On the Relationship Between White Matter Structure and Subjective Pain. Lessons From an Acute Surgical Pain Model
- 1Department of Oral Surgery and Implant Dentistry, School of Dentistry, University of Granada, Granada, Spain
- 2Mind, Brain and Behavior Research Center (CIMCYC), University of Granada, Granada, Spain
- 3Department of Pathology, School of Medicine and Instituto de Biopatología y Medicina Reparativa, University of Granada, Granada, Spain
Background: Pain has been associated with structural changes of the brain. However, evidence regarding white matter changes in response to acute pain protocols is still scarce. In the present study, we assess the existence of differences in brain white matter related to pain intensity reported by patients undergoing surgical removal of a mandibular impacted third molar using diffusion tensor imaging (DTI) analysis.
Methods: 30 participants reported their subjective pain using a visual analog scale at three postsurgical stages: under anesthesia, in pain, and after the administration of an analgesic. The diffusion data were acquired prior to surgery.
Results: DTI analysis yielded significant positive associations of fractional anisotropy in white matter areas related to pain processing (corticospinal tract, corona radiata, corpus callosum) with the differences in pain between the three postsurgery stages. Extent and location of these associations depended on the magnitude of the subjective pain differences. Tractography analysis indicated that some pain–tract associations are significant only when pain stage is involved in the contrast (posterior corona radiata), while others (middle cerebellar peduncle, pontine crossing) are only when anesthesia is involved in the contrast.
Conclusions: The association of white matter fractional anisotropy and connectivity, measured before the pain stages, with subjective pain depends on the magnitude of the differences in pain scores.
Introduction
Chronic pain has been associated with structural changes of the brain, including prefrontal, somatosensory and occipital areas and subcortical nuclei (Cauda et al., 2014; Kuner and Flor, 2017; Yuan et al., 2017; Shokouhi et al., 2018). Gray matter structural changes have been observed in chronic pain conditions (Diaz-Piedra et al., 2016; Jia and Yu, 2017; Wang et al., 2017) as well as changes in white matter (Jutzeler et al., 2016; Tian et al., 2016; Hotta et al., 2017; Malfliet et al., 2017; Zhong et al., 2018).
Brain morphometric alterations have been documented also in acute pain conditions (Emerson et al., 2014), indicating that the volume of some pain-processing brain regions can be affected by them (Elsenbruch et al., 2014), even when the strength of these associations is rather modest (4–5% Stankewitz et al., 2013) or nonsignificant (i.e., pressure pain threshold Ruscheweyh et al., 2018). Brain functional changes have been reported after repetitive pain stimulation (Stankewitz et al., 2013), especially in subgenual anterior cingulate. These changes last up to 1 year (Bingel et al., 2008), indicating that habituation to painful stimuli is key in pain perception (Ginzburg et al., 2015). Repetitive pain stimulation changes gray matter concentration of pain-related areas in individuals who do not show habituation (Stankewitz et al., 2013). However, gray matter changes tend to recede when the nociceptive input stops (Teutsch et al., 2008), or the chronic pain is relieved (Lewis et al., 2018). This suggests that acute pain can be associated with brain structural changes, and the association between brain structure and pain can be observed independently of contextual factors or level of pain experienced. Evidence regarding white matter changes in response to acute pain protocols is scarce, although some reports of abnormal regional fractional anisotropy (FA) and structural connectivity, measured by tractography, in the prefrontal cortex may underlie the transition (Chapman and Vierck, 2017) from acute to chronic pain (Vachon-Presseau et al., 2016).
