet et al. [17] and Spinelli [3] demonstrated that engagement in Mindfulness Meditation programs, especially when accompanied by regular practice, appeared to be most effective in increasing well-being.
4.4Limitations
Several limitations must be acknowledged in this review. First of all, most studies included in the single reviews had small sample sizes, and a grade of heterogeneity varying from moderate to high for different outcomes, having the potential for bias [15, 25]. In many studies there a control group was lacking, making it difficult to provide evident outcomes. Furthermore, the intervention settings often varied within the studies, mainly due to the difficulty for participants to attend the courses at the same time of the day due to different work-shifts. Consequently, it was difficult to recommend a standardized MBSR or MBIs approach to better evaluate the outcome [4]. Besides, almost all studies did not include follow-up observations, making it difficult to establish the long-term effect of the interventions [14]. Furthermore, the studies that used a follow-up, showed no sustained effects, suggesting that MBSR courses should be continuatively implemented in order to maintain the benefits over time [9].
Another limitation was the choice of some studies to include together different types of HCPs and students, not considering the difference that can be present among them, especially for students, which were certainly exposed to different factors compared to HCPs. For all these reasons, the quality of the studies was generally affected, and this review could not fully clarify the effectiveness of the analyzed methods in reducing stress in HCPs and healthcare students.
5Conclusions
Stress has been identified as a risk factor for health among both HCPs and healthcare students. The high prevalence of workplace stress as well as the complex and demanding nature of healthcare underline the need for implementing strategies to increase resilience. The present review summarized studies that focused on the efficacy and effectiveness of MBSR and MBI techniques to reduce stress.
However, we need to recognize that while both MBSR and other MBIs techniques can be effective in reducing stress, the review also identified limitations and consequently roadways for further research. There is sufficient evidence to use these techniques in longitudinal education training of both HCPs and healthcare students.
From the methodological point of view, future research should focus on the standardization of the intervention, sufficient sample sizes to empower hypothesis testing, a separate analysis of HCPs and students, conduction of follow-up investigations to assess the continuation of the intervention efficacy and application of better instruments of analysis, such as developing more focused questionnaires for HCPs.
Funding
This research received no external funding.
Acknowledgments
The authors thank Dr. Insa Backhaus for the linguistic revision of the paper
Conflict of interest
The authors declare no conflict of interest.
References
[1] | Cocchiara RA , Peruzzo M , Mannocci A , Ottolenghi L , Villari P , Polimeni A , Guerra F , La Torre G . The Use of Yoga to Manage Stress and Burnout in Healthcare Workers: A Systematic Review, J Clin Med (2019) ;8: :284. |
[2] | Silva-Junior JS . Preventing occupational stress in healthcare workers, Sao Paulo Med J (2016) ;134: (1):92. |
[3] | Raab K . Mindfulness, Self-Compassion, and Empathy Among Health Care Professionals: A Review of the Literature, J Health Care Chaplain (2014) ;20: (3):95–108. |
[4] | Spinelli C , Wisener M , Khoury B . Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials, J Psychosom Res (2019) ;120: :29–38. |
[5] | Romani M , Ashkar K . Burnout among physicians, Libyan J Med (2014) ;9: :1. |
[6] | West CP , Dyrbye LN , Shanafelt TD . Physician burnout: contributors, consequences and solutions, J Intern Med (2018) ;283: (6):516–29. |
[7] | Panagioti M , Panagopoulou E , Bower P , Lewith G , Kontopantelis E , Chew-Graham C , Dawson S , van Marwijk H , Geraghty K , Esmail A . Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis, JAMA Intern Med (2017) ;177: (2):195–205. |
[8] | Stecker T . Well-being in an academic environment, Med Educ (2004) ;38: (5):465–78. |
