Antibiotics Susceptibility Profile of Gram-Positive Bacteria from Primary Health Centers in Jega, Kebbi State
Abstract
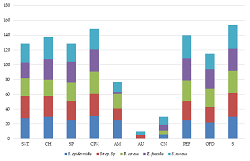
Nosocomial or healthcare-associated infection (HCAI) is an infection acquired during receiving health care that was not present during admission. The research aimed to determine the antibiotic susceptibility pattern of gram-positive bacteria isolated from Primary Health Centers in Jega Town. A total of fifty (50) swab samples were collected from 10 different health centers and analyzed using the streak plate technique. Pure bacterial isolates were maintained and characterized using biochemical tests; their percentage of occurrence show; Staphylococcus aureus 18 (43.9%), Enterococcus feacalis 8 (19.5%), Streptococcus spp 8 (19.5%), Bacillus cereus 4 (9.8%), and Staphylococcus epidermidis 3 (7.3%). McFarland standard solution was prepared and used to control inoculants, after which the antibiotic susceptibility pattern of the isolates was determined using the disc diffusion method. Staphylococcus epidermidis was resistant to Gentamycin, and other isolates were multi-drug resistant. In light of this research, there is a need for thorough disinfection and conscientious contact control procedures to minimize the spread of these pathogens in health centers where interaction between patients, HCWs, and caregivers is widespread and frequent.
Full text article
References
2. Khan HA, Baig FK, Mehboob R. Nosocomial infections: Epidemiology, prevention, control and surveillance. Asian Pac J Trop Biomed. 2017;7(5):478-82. doi:10.1016/j.apjtb.2017.01.019
3. Ssekitoleko RT, Oshabaheebwa S, Munabi IG, Tusabe MS, Namayega C, Ngabirano BA, et al. The role of medical equipment in the spread of nosocomial infections: a cross-sectional study in four tertiary public health facilities in Uganda. BMC Public Health. 2020;20(1):1561. doi:10.1186/s12889-020-09662-w
4. Voidazan S, Albu S, Toth R, Grigorescu B, Rachita A, Moldovan I. Healthcare Associated Infections-A New Pathology in Medical Practice? Int J Environ Res Public Health. 2020;17(3):760. doi:10.3390/ijerph17030760
5. Maki G, Zervos M. Health Care-Acquired Infections in Low- and Middle-Income Countries and the Role of Infection Prevention and Control. Infect Dis Clin North Am. 2021;35(3):827-39. doi:10.1016/j.idc.2021.04.014
6. Rangelova VR, Raycheva RD, Kevorkyan AK, Krasteva MB, Kalchev YI. Ventilator-Associated Pneumonia in Neonates Admitted to a Tertiary Care NICU in Bulgaria. Front Pediatr. 2022;10:909217. doi:10.3389/fped.2022.909217
7. Vincent JL, Sakr Y, Singer M, Martin-Loeches I, Machado FR, Marshall JC, et al. Prevalence and outcomes of infection among patients in intensive care units in 2017. JAMA. 2020;323(15):1478-87. doi:10.1001/jama.2020.2717
8. Ghashghaee A, Behzadifar M, Azari S, Farhadi Z, Bragazzi N, Behzadifar M, et al. Prevalence of Nosocomal Infections in Iran: Asystematic Review and Meta-analysis. Med J Islam Repub Iran. 2018;32:48. doi:10.14196/mjiri.32.48
9. Winters ME, Hu K, Martinez JP, Mallemat H, Brady WJ. The critical care literature 2018. Am J Emerg Med. 2020;38(3):670-80. doi:10.1016/j.ajem.2019.11.032
10. Li S, Xu Y, Cai J, Hu D, He Q. Integrated environment-occupant-pathogen information modeling to assess and communicate room-level outbreak risks of infectious diseases. Build Environ. 2021;187:107394. doi:10.1016/j.buildenv.2020.107394
11. Yen MY, Schwartz J, King CC, Lee CM, Hsueh PR, Society of Taiwan Long-term Care Infection Prevention and Control. Recommendations for protecting against and mitigating the COVID-19 pandemic in long-term care facilities. J Microbiol Immunol Infect. 2020;53(3):447-53. doi:10.1016/j.jmii.2020.04.003
12. Ikeh EI, Isamade ES. Bacterial flora of fomites in a Nigerian multi-disciplinary intensive care unit. Lab Med. 2011;42(7):411-3. doi:10.1309/LMTVPU3PMWAWL0IG
13. Neely AN, Maley MP. Survival of enterococci and staphylococci on hospital fabrics and plastic. J Clin Microbiol. 2000;38(2):724-6. doi:10.1128/jcm.38.2.724-726.2000
14. Maryam A, Hadiza US, Aminu UM. Characterization and determination of antibiotics susceptibility pattern of bacteria from some fomites in a teaching hospital in northern Nigeria. Afr J Microbiol Res. 2014;8(8):814-8. doi:10.5897/AJMR2013.6512
15. Inweregbu K, Dave J, Pittard A. Nosocomial infections. Contin Educ Anaesth Crit Care Pain. 2005;5(1):4-17. doi:10.1093/bjaceaccp/mki006
16. Gopinathan U, Sharma S, Garg P, Rao GN. Review of Epidemiological Feature, Microbiological Diagnosis and Treatment Outcome of Microbial Keratitis: experience of over a decade. Indian J Ophthalmol. 2009;57(4):273-9. doi:10.4103/0301-4738.53051
