- Norwich Medical School, University of East Anglia, Norwich, United Kingdom
Aims: We conducted a meta-analysis of serious adverse events (dementia, macro- and micro-vascular events, falls and fractures, and death) associated with hypoglycemia in older patients treated with glucose lowering drugs.
Materials and Methods: Meta-analysis of studies reporting on hypoglycemia and adverse events. The search included studies from two previously published systematic reviews, and an updated search of MEDLINE and EMBASE from April 2014 to November 2019. We assessed study validity based on ascertainment of hypoglycemia, adverse events and adjustment for confounders, and conducted a random effects meta-analyses, assessing heterogeneity using the I2 statistic.
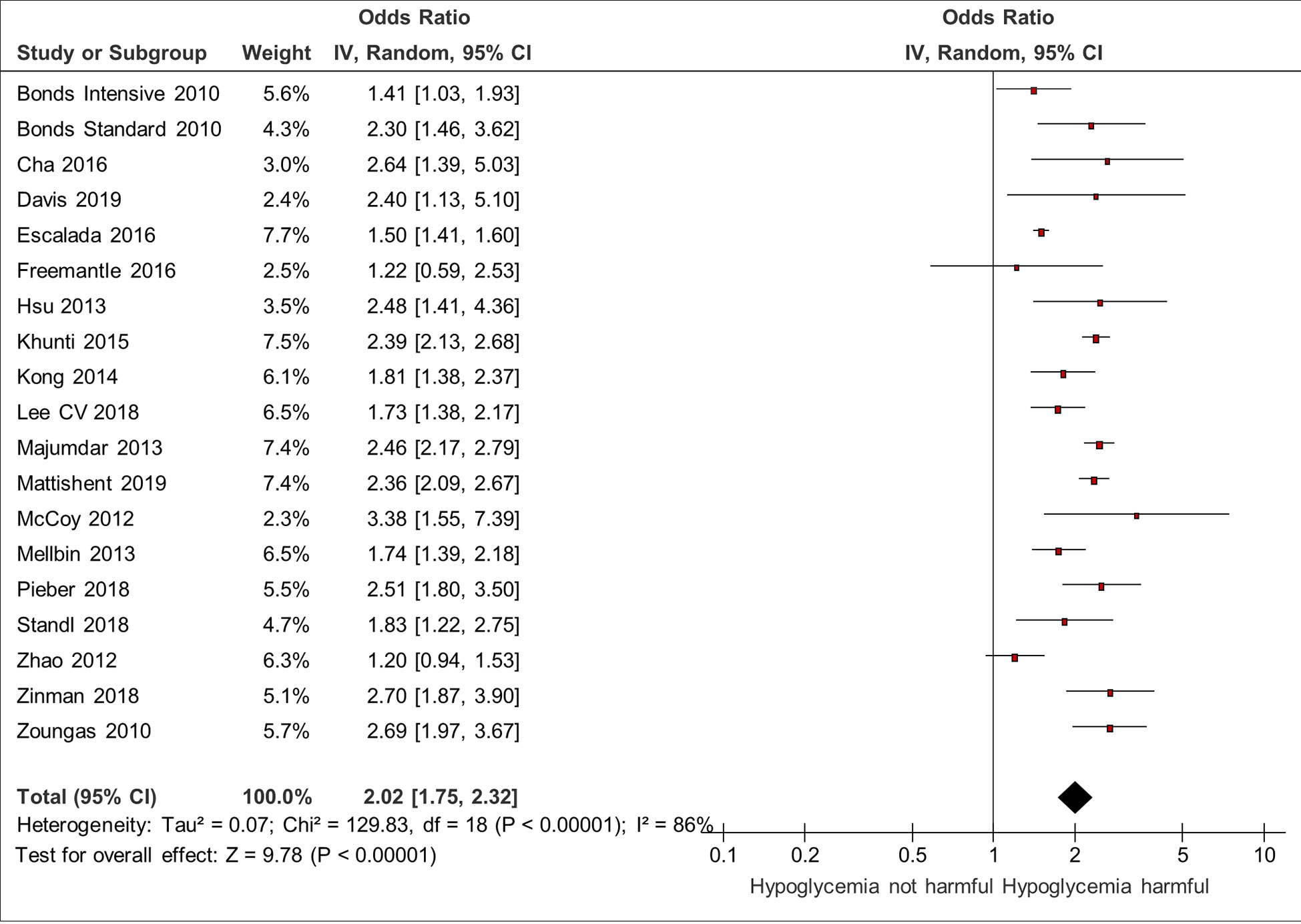
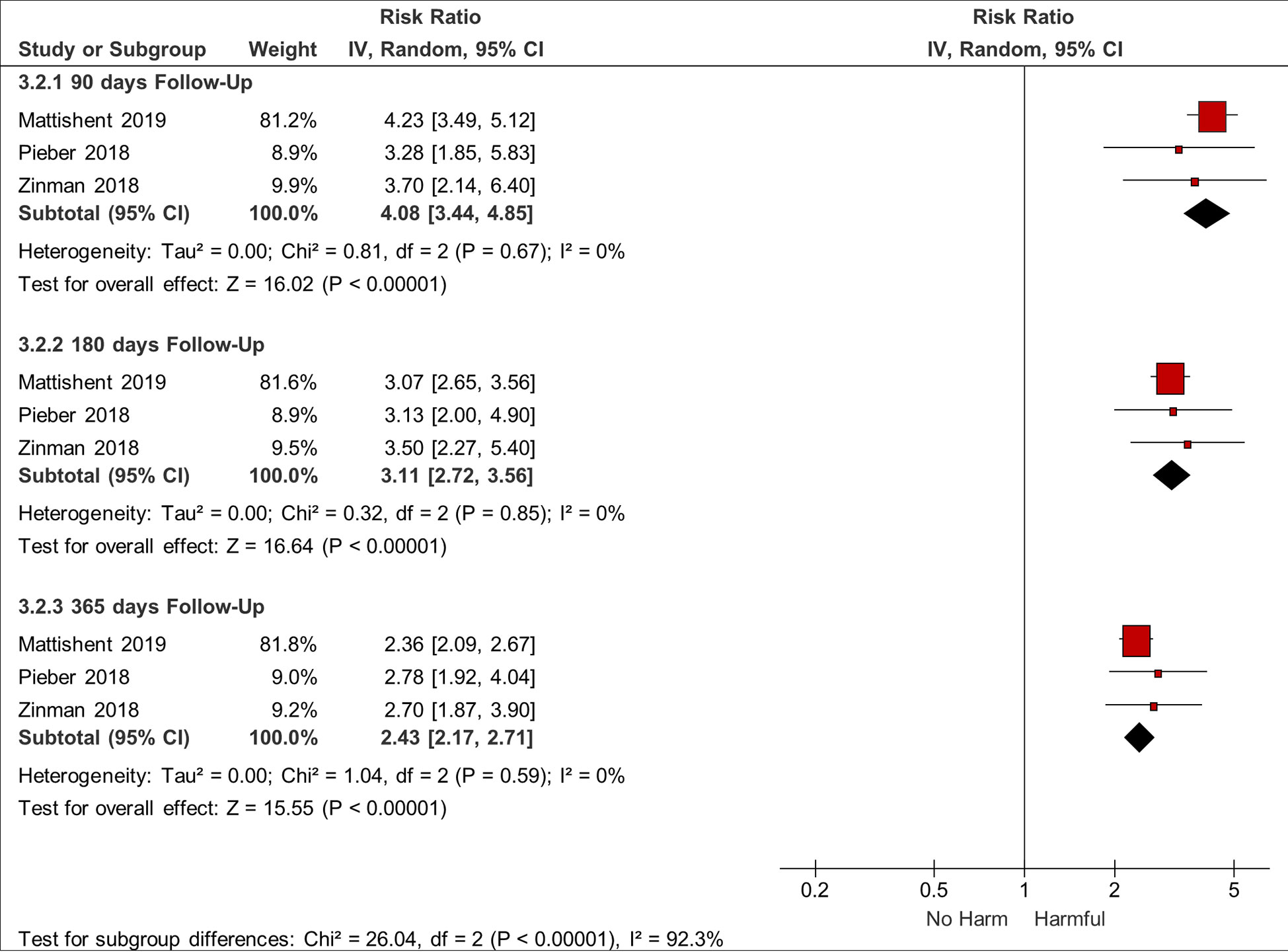
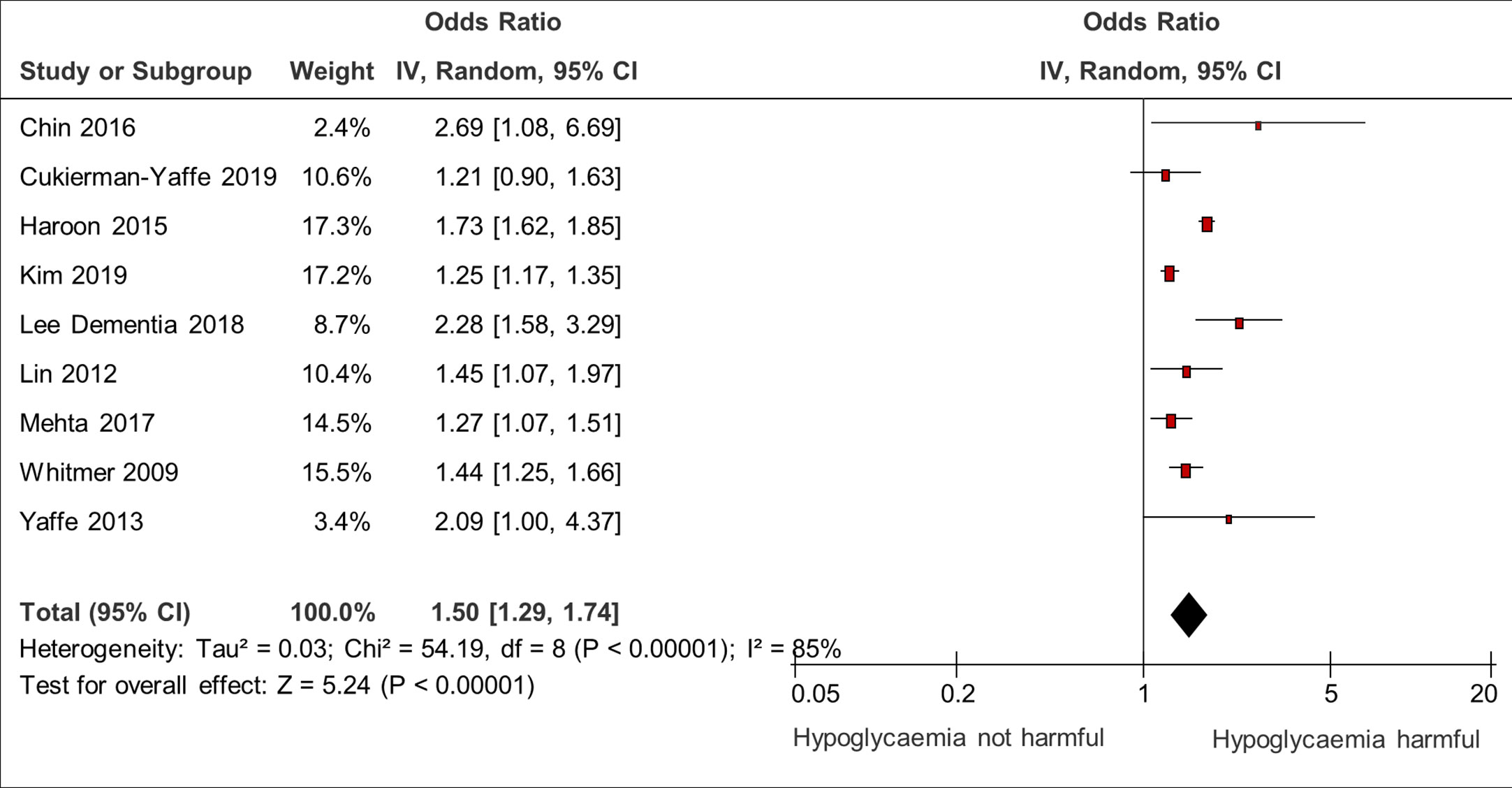
Results: We included 44 studies involving 2,507,434 participants. Most of the studies used adjusted analysis for confounders and hypoglycaemic events were typically identified based on healthcare databases (severe events). Hypoglycemia was associated with increased likelihood of death in a meta-analysis of eighteen studies, pooled OR 2.02 (95% Confidence Interval 1.75–2.32). Studies assessing mortality signal a time-response relationship with a higher risk of adverse events occurring within the first 90 days after hypoglycemia. Our meta-analysis of nine studies demonstrated that hypoglycaemic episodes were associated with dementia – pooled OR 1.50 (95% CI 1.29–1.74). Our meta-analysis of nineteen studies demonstrated associations between hypoglycaemia and macrovascular complications, pooled OR 1.81 (95% CI 1.70–1.94), and microvascular complications (two studies) pooled OR 1.77 (95% CI 1.49–2.10). There is also an association between hypoglycemia and cardiovascular death (six studies) – pooled OR 2.11 (95% CI 1.55 to 2.87). Similarly, our meta-analysis of six studies demonstrated an association between hypoglycemia and falls and fractures, pooled OR 1.78 (95% CI 1.44–2.21) and 1.68 (95% CI 1.37–2.07) respectively.