[9] | O’ Driscoll M , Byrne S , Mc Gillicuddy A , Lambert S , Sahm LJ . The effects of mindfulness-based interventions for health and social care undergraduate students –a systematic review of the literature. Psychol Health Med. (2017) ;8506: :1–15. |
[10] | Praissman S . Mindfulness-based stress reduction: A literature review and clinician’s guide, J Am Acad Nurse Pract (2008) ;20: (4):212–6. |
[11] | Kabat-Zinn J . An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results, Gen Hosp Psychiatry (1982) ;4: (1):33–47. |
[12] | Smith SA . Mindfulness-Based Stress Reduction: An Intervention to Enhance the Effectiveness of Nurses’ Coping With Work-Related Stress, Int J Nurs Knowl (2014) ;25: (2):119. |
[13] | Salmon P , Sephton S , Weissbecker I , Hoover K , Ulmer C , Studts JL . Mindfulness meditation in clinical practice, Cogn Behav Pract (2004) ;11: (4):434–46. |
[14] | Manotas M , Segura C , Eraso M , Oggins J , McGovern K . Association of brief mindfulness training with reductions in perceived stress and distress in Colombian health care professionals, Int J Stress Manag (2014) ;21: (2):207–25. |
[15] | Irving JA , Dobkin PL , Park J . Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR), Complement Ther Clin Pract (2009) ;15: (2):61–6. |
[16] | Gilmartin H , Goyal A , Hamati MC , Mann J , Saint S , Chopra V . Brief Mindfulness Practices for Healthcare Providers –A Systematic Literature Review, Am J Med (2017) ;130: (10):e1–1219.e17. |
[17] | van der Riet P , Levett-Jones T , Aquino-Russell C . The effectiveness of mindfulness meditation for nurses and nursing students: An integrated literature review, Nurse Educ Today (2018) ;65: :201–11. |
[18] | Dobkin PL , Hutchinson TA . Teaching mindfulness in medical school: Where are we now and where are we going? Med Educ (2013) ;47: (8):768–79. |
[19] | Lamothe M , Rondeau E , Malboeuf-Hurtubise C , Duval M , Sultan S . Outcomes of MBSR or MBSR-based interventions in health care providers: A systematic review with a focus on empathy and emotional competencies, Complement Ther Med (2016) ;24: :19–28. |
[20] | Liberati A , Altman DG , Tetzlaff J , Mulrow C , Gøtzsche PC , Ioannidis JP , Clarke M , Devereaux PJ , Kleijnen J , Moher D . The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration, Ann Intern Med (2009) ;151: (4):W65–94. |
[21] | Shea BJ , Grimshaw JM , Wells GA , Boers M , Andersson N , Hamel C , Porter AC , Tugwell P , Moher D , Bouter LM . Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews, BMC Med Res Methodol (2007) ;7: :10. |
[22] | La Torre G , Backhaus I , Mannocci A . Rating for narrative reviews: concept and development of the International Narrative Systemic Assessment tool, Senses Sci (2015) ;2: (2):31–5. |
[23] | Cohen S , Kamarck T , Mermelstein R . A global measure of perceived stress, J Health Soc Behav (1983) ;24: (4):385–96. |
[24] | Maslach C , Jackson SE , Leiter MP . The Maslach Burnout Inventory. Evaluating Stress: A Book of Resources, 1997. |
[25] | Stillwell SB , Vermeesch AL , Scott JG . Interventions to Reduce Perceived Stress Among Graduate Students: A Systematic Review With Implications for Evidence-Based Practice, Worldviews Evid Based Nurs (2017) ;14: (6):507–13. |
[26] | Burton A , Burgess C , Dean S , Koutsopoulou GZ , Hugh-Jones S . How Effective are Mindfulness-Based Interventions for Reducing Stress Among Healthcare Professionals? A Systematic Review and Meta-Analysis, Stress Health (2017) ;33: (1):3–13. |
[27] | Ghawadra SF , Abdullah KL , Choo WY , Phang CK . Mindfulness-based stress reduction for psychological distress among nurses: A systematic review, J Clin Nurs (2019) ;28: (21-22):3747–58. |
[28] | Lomas T , Medina JC , Ivtzan I , Rupprecht S , Eiroa-Orosa FJ . A systematic review of the impact of mindfulness on the well-being of healthcare professionals, J Clin Psychol (2018) ;74: (3):319–55. |
[29] | Everson N , Levett-Jones T , Pitt V . The impact of educational interventions on the empathic concern of health professional students: A literature review, Nurse Educ Pract (2018) ;31: :104–11. |
[30] | Hilton LG , Marshall NJ , Motala A , Taylor SL , Miake-Lye IM , Baxi S , Shanman RM , Solloway MR , Beroesand JM , Hempel S . Mindfulness meditation for workplace wellness: An evidence maWork (2019) ;63: (2):205–18. |