The present study aims to determine whether white matter integrity and structure are associated with acute pain, and more specifically, whether variations in pain intensity are linked to fractional anisotropy and white matter connectivity. We used an orofacial pain model, the extraction of mandibular impacted third molars. This pain lasts for hours, but its intensity changes in accordance with three typical stages: (1) Anesthesia, applied before the surgery and lasting approx 3 h, (2) pain, cessation of the anesthetic agent, and (3) analgesia, postoperative medication prescribed. Patients were asked to indicate their pain intensity at the three stages (hereafter, subjective pain). We hypothesize that subjective pain will differ between stages, so that pain is greater than anesthesia, pain is greater than analgesia, and anesthesia is greater than analgesia, but the associations of these differences in subjective pain and white matter structure must remain constant, as there is no time for structural changes to happen, as our protocol lasted 4 h, and there is no scientific literature pointing out to changes in white or gray matter in such a sort of period of time. Furthermore, if changes were observed this will indicate that these associations reflect the recruitment of more (or less) structures to process pain, rather than a change in the nature of the pain–brain structure relationships.
Materials and Methods
Participants
This prospective study was conducted after approval by the University of Granada Ethics Committee on Human Research (n° 877) and in accordance with the Declaration of Helsinki for treatment of experimental human subjects (Williams, 2008), and it adheres to the applicable STROBE guidelines. Subjects received detailed information about the surgical and scanning procedures and they or their legal representatives provided written informed consent.
A total of 30 subjects (23 women) were recruited for the present study (mean age, 21.83 years, range 18–32 years). Participants were healthy and were included only if they had a mandible impacted third molar which needed surgical procedure to be removed, but they were completely free of pain at the start of the study. All molars were located in the mandible (50% left). Participants were recruited from the pool of patients/students of the School of Dentistry of the University of Granada and were part of a larger study on the effects of oral surgery on brain structure and function. Power analysis (α = 0.05, power = 0.9, and partial R-square = 0.3) on subjective measures suggested a total sample size of 27 participants. We added three more participants, assuming a dropout of 10%.
Surgical Procedure and Pain Measurement
The third molars were extracted by an expert oral surgeon (PGM) following a standardized surgical procedure performed at the School of Dentistry at University of Granada. In short, an inferior alveolar and buccal nerve block was given using 1.8-mL carpule of 2% articaine with adrenaline 1:100,000. Surgical access was routinely achieved buccally through a triangular flap. Bone removal around the tooth was then performed with a round bur on a straight hand-piece under continuous irrigation. Crown and/or roots were sectioned when necessary. After extraction, the socket was inspected and the flap was sutured back by 2–4 interrupted stitches using a 3–0 silk suture. Gauze impregnated with either chlorhexidine or hyaluronic acid was applied over the socket, and the usual post extraction instructions were given written to the patient. All the patients received routinely the following postoperative medication: amoxicillin/clavulanic acid 2 g twice a day and dexketoprofen 25 mg three times a day for 7 days; metamizole 565 mg was given as a rescue analgesic. The duration of surgery (from the incision to the extraction) and the duration of the anesthetic agent in minutes, among others, were recorded.
Patients were asked to report their subjective pain using a visual analog Likert-type scale (hereafter, subjective pain), in which 0 meant “no pain at all” and 10 meant “worst pain imaginable,” at three different times: anesthesia, pain, and analgesia. The anesthesia scoring was taken 30 min after the surgical procedure, and patients were still under anesthesia effects (anesthesia stage). The second measure was taken either when local anesthetic ceased its function, as reported by the participant, or 3 h after the extraction (pain stage). At this moment, patients were supposed to be at the pain peek, caused by the surgical trauma provoked by the dental surgery. The length of these two intervals (30 min and 3 h.) was selected according to Senes et al. (2015), who reported anesthesia durations around 3 h. Then, all participants were given an analgesic (Metamizole 565 mg, Laboratorios Normon S.A, Spain) in order to reduce their pain. Thirty minutes after the analgesic, the last measure of pain was taken (analgesia stage). This interval was based on Schmieder et al. (1993) metamizole onset time 10.9 (±5.8) min.