Conclusion: This meta-analysis confirms previously reported concerns of serious harm following hypoglycemia, especially in the immediate time period after a hypoglycaemic event. Avoidance of hypoglycaemic episodes should be a priority in this vulnerable population.
Introduction
We have previously published two meta-analyses on adverse events (dementia, macro- and micro-vascular events, falls and fractures, and death associated with hypoglycemia in older people treated with glucose-lowering drugs (1, 2). However, since those publications in 2016, we are aware of many new studies [including the authors’ own work (3)] on adverse events associated with hypoglycemia. Hence, we have updated our meta-analyses and present a comprehensive review of the up to date evidence regarding the association between hypoglycemia and adverse events in older people.
Our first systematic review looked at the bi-directional relationship between hypoglycemia and dementia (2). The key findings of the meta-analyses were a 70% increased risk of deterioration in cognition following hypoglycemia and conversely a 60% increased risk of hypoglycemia in older people with dementia. However, this review did not include other major adverse events that may be associated with hypoglycemia. Hence, our second systematic review which focused on vascular adverse events, falls and fractures and all-cause mortality. We found a 1.5 times increased risk in macrovascular events (ischaemic strokes, myocardial infarctions) and a doubling of risk in falls, fractures, and all-cause mortality, but there was insufficient data on cardiovascular death to enable meta-analysis (1). This second review also did not find any studies that specifically looked at the effects of hypoglycemia in older patients who also have dementia.
This updated search of the most recent evidence allows us to access a far larger data set and perform meta-analyses of additional cardiovascular outcomes and time-relationships that we could not previously address due to insufficient data.
Materials and Methods
We worked from the methods described in previously published meta-analyses (1, 2).
Data Sources and Searches
The population we were interested in was older adults. The intervention was ‘hypoglycemia’ and the comparator ‘no hypoglycemia’. The outcomes of interest were cardiovascular events, falls and fractures, death and dementia.
The searches we ran only included terms for the population and the intervention, as the outcomes are too diverse and non-specific for us to be confident that we would capture all the relevant papers if we focused on particular outcomes. For instance, myocardial infarction could be described under a multitude of terms as acute coronary syndrome, STEMI or NSTEMI.
Three searches fed into this systematic review and meta-analysis.
For both previously published reviews, we searched MEDLINE and EMBASE for a ten-year period up to March 2015 with English language restriction.
Bibliographies of included studies were checked for other potentially suitable studies. We were notified through PubMed automated updates of any new relevant studies.
The search strategy for the current review was conducted up to November 2019 and can be found in Appendix 1.
Study Selection
In our analysis, we included cohort studies (prospective and retrospective), which examined the association between hypoglycemia and serious adverse events in participants aged 55 years and older on glucose-lowering medications. We used an arbitrary cut-off of 55 years because there is no internationally accepted definition, and we aimed to be broad rather than too restrictive. We treated post-hoc analyses of randomized controlled trials as cohort studies, as the analysis is no longer on a prospective randomized basis due to post-hoc classification of patients (with and without hypoglycemia).
We excluded cross-sectional studies, because it would be impossible to determine whether the intervention (hypoglycemia) or outcome (adverse events) occurred first.
We included only full journal publications because abstracts are limited in word count and cannot fully describe the statistical models and confounding variables that are of key interest in non-randomized studies.
Data Extraction and Quality Assessment
Two authors conducted study screening and data extraction independently. Uncertainties and discrepancies were resolved through discussion.
We used a standardized form to collect data on study design, study year, geographical location, setting, selection criteria, participants’ characteristics and outcome measures. We extracted relative measures of effect such as odds ratios, risk ratios, and hazard ratios for the outcomes of interest in the group with hypoglycemia as compared to the controls (please refer to Tables 1 and 2). For the sensitivity analysis of survival at different time-points we have focussed only on studies that report hazard ratios.
The outcomes (adverse events) of interest were dementia, falls and fractures, composite cardiovascular (macrovascular) and microvascular events and all-cause mortality.
We independently assessed study validity by looking at how hypoglycemia and serious adverse events were recorded and whether adjustments were made for potential confounding factors.
Data Synthesis and Analysis
We performed a random effects meta-analysis of the relative effect measures using the generic inverse variance method (Revman 5.3, Nordic Cochrane Centre, Kobenhavn). As adverse events are rare, odds ratios and risk or hazard ratios will yield similar estimates of relative effect, and we have pooled all of them using a random effects model. The random effects method for meta-analyses takes into account heterogeneity and estimates an average effect, considering differences in intervention effects as random, rather than the single true effect pooled estimate that arises from the fixed effect model.
Heterogeneity was assessed by using the I2 statistic and visual inspection of the forest plots.