17. Olise CC, Simon-Oke IA. Formites: Possible Vehicle of Nosocomial Infections. J Public Health Nutr. 2018;1(1):16. doi:10.35841/public-health-nutrition.1.1.11-16
18. Sathish KSR, Kokati VBR. In-vitro antimicrobial activity of marine actinobacteria against multidrug resistance Staphylococcus aureus. Asian Pac J Trop Biomed. 2012;2(10):787-92. doi:10.1016/s2221-1691(12)60230-5
19. Bhutia MO, Thapa N, Tamang JP. Molecular Characterization of Bacteria, Detection of Enterotoxin Genes, and Screening of Antibiotic Susceptibility Patterns in Traditionally Processed Meat Products of Sikkim, India. Front Microbiol. 2021;11:599606. doi:10.3389/fmicb.2020.599606
20. Balouiri M, Sadiki M, Ibnsouda SK. Methods for in vitro evaluating antimicrobial activity: A review. J Pharm Anal. 2016;6(2):71-9. doi:10.1016/j.jpha.2015.11.005
21. Alphons KS, Fortune TV, Haindongo E, Guillaume AY. Bacterial contamination and antimicrobial susceptibility from the hands of health care workers (HCWs) and inanimate surfaces in the neonatal intensive care unit (NICU) at the Windhoek Central Hospital (WCH). Microbiol Nat. 2020;1(3):83-95. doi:10.26167/x34y-rn94
22. Kim MW, Greenfield BK, Snyder RE, Steinmaus CM, Riley LW. The association between community-associated Staphylococcus aureus colonization and disease: a meta-analysis. BMC Infect Dis. 2018;18(1):86. doi:10.1186/s12879-018-2990-3
23. Munoz-Price LS, Arheart KL, Mills JP. Associations between bacterial contamination of health care workers' hands and contamination of white coats and scrubs. Am J Infect Control. 2012;40(9):e245-8. doi:10.1016/j.ajic.2012.03.032
24. Chikere CB, Omoni VT, Chikere BO. Distribution of potential nosocomial pathogens in a hospital environment. Afr J Biotechnol. 2008;7(20):3535-8.
25. Yahav D, Eliakim-Raz N, Leibovici L, Paul M. Bloodstream infections in older patients. Virulence. 2016;7(3):341-52. doi:10.1080/21505594.2015.1132142
26. Vasudevan R, Shin JH, Chopyk J, Peacock WF, Torriani FJ, Maisel AS, et al. Aseptic barriers allow a clean contact for contaminated stethoscope diaphragms. Mayo Clin Proc Innov Qual Outcomes. 2020;4(1):21-30. doi:10.1016/j.mayocpiqo.2019.10.010
27. Koscova J, Hurnikova Z, Pistl J. Degree of bacterial contamination of mobile phone and computer keyboard surfaces and efficacy of disinfection with chlorhexidine digluconate and triclosan to its reduction. Int J Environ Res Public Health. 2018;15(10):2238. doi:10.3390/ijerph15102238
28. Lee AS, de Lencastre H, Garau J, Kluytmans J, Malhotra-Kumar S, Peschel A, et al. Methicillin-resistant Staphylococcus aureus. Nat Rev Dis Primers. 2018;4:18033. doi:10.1038/nrdp.2018.33
29. Treakle AM, Thom KA, Furuno JP, Strauss SM, Harris AD, Perencevich EN. Bacterial contamination of health care workers' white coats. Am J Infect Control. 2009;37(2):101-5. doi:10.1016/j.ajic.2008.03.009
30. Sani RA, Garba SA, Oyewole OA, Ibrahim A. Antibiotic resistance profile of gram positive bacteria isolated from wound infections in Minna, Bida, Kontagora and Suleja area of Niger State. J Health Sci. 2012;2(3):19-22. doi:10.5923/j.health.20120203.01
31. Ogunshe AA, Niemogha MT, Azum GN, Odikagbue AN. Microbiological evaluation of antibiotic resistance in bacterial flora from skin wounds. J Pharm Biomed Sci. 2012;22(6):1-7.
32. Lee NY, Song JH, Kim S, Peck KR, Ahn KM, Lee SI. Carriage of antibiotic-resistant pneumococci among Asian children: A multinational surveillance by the Asian Network for Surveillance of Resistant Pathogens (ANSORP). Clin Infect Dis. 2001;32(10):1463-9. doi:10.1086/320165
Authors
Authors continue to retain the copyright to the article if the article is published in the Borneo Journal of Pharmacy. They will also retain the publishing rights to the article without any restrictions.
Authors who publish with this journal agree to the following terms:
- Any article on the copyright is retained by the author(s).
- The author grants the journal, right of first publication with the work simultaneously licensed under a Creative Commons Attribution License that allows others to share work with an acknowledgment of the work authors and initial publications in this journal.
- Authors are able to enter into separate, additional contractual arrangements for the non-exclusive distribution of published articles of work (eg, post-institutional repository) or publish it in a book, with acknowledgment of its initial publication in this journal.
- Authors are permitted and encouraged to post their work online (e.g., in institutional repositories or on their websites) prior to and during the submission process, as can lead to productive exchanges, as well as earlier and greater citation of published work.
- The article and any associated published material are distributed under the Creative Commons Attribution-ShareAlike 4.0 International License.