DTI Scanning
Participants were scanned before the surgery using a DTI diffusion scheme. The diffusion images were acquired on a SIEMENS Trio Tim scanner located at the Mind, Brain and Behavior Research Center of the University of Granada using a 2D EPI diffusion sequence, with TE = 90 ms, and TR = 3,300 ms. A HARDI scheme was used, and a total of 30 diffusion sampling directions were acquired, three times each. The b-value was 1,000 s/mm2. A non-diffusion scan was obtained with b-value = 0 s/mm2. The in-plane resolution was 1.8 mm. The slice thickness was 5.2 mm. A T1-weighted anatomical scan was also obtained for each participant using a MPRAGE sequence (TR = 1,900 ms; TE = 2.52 ms; flip angle = 9°, voxel size = 1 × 1 × 1 mm3; FOV = 256 × 256 mm2; matrix size = 256 × 256, 176 slices). The average interval between session and third molar surgery was 23.6 (±42.41) days.
White Matter Analysis
White Matter Integrity
Diffusion tensor imaging analysis was carried out using the FB Software Library (FSL, https://fsl.fb.ox.ac.uk/fsl Jenkinson et al., 2012), which includes eddy current and motion correction, brain mask extraction (BET v2.1 Smith, 2002), reconstruction of the diffusion tensors (DTIFIT), and computation of fractional anisotropy (FA). Mean diffusivity (MD) was obtained as the average of the three eigenvalues (L1, L2, L3). Axial diffusivity (AD) was obtained as the first eigenvalue (L1). Voxel-wise Tract-Based Spatial Statistics (TBSS), a part of the FSL software, was used to examine the association of the differences between subjective pain intensities at the three postsurgical stages (pain–anesthesia, pain–analgesia, and anesthesia–analgesia) and FA, MD, and AD. In short, all the FA volumes were nonlinearly registered to the FB58-FA template (https://fsl.fb.ox.ac.uk/fsl/fslwiki/data/FB58_FA.html) and aligned to the Montreal Neurological Institute space. A FA skeleton was created by first averaging all the FA volumes and thinning the average, with a 0.2 FA threshold. The aligned FA volume of each participant was projected onto this FA skeleton and submitted to the statistical analysis. A randomization procedure (2,000 random permutations, FSL's randomize software) was used to perform the multiple regression analysis, in which the variables of interest were the between-stage differences in pain intensity, and the nuisances were age and gender. The results were corrected using threshold-free cluster enhancement (TFCE) correction for multiple comparisons (family-wise error rate p = 0.05). The same analyses were applied to the MD and AD volumes, after aligning them into the MNI space and projecting them onto the mean FA skeleton using the non-FA script included in FSL. No significant effects were observed in MD and AD.
Connectometry Analysis
The diffusion data were eddy and motion corrected and averaged across repetitions to improve the signal-to-noise ratio. The volumes were reconstructed in MNI space using q-space diffeomorphic reconstruction (Yeh et al., 2011) to obtain the spin distribution function (SDF) (Yeh et al., 2010). The diffusion sampling length ratio was 1.25. The output resolution was 2 mm.
Diffusion magnetic resonance imaging (MRI) connectometry (Yeh et al., 2016) was used to study the association of pain intensity with white matter spin distribution function. The SDF measures the density of water diffusion, instead of the speed of water diffusion, as diffusivity measures do. Connectometry analysis tracks de association, so that the first identifies voxels with a high association and then tracks along the fiber direction to determine the consecutive fiber segments that also show that association. We used a multiple-regression analysis, in which the predictors of interest were the between-stage differences in pain intensity: anesthesia–pain, pain–analgesia, and anesthesia–analgesia. The variables of no interest were gender and age. One t-tresholds (3.02) were used to select local connectomes to provide high sensitivity (lower threshold) and high specificity (higher threshold). A deterministic fiber-tracking algorithm, implemented in DSI_Studio (http://dsi-studio.labsolver.org/; Yeh et al., 2013), was used to estimate fiber directions in whole-brain regions. All tracks generated from bootstrap resampling were included. The length threshold to select tracks was 40 mm. The seeding density was 20 seeds/mm3. We used a p < 0.05 false discovery ratio (FDR) to control for the multiple-comparison problem. FDR was estimated in a total of 2,000 random permutations to determine the null distribution of track length. All the analyses were done using DSI Studio.
Results
Subjective pain intensities were higher at the pain stage than at the anesthesia [averages = 4.3 and 5.5, respectively, t(29) = 4.15, p < 0.001] and analgesia [average= 2.25, t(29) = 6.81, p < 0.001] stages and were higher at anesthesia than at analgesia [t(29) = 4.41, p < 0.001].
Diffusivity
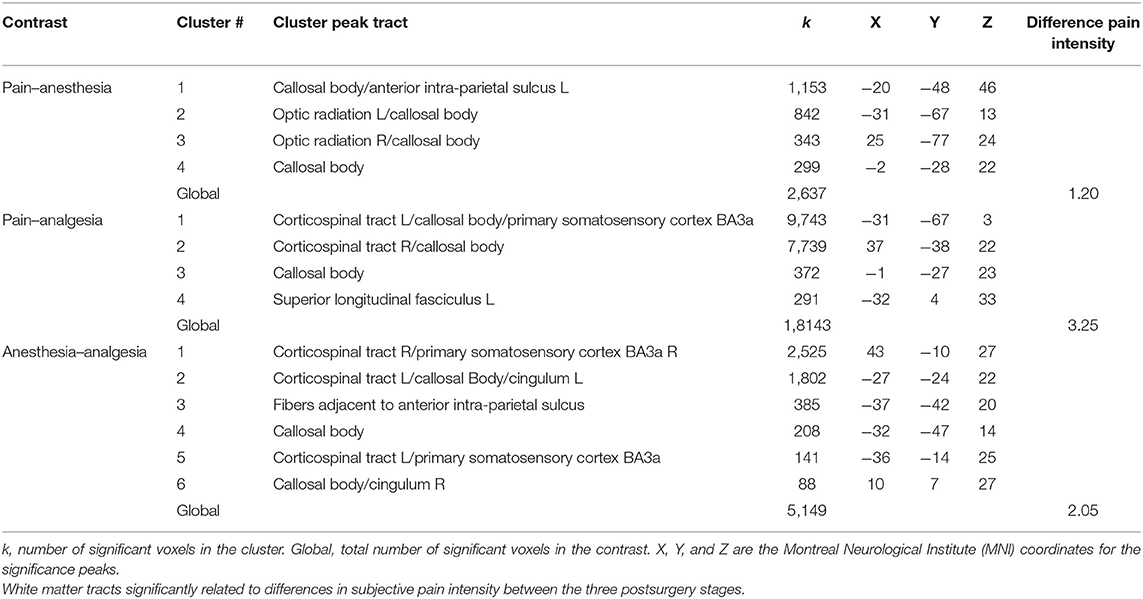
The positive associations between FA and the difference between pain intensities (pain–anesthesia, pain–analgesia, and anesthesia–analgesia) are displayed in Table 1 and Figure 1. No negative associations were observed. The set of significant tracts, according to the Juelich Histological atlas, included in FSL, embraces posterior parts of corpus callosum (splenium), and left and right corticospinal tract. Figure 1A shows that the location of these tracts partially overlaps (Figure 1B) but also that there are unique areas associated with each one of the subjective pain difference (Table 1). No differences were observed as a function of the surgery location (all corrected p > 0.22). Moreover, the number of significant voxels seems to depend on the size of the difference between postsurgical stages, that is, between subjective pain intensities (Table 1). No differences were observed for MD and AD.