We planned to construct a funnel plot if we had more than 10 studies in the meta-analysis (without evidence of statistical heterogeneity - I2 <50%).
As this was a systematic literature review, ethics approval was not required.
Results
We screened 3,175 citations in addition to the 29 papers that were included in the previous reviews. We included 44 studies with a total of 2,507,434 participants (3–24). The flow chart of the study selection is shown in Figure 1.
Characteristics of the included studies and participants are shown in Table 1. The included studies consist of 21 retrospective, 11 prospective and 12 post-hoc analyses. Geographical locations were diverse and included North America, Canada, Asia and Europe.
29 studies looked at patients with type 2 diabetes, whereas the remaining studies included patients with a mix of type 1 diabetes, type 2 diabetes, and impaired glucose tolerance/impaired fasting glucose. Four studies focussed on oral hypoglycaemics (37–39, 46). We report details of study validity (ascertainment of adverse outcomes, and confounding factors) in Table 2 and summarize the key features below.
Ascertainment of Hypoglycemia
Most of the studies relied on hospital or claims data records for severe hypoglycaemic events, ie hypoglycemia that requires help from another person to be managed/treated. 11 studies rely on either a history of self-reported hypoglycaemic episodes, questionnaires, or provided participants with diaries and glucometers (4–7, 10, 13, 16, 32, 34, 40, 45). These studies would be considered to be lower quality because of lack of medical documentation and high risk of recall bias.
Ascertainment of Adverse Events
12 studies used pre-specified outcomes from RCTs and one non-interventional study (5, 9–11, 13, 25, 34, 36, 40, 45, 46).
29 studies measured adverse events through database or medical records codes, one study relied on a professional interviewer with questionnaire (7) and one study on self-report/GP questionnaires (4). Dementia was ascertained though a wide variety of tests.
Confounding Factors
The included studies took account of potential confounding through the use of multivariate logistic regression models. Five studies used propensity score matching (18, 24, 34, 43, 47).
Meta-Analysis
Association Between Hypoglycemia and Macro- and Microvascular Disease and Cardiovascular Death
19 studies confirmed a significant association between hypoglycemia and macrovascular complications (3, 4, 10, 11, 14, 16, 17, 18, 20, 23, 26, 28, 34, 36, 38, 40, 43, 45, 46). The pooled odds ratio was 1.81 (95% CI 1.70–1.94). There was low heterogeneity (I2 = 6%).
Similarly, two studies confirmed a significant association between hypoglycemia and microvascular complications (43, 46). The microvascular complications covered in the study were nephropathy or retinopathy (46) and a composite endpoint of several complications (43). The pooled odds ratio was 1.77 (95% CI 1.49–2.10) with no evidence of heterogeneity (I2 = 0%) (Figure 2).
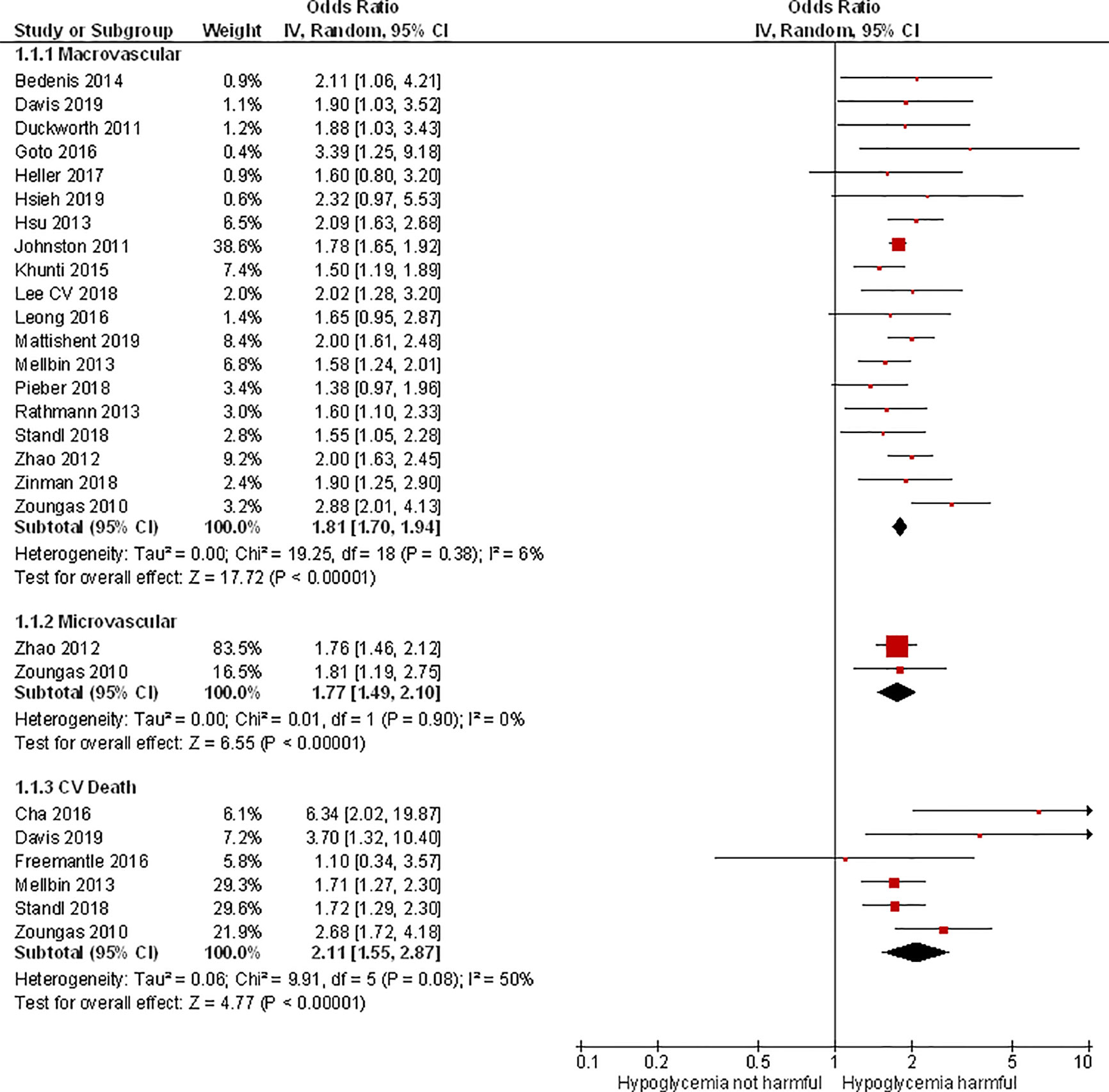
Figure 2 Meta-analysis of association between hypoglycemia and macro- and microvascular disease and cardiovascular death.
Six studies reported on cardiovascular death and confirmed a significant association between hypoglycaemia and cardiovascular death. The pooled odds ratio was 2.11 (95% CI 1.55–2.87) with evidence of moderate heterogeneity (I2 = 50%) (6, 10, 13, 34, 40, 46).
Association Between Hypoglycemia and Falls or Fractures
Six studies reported on falls (3, 7, 22, 30, 39, 44) with a pooled odds ratio of 1.78 (95% CI 1.44–2.21) and substantial heterogeneity (I2 = 87%).
Six studies reported on fractures with a pooled odds ratio of 1.68 (95% CI 1.37–2.07) and considerable heterogeneity (I2 = 91%) (3, 19, 20, 22, 35, 37) (Figure 3).
Association Between Hypoglycemia and Mortality
18 studies reported on overall mortality confirming a significant association between hypoglycemia and mortality with a pooled odds ratio of 2.02 (95% CI 1.75–2.32) and substantial heterogeneity (I2 = 86%) (3, 5, 6, 10, 12, 13, 18, 23, 25, 26, 31, 32, 34, 36, 40, 43, 45, 46) (Figure 4). Despite the heterogeneity, the direction of association was consistent across all the studies in the Forest plot. Two studies did not find a statistically significant association between hypoglycemia and mortality (13, 43).
We also conducted a sensitivity analysis for mortality hazard ratios (HRs) at different durations of follow-up, which three studies addressed (Figure 5). The HR is greatest early on [pooled HR 4.08 (95% CI 3.44–4.85) at 90-days follow-up] and diminishes with time after the hypoglycaemic episode [pooled HR 2.43 (95% CI 2.17–2.71) at 365-days follow-up] (3, 36, 45).
Association between hypoglycemia and dementia
9 studies confirmed a significant association between hypoglycemia and dementia (8, 9, 15, 24, 27, 33, 41, 42) with a pooled odds ratio of 1.50 (95% CI 1.29–1.74). There was substantial heterogeneity with I2 = 85% (Figure 6).
Sensitivity analysis – restriction to studies with patients’ mean age ≥65 years
As there is no consensus on the age-threshold for ‘older’ patients, we conducted a sensitivity analysis where we excluded studies in younger patients (mean age< 65 years). The pooled odds ratios were modestly increased when restricted to older patients, thus suggesting the possibility of greater harm associated with hypoglycemia with older age: Macrovascular events OR 1.88 (95% CI 1.72–2.07), Falls OR 1.98 (95% CI 1.80–2.19), and Death OR 2.25 (95% CI 1.78–2.83).
Publication Bias and Selective Outcome Reporting
We constructed a funnel plot for the meta-analysis on the association between hypoglycemia and vascular events, as more than ten studies were included in the analysis (see Supplemental Figure 1). On visual inspection of the funnel plot there are very few small studies that contributed to the meta-analysis, and it is difficult to judge presence or absence of asymmetry. As such, we cannot rule out the possibility of selective reporting or publication bias.
Discussion
This updated meta-analysis incorporated 23 new studies to the previously published meta-analyses on the association between hypoglycemia and adverse events in older people with diabetes. The total of 44 observational studies (involving over 2.5 million participants) confirms the danger of hypoglycemia in older people with diabetes, which is consistent with the previously published reviews.
Our meta-analyses demonstrated significant associations between hypoglycemia and death, dementia, macrovascular and microvascular complications, cardiovascular death, and falls and fractures. In our previous work, we were unable to report on cardiovascular death due to lack of data, but we have now been able to perform this meta-analysis with six studies (6 10, 13, 34, 40, 46).
In addition, our new sensitivity analysis of mortality HRs at different times of follow-up also shows that the HR for death is greatest early on and diminishes with longer follow-up duration. This suggests that the association between hypoglycaemic episodes and death is not just due to baseline confounding. If that were the case, we would not expect to see diminishing hazard ratios with longer intervals of time after the hypoglycaemic episode.
The collated evidence regarding serious harm supports our argument that we should prioritize the avoidance of hypoglycemia in this vulnerable group of patients.
An international consensus on clinical targets for continuous glucose monitoring data was published in June 2019, highlighted that older adults with diabetes should spend less than 15 minutes per day in the hypoglycaemic range (<3.9mmol/L) (48). This is of particular significance, as hypoglycaemic episodes are often missed in older people with diabetes (49).
We are aware of studies that have identified potential links between hypoglycemia and cardiac arrhythmias (50, 51), which could account in part for the findings of increased risk of myocardial infarction, stroke, falls and death following hypoglycemia.
Regarding cognitive adverse effects, a recent study found that hypoglycemia was associated with smaller total brain volume on MRI (27). Furthermore, Gibas et al. put forward the theory of “brain starvation” in patients with type 2 diabetes, due to concurrent hyperinsulinemia and relative hypoglycemia due to insulin resistance resulting in apoptosis of healthy neurons from catabolic degeneration (52). Radiological studies in patient who had suffered profound hypoglycemia have shown that neurons in the hippocampal and temporal areas, cerebral cortex, substantia nigra, and basal ganglia are particularly sensitive to hypoglycemia (53). Cognitive decline may in turn pre-dispose older frail people to falls, fractures and death following hypoglycemia.
Limitations
We cannot prove causality due to the observational nature of the studies. Although we identified heterogeneity in some of the meta-analyses, the direction of the effect was consistent amongst the studies. Factors which could be influencing heterogeneity include different classes of medications, different geographical locations, different study designs and the accuracy of ascertainment of hypoglycaemic episodes and adverse events.