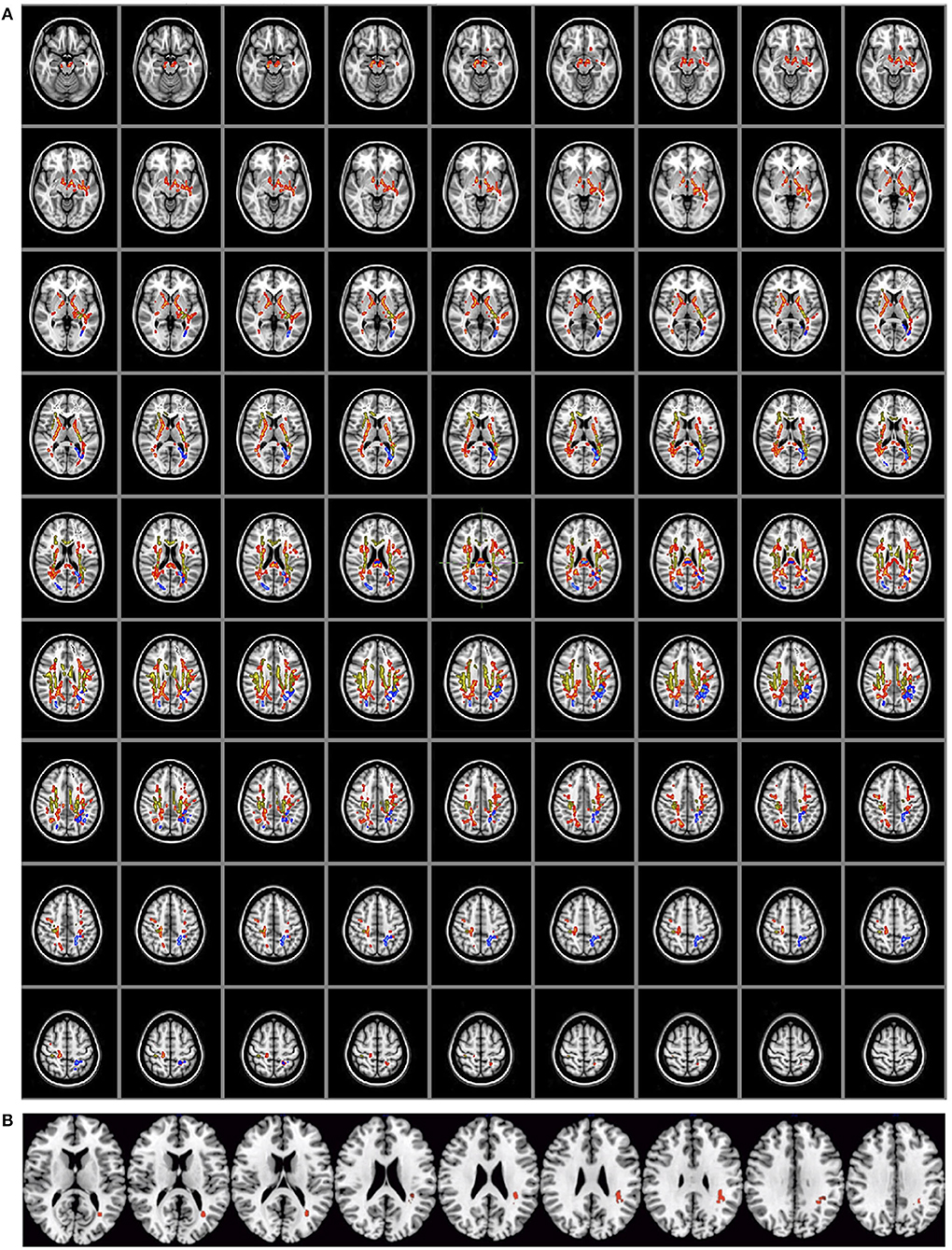
Figure 1. (A) Diffusivity (n = 30). Significant positive associations of fractional anisotropy with differences in pain intensities between the three stages: pain–anesthesia (blue), pain–analgesia (red), and anesthesia–analgesia (yellow). (B) Areas (right superior longitudinal fasciculus) in which the three associations overlap.
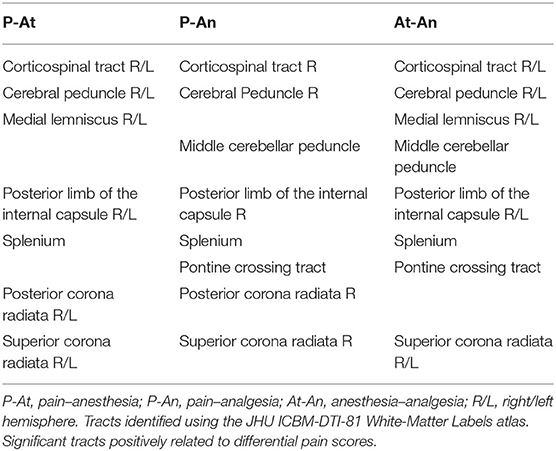
Connectivity
The connectometry analysis (Table 2, Figure 2) identified significant increased tracks connectivity (FDR corrected p < 0.05) related to pain–anesthesia, to pain–analgesia, and anesthesia–analgesia subjective pain differences. We observed significant associations in cerebral peduncles, corticospinal tracts, medial lemniscus, splenium of the corpus callosum, and posterior limb of the internal capsule. Middle cerebellar peduncle and superior corona radiata are involved only when analgesia postsurgical stage enters into the contrast (pain–analgesia and anesthesia–analgesia). No tracts showed significant decreased connectivity related to any of the differences between subjective pain intensities.
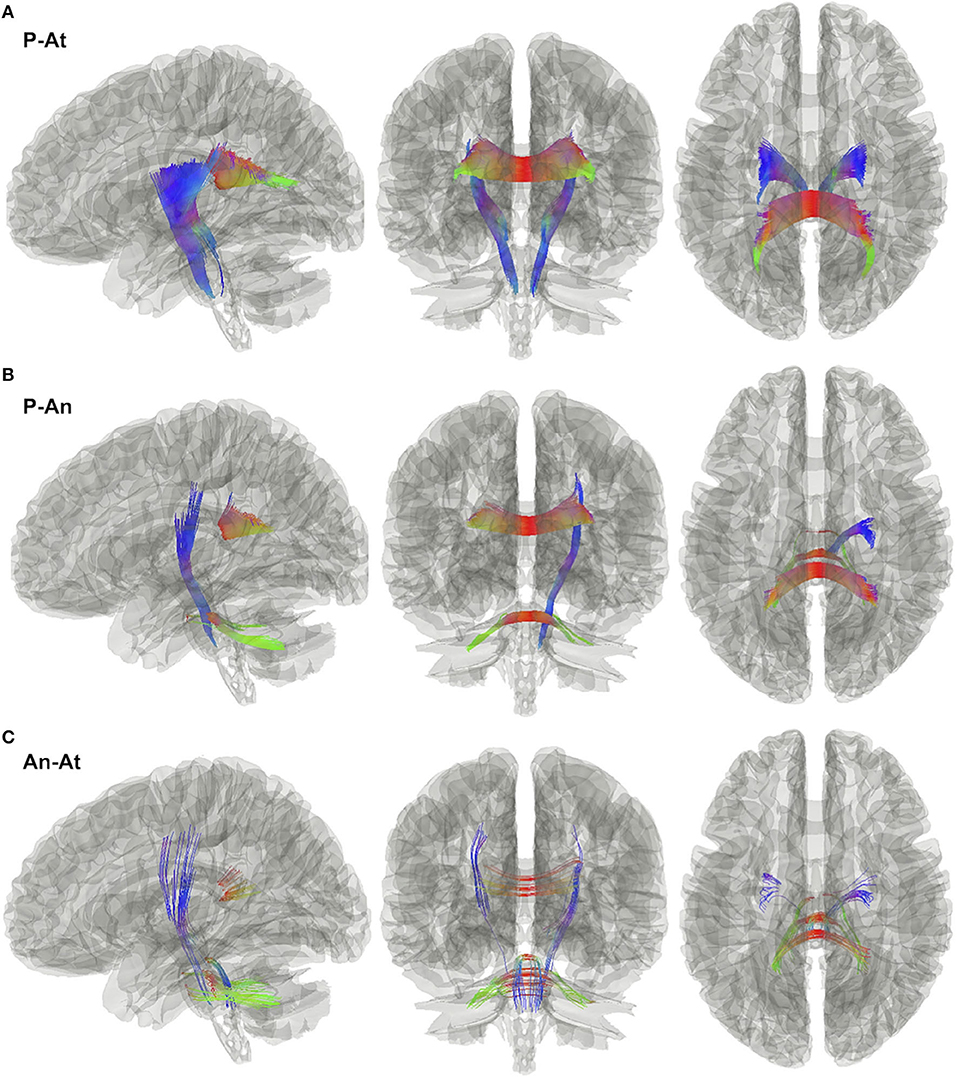
Figure 2. White matter tracks (n = 30) positively associated with subjective pain intensity differences between the three postsurgical stages. (A) Pain–anesthesia, (B) pain–analgesia, and (C) anesthesia–analgesia at the 2.5 threshold.
Discussion
Two main results have been observed in this study: first, the association of pain with white matter integrity and connectivity, and second, the dependency of these associations of the level of pain experienced during the protocol. The causal role of pain on brain structure has been a matter of intense research during the last decades. Nowadays, data on brain gray matter volume and white matter integrity suggest that pain is strongly associated with brain morphology changes and plasticity (Chapman and Vierck, 2017; Kuner and Flor, 2017). Most of these data have been observed when using a between-subject approach, in which a chronic pain condition is commonly compared with a non-pain one. Here, we used a postsurgical pain model (third impacted molar) in which pain changes from the anesthesia stage, immediately posterior to the surgery, followed by a short pain stage, to the final analgesia stage. These