We considered summarizing the evidence using GRADE, however, this tool is mainly designed for recommendations on healthcare intervention and not for etiology and prognostic studies. The two main areas within GRADE that cannot be applied here are ‘measure of indirectness’ and ‘estimation of absolute effect size’.
Regarding publication bias, if null or negative findings are not fully reported, this may result in inflated estimates of association in the meta-analyses. However, there were very few small studies in the funnel plot analysis we performed in relation to cardiovascular events, and so it is not possible for us to rule out bias from non-publication of small studies.
Conclusions
Our updated review provides a strong evidence base to support and strengthen our argument about the importance of adopting a hypoglycemia minimization strategy. Further work has to be carried out in older people with diabetes to establish effective hypoglycemia minimization strategies through better monitoring via continuous glucose monitoring coupled with de-intensification of management regimes, rather than the pursuit of specific HbA1c targets.
Author Contributions
KM and YKL designed the systematic review and meta-analysis, carried out the data extraction, analysis and drafted the manuscript. YKL is the guarantor. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fendo.2021.571568/full#supplementary-material
References
1. Mattishent K, Loke YK. Meta-analysis: Association between hypoglycemia and serious adverse events in older patients. J Diabetes Complications (2016) 30(5):811–8. doi: 10.1016/j.jdiacomp.2016.03.018
2. Mattishent K, Loke YK. Bi-directional interaction between hypoglycemia and cognitive impairment in elderly patients treated with glucose-lowering agents: a systematic review and meta-analysis. Diabetes Obes Metab (2016) 18(2):135–41. doi: 10.1111/dom.12587
3. Mattishent K, Richardson K, Dhatariya K, Savva GM, Fox C, Loke YK. The effects of hypoglycemia and dementia on cardiovascular events, falls and fractures and all-cause mortality in older people - a retrospective cohort study. Diabetes Obes Metab (2019) 21(9):2076–85. doi: 10.1111/dom.13769
4. Bedenis R, Price AH, Robertson CM, Morling JR, Frier BM, Strachan MW, et al. Association between severe hypoglycemia, adverse macrovascular events, and inflammation in the Edinburgh Type 2 Diabetes Study. Diabetes Care (2014) 37(12):3301–8. doi: 10.2337/dc14-0908
5. Bonds DE, Miller ME, Bergenstal RM, Buse JB, Byington RP, Cutler JA, et al. The association between symptomatic, severe hypoglycemia and mortality in type 2 diabetes: retrospective epidemiological analysis of the ACCORD study. BMJ (2010) 340:b4909. doi: 10.1136/bmj.b4909
6. Cha SA, Yun JS, Lim TS, Hwang S, Yim EJ, Song KH, et al. Severe Hypoglycemia and Cardiovascular or All-Cause Mortality in Patients with Type 2 Diabetes. Diabetes Metab J (2016) 40(3):202–10. doi: 10.4093/dmj.2016.40.3.202
7. Chiba Y, Kimbara Y, Kodera R, Tsuboi Y, Sato K, Tamura Y, et al. Risk factors associated with falls in elderly patients with type 2 diabetes. J Diabetes Complications (2015) 29(7):898–902. doi: 10.1016/j.jdiacomp.2015.05.016
8. Chin SO, Rhee SY, Chon S, Baik SH, Park Y, Nam MS, et al. Hypoglycemia is associated with dementia in elderly patients with type 2 diabetes mellitus: An analysis based on the Korea National Diabetes Program Cohort. Diabetes Res Clin Pract (2016) 122:54–61. doi: 10.1016/j.diabres.2016.09.027
9. Cukierman-Yaffe T, Bosch J, Jung H, Punthakee Z, Gerstein HC. Hypoglycemia and Incident Cognitive Dysfunction: A Post Hoc Analysis From the ORIGIN Trial. Diabetes Care (2019) 42(1):142–7. doi: 10.2337/dc18-0690
10. Davis SN, Duckworth W, Emanuele N, Hayward RA, Wiitala WL, Thottapurathu L, et al. Effects of Severe Hypoglycemia on Cardiovascular Outcomes and Death in the Veterans Affairs Diabetes Trial. Diabetes Care (2019) 42(1):157–63. doi: 10.2337/dc18-1144
11. Duckworth WC, Abraira C, Moritz TE, Davis SN, Emanuele N, Goldman S, et al. The duration of diabetes affects the response to intensive glucose control in type 2 subjects: the VA Diabetes Trial. J Diabetes Complications (2011) 25(6):355–61. doi: 10.1016/j.jdiacomp.2011.10.003
12. Escalada J, Liao L, Pan C, Wang H, Bala M. Outcomes and healthcare resource utilization associated with medically attended hypoglycemia in older patients with type 2 diabetes initiating basal insulin in a US managed care setting. Curr Med Res Opin (2016) 32(9):1557–65. doi: 10.1080/03007995.2016.1189893
13. Freemantle N, Danchin N, Calvi-Gries F, Vincent M, Home PD. Relationship of glycaemic control and hypoglycaemic episodes to 4-year cardiovascular outcomes in people with type 2 diabetes starting insulin. Diabetes Obes Metab (2016) 18(2):152–8. doi: 10.1111/dom.12598
14. Goto A, Goto M, Terauchi Y, Yamaguchi N, Noda M. Association Between Severe Hypoglycemia and Cardiovascular Disease Risk in Japanese Patients With Type 2 Diabetes. J Am Heart Assoc (2016) 5(3):e002875. doi: 10.1161/JAHA.115.002875
15. Haroon NN, Austin PC, Shah BR, Wu J, Gill SS, Booth GL. Risk of Dementia in Seniors With Newly Diagnosed Diabetes: A Population-Based Study. Diabetes Care (2015) 36(10):1868–75. doi: 10.2337/dc15-0491
16. Heller SR, Bergenstal RM, White WB, Kupfer S, Bakris GL, Cushman WC, et al. Relationship of glycated haemoglobin and reported hypoglycemia to cardiovascular outcomes in patients with type 2 diabetes and recent acute coronary syndrome events: The EXAMINE trial. Diabetes Obes Metab (2017) 19(5):664–71. doi: 10.1111/dom.12871
17. Hsieh YC, Liao YC, Li CH, Lin JC, Weng CJ, Lin CC, et al. Hypoglycaemic episodes increase the risk of ventricular arrhythmia and sudden cardiac arrest in patients with type 2 diabetes-A nationwide cohort study. Diabetes Metab Res Rev (2019) 36(2):e3226. doi: 10.1002/dmrr.3226
18. Hsu PF, Sung SH, Cheng HM, Yeh JS, Liu WL, Chan WL, et al. Association of clinical symptomatic hypoglycemia with cardiovascular events and total mortality in type 2 diabetes: a nationwide population-based study. Diabetes Care (2013) 36(4):894–900. doi: 10.2337/dc12-0916
19. Hung YC, Lin CC, Chen HJ, Chang MP, Huang KC, Chen YH, et al. Severe hypoglycemia and hip fracture in patients with type 2 diabetes: a nationwide population-based cohort study. Osteoporos Int (2017) 28(7):2053–60. doi: 10.1007/s00198-017-4021-4
20. Johnston SS, Conner C, Aagren M, Ruiz K, Bouchard J. Association between hypoglycaemic events and fall-related fractures in Medicare-covered patients with type 2 diabetes. Diabetes Obes Metab (2012) 14(7):634–43. doi: 10.1111/j.1463-1326.2012.01583.x
21. Johnston SS, Conner C, Aagren M, Smith DM, Bouchard J, Brett J. Evidence linking hypoglycemic events to an increased risk of acute cardiovascular events in patients with type 2 diabetes. Diabetes Care (2011) 34(5):1164–70. doi: 10.2337/dc10-1915
22. Kachroo S, Kawabata H, Colilla S, Shi L, Zhao Y, Mukherjee J, et al. Association between hypoglycemia and fall-related events in type 2 diabetes mellitus: analysis of a u.s. Commercial database. J Manag Care Spec Pharm (2015) 21(3):243–53. doi: 10.18553/jmcp.2015.21.3.243
23. Khunti K, Davies M, Majeed A, Thorsted BL, Wolden ML, Paul SK. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: a cohort study. Diabetes Care (2015) 38(2):316–22. doi: 10.2337/dc14-0920
24. Kim YG, Park DG, Moon SY, Jeon JY, Kim HJ, Kim DJ, et al. Hypoglycemia and Dementia Risk in Older Patients with Type 2 Diabetes Mellitus: A Propensity-Score Matched Analysis of a Population-Based Cohort Study. Diabetes Metab J (2019) 44(1):125–33. doi: 10.4093/dmj.2018.0260
25. Kong AP, Yang X, Luk A, Cheung KK, Ma RC, So WY, et al. Hypoglycemia, chronic kidney disease and death in type 2 diabetes: the Hong Kong diabetes registry. BMC Endocr Disord (2014) 14:48. doi: 10.1186/1472-6823-14-48
26. Lee AK, Warren B, Lee CJ, McEvoy JW, Matsushita K, Huang ES, et al. The Association of Severe Hypoglycemia With Incident Cardiovascular Events and Mortality in Adults With Type 2 Diabetes. Diabetes Care (2018) 41(1):104–11. doi: 10.2337/dc17-1669
27. Lee AK, Rawlings AM, Lee CJ, Gross AL, Huang ES, Sharrett AR, et al. Severe hypoglycemia, mild cognitive impairment, dementia and brain volumes in older adults with type 2 diabetes: the Atherosclerosis Risk in Communities (ARIC) cohort study. Diabetologia (2018) 61(9):1956–65. doi: 10.1007/s00125-018-4668-1
28. Leong A, Berkowitz SA, Triant VA, Porneala B, He W, Atlas SJ, et al. Hypoglycemia in Diabetes Mellitus as a Coronary Artery Disease Risk Factor in Patients at Elevated Vascular Risk. J Clin Endocrinol Metab (2016) 101(2):659–68. doi: 10.1210/jc.2015-3169
29. Lin CH, Sheu WH. Hypoglycaemic episodes and risk of dementia in diabetes mellitus: 7-year follow-up study. J Internal Med (2013) 273(1):102–10. doi: 10.1111/joim.12000
30. Lu CL, Hsu PC, Shen HN, Chang YH, Chen HF, Li CY. Association Between History of Severe Hypoglycemia and Risk of Falls in Younger and Older Patients With Diabetes. Medicine (Baltimore) (2015) 94(33):e1339. doi: 10.1097/MD.0000000000001339
31. Majumdar SR, Hemmelgarn BR, Lin M, McBrien K, Manns BJ, Tonelli M. Hypoglycemia associated with hospitalization and adverse events in older people : Population-based cohort study. Diabetes Care (2013) 36(11):3585–90. doi: 10.2337/dc13-0523
32. McCoy RG, Van Houten HK, Ziegenfuss JY, Shah ND, Wermers RA, Smith SA. Increased mortality of patients with diabetes reporting severe hypoglycemia. Diabetes Care (2012) 35(9):1897–901. doi: 10.2337/dc11-2054
33. Mehta HB, Mehta V, Goodwin JS. Association of Hypoglycemia With Subsequent Dementia in Older Patients With Type 2 Diabetes Mellitus. J Gerontol A Biol Sci Med Sci (2017) 72(8):1110–6. doi: 10.1093/gerona/glw217
34. Origin Trial Investigators, Mellbin LG, Ryden L, Riddle MC, Probstfield J, Rosenstock J, et al. Does hypoglycemia increase the risk of cardiovascular events? A report from the ORIGIN trial. Eur Heart J (2013) 34(40):3137–44. doi: 10.1093/eurheartj/eht332
35. Ntouva A, Toulis KA, Keerthy D, Adderley NJ, Hanif W, Thayakaran R, et al. Hypoglycemia is associated with increased risk of fractures in patients with type 2 diabetes mellitus: a cohort study. Eur J Endocrinol (2019) 180(1):51–8. doi: 10.1530/EJE-18-0458
36. Pieber TR, Marso SP, McGuire DK, Zinman B, Poulter NR, Emerson SS, et al. DEVOTE 3: temporal relationships between severe hypoglycemia, cardiovascular outcomes and mortality. Diabetologia (2018) 61(1):58–65. doi: 10.1007/s00125-017-4422-0
37. Rajpathak SN, Fu C, Brodovicz KG, Engel SS, Lapane K. Sulfonylurea use and risk of hip fractures among elderly men and women with type 2 diabetes. Drugs Aging (2015) 32(4):321–7. doi: 10.1007/s40266-015-0254-0
38. Rathmann W, Kostev K, Gruenberger JB, Dworak M, Bader G, Giani G. Treatment persistence, hypoglycemia and clinical outcomes in type 2 diabetes patients with dipeptidyl peptidase-4 inhibitors and sulphonylureas: a primary care database analysis. Diabetes Obes Metab (2013) 15(1):55–61. doi: 10.1111/j.1463-1326.2012.01674.x
39. Signorovitch JE, Macaulay D, Diener M, Yan Y, Wu EQ, Gruenberger JB, et al. Hypoglycemia and accident risk in people with type 2 diabetes mellitus treated with non-insulin antidiabetes drugs. Diabetes Obes Metab (2013) 15(4):335–41. doi: 10.1111/dom.12031
40. Standl E, Stevens SR, Armstrong PW, Buse JB, Chan JCN, Green JB, et al. Increased Risk of Severe Hypoglycemic Events Before and After Cardiovascular Outcomes in TECOS Suggests an At-Risk Type 2 Diabetes Frail Patient Phenotype. Diabetes Care (2018) 41(3):596–603. doi: 10.2337/dc17-1778
41. Whitmer RA, Karter AJ, Yaffe K, Quesenberry CP Jr., Selby JV. Hypoglycemic episodes and risk of dementia in older patients with type 2 diabetes mellitus. Jama (2009) 301(15):1565–72. doi: 10.1001/jama.2009.460
42. Yaffe K, Falvey CM, Hamilton N, Harris TB, Simonsick EM, Strotmeyer ES, et al. Association between hypoglycemia and dementia in a biracial cohort of older adults with diabetes mellitus. JAMA Intern Med (2013) 173(14):1300–6. doi: 10.1001/jamainternmed.2013.6176
43. Zhao Y, Campbell CR, Fonseca V, Shi L. Impact of hypoglycemia associated with antihyperglycemic medications on vascular risks in veterans with type 2 diabetes. Diabetes Care (2012) 35(5):1126–32. doi: 10.2337/dc11-2048
44. Zhao Y, Kachroo S, Kawabata H, Colilla S, Mukherjee J, Fonseca V, et al. Association between Hypoglycemia and Fall-Related Fractures and Health Care Utilization in Older Veterans with Type 2 Diabetes. Endocr Pract (2015) 22(2):P196–204. doi: 10.4158/EP15640.OR
45. Zinman B, Marso SP, Christiansen E, Calanna S, Rasmussen S, Buse JB, et al. Hypoglycemia, Cardiovascular Outcomes, and Death: The LEADER Experience. Diabetes Care (2018) 41(8):1783–91. doi: 10.2337/dc17-2677
46. Zoungas S, Patel A, Chalmers J, de Galan BE, Li Q, Billot L, et al. Severe hypoglycemia and risks of vascular events and death. N Engl J Med (2010) 363(15):1410–8. doi: 10.1056/NEJMoa1003795
47. Goto A, Arah OA, Goto M, Terauchi Y, Noda M. Severe hypoglycemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. BMJ (2013) 347:f4533. doi: 10.1136/bmj.f4533
48. Battelino T, Danne T, Bergenstal RM, Amiel SA, Beck R, Biester T, et al. Clinical Targets for Continuous Glucose Monitoring Data Interpretation: Recommendations From the International Consensus on Time in Range. Diabetes Care (2019) 42(8):1593–603. doi: 10.2337/dci19-0028
49. Mattishent K, Loke YK. Detection of asymptomatic drug-induced hypoglycemia using continuous glucose monitoring in older people - Systematic review. J Diabetes Complications (2018) 32(8):805–12. doi: 10.1016/j.jdiacomp.2018.05.005
50. Pistrosch F, Ganz X, Bornstein SR, Birkenfeld AL, Henkel E, Hanefeld M. Risk of and risk factors for hypoglycemia and associated arrhythmias in patients with type 2 diabetes and cardiovascular disease: a cohort study under real-world conditions. Acta Diabetol (2015) 52(5):889–95. doi: 10.1007/s00592-015-0727-y
51. Fitzpatrick C, Chatterjee S, Seidu S, Bodicoat DH, Ng GA, Davies MJ, et al. Association of hypoglycemia and risk of cardiac arrhythmia in patients with diabetes mellitus: A systematic review and meta-analysis. Diabetes Obes Metab (2018) 20(9):2169–78. doi: 10.1111/dom.13348
52. Gibas KJ. The starving brain: Overfed meets undernourished in the pathology of mild cognitive impairment (MCI) and Alzheimer’s disease (AD). Neurochem Int (2017) 110:57–68. doi: 10.1016/j.neuint.2017.09.004
Keywords: hypoglycemia, older people, diabetes, adverse effects, meta-analysis
Citation: Mattishent K and Loke YK (2021) Meta-Analysis: Association Between Hypoglycemia and Serious Adverse Events in Older Patients Treated With Glucose-Lowering Agents. Front. Endocrinol. 12:571568. doi: 10.3389/fendo.2021.571568
Received: 03 August 2020; Accepted: 11 January 2021;
Published: 08 March 2021.
Edited by:
Stefan Zoltán Lutz, Bad Sebastiansweiler, GermanyCopyright © 2021 Mattishent and Loke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katharina Mattishent, k.mattishent@uea.ac.uk
 Katharina Mattishent
Katharina Mattishent Yoon K. Loke
Yoon K. Loke