pain changes happen in such a short time interval (a few hours) that changes in brain structure are extremely improbable, and, therefore, a single pre-surgery DTI scan allows us to ascertain, first, whether acute pain is associated with white matter integrity and connectivity, and, second, whether these associations depended on the level of experienced acute pain.
The white matter tracts we have observed in the present study are involved in the processing of pain, including orofacial one (Moayedi et al., 2012; Wang et al., 2017). The medial lemniscus pathway, specially its medial border, conveys information from the principal sensory nucleus and the spinal nucleus, whose afferents are originated in the oral cavity, and play a role in the transmission of propioceptive information, including pain after mechanical stimulation (Henssen et al., 2016). Similarly, associations of pain with sensorimotor tracts can be related to the differences in the inputs originated in the oral cavity (Moayedi et al., 2012) between the three postsurgery stages that may influence the perceived pain. However, as DTI is unable to discriminate ascending from descending pathways, we cannot discard that motor commands to the orofacial region can be a function of the postsurgery stage, which again influences the subjective experience of pain. The cerebellum has also a role in pain perception (Bocci et al., 2015), probably because nociceptive information is conveyed to the Purkinje cells either by the spino-olivocerebellar or by the spino-pontocerebellar pathways (Baumann et al., 2015). Moreover, the fact that pontine crossing tract (the entry points of cortical inputs to the cerebellum via middle cerebellar peduncle) connectivity is significant when analgesia stage is involved in the statistical contrast suggests that at least part of the difference in pain intensity can depend on the processing of nociceptive inputs performed by cerebellum.
There is abundant literature showing that the anisotropy of the remaining brain areas observed in our study (as corpus callosum, internal capsule, corona radiata, or superior longitudinal fasciculus) seem to be altered in chronic pain (Moayedi et al., 2012; Yoon et al., 2013; Yu et al., 2013; Lieberman et al., 2014). Little evidence is available on the relationship between acute pain and white matter integrity. Using functional DTI (fDTI), a decrease in FA in response to painful stimulation in the contralateral spinothalamic tract has been observed (Lin et al., 2018). This change is specific to the stimulation as the control region does not showed FA alterations. An association between fMRI BOLD response and fractional anisotropy of the midcingulate cortex in response to thermal stimulation has been also observed, so that the functional response was positively correlated with the FA in internal capsule and negatively to that of the cingulum (Warbrick et al., 2016). In the same vein, our results points out that the association of white matter integrity measures and acute pain does not only indicate potential changes in brain structure but that the strength of the association can depend on the actual pain intensity (Liu et al., 2017), even when the white matter integrity is assessed before the pain induction protocol.
Our results have some limitations that are important to take into account. Firstly, sample size can be limited as a consequence of the pain model we have used in our study. However, we have run a power analysis, based on the subjective measures that have the aim to overcome this limitation. Secondly, we have used a subjective pain assessment scale, which cannot discriminate between the different dimensions of pain experience. A more objective measure of pain can produce a different set of results. However, one very important component of pain is how one feels about, that is, the subjective part, which indicates that our results can be interesting in this regard. Thirdly, we have used a b-value of 1,000 s/mm2 that will render more difficult to resolve intravoxel crossing fibers (Xie et al., 2015). Further research will be needed in order to disentangle the associations of these dimensions with brain white matter integrity and connectivity. Finally, the cultural and socioeconomic level of our participants is medium-high, which can have an impact on the subjective ratings of pain and on the generality of our results. Further research is needed in order to determine whether the associations we have observed here hold for other cultural and socioeconomic statuses.
Acute pain is associated with white matter integrity, measured by FA, and connectivity, measured by connectometry. FA results suggest that both specific tracts (and number of voxels) associated with pain are a function of the differential level of acute pain. Connectometry results suggest that the white matter tracts (corticospinal tract, medial lemniscus pathway, corpus callosum, middle cerebellar peduncle, and corona radiata) typically involved in pain processing are related to the differences in pain intensity in between the postsurgical stages (anesthesia, pain, analgesia), but the strength of these relationships, as measured by the total count of fibers, seems to depend more on the differences between types of pain relief (anesthesia, analgesia). Specifically, we observed that the difference between the pain stage and the anesthesia stage (the lower difference in subjective pain) embraced much more bilateral tracts than that between pain–analgesia or anesthesia–analgesia (that uniquely involved middle cerebellar peduncle and pontine crossing). Thus, it seems that the number of fibers showing a significant association can depend more on the action mechanisms or the pain-relief effectivity of anesthesia and analgesia than on the action mechanisms of subjective pain.
Summary Statement
The association of white matter fractional anisotropy and connectivity, measured before the pain stages, with subjective pain depends on the magnitude of the differences in pain scores.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary materials, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by University of Granada Ethics Committee on Human Research (n° 877). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
AC and PG-M: conceptualization, methodology, and supervision. AC: data curation and resources. AC, LT-M, and CS-G: formal analysis. AC and LT-M: investigation. AC, PG-M, and LT-M: project administration. AC, PG-M, LT-M, MP-M, CS-G, and FO'V: visualization and writing. All authors contributed to the article and approved the submitted version.
Funding
The present article part of the investigation performed during the course of LT-M PhD studies at University of Granada (Spain). This investigation was partially supported by the Research Groups #CTS-138, #CTS-176 and #CTS-1028 (Junta de Andalucía, Spain). LT-M was supported by the Talentia Scholarship Program of the Regional Ministry for Innovation, Science, and Enterprise (Junta de Andalucía). Research by AC was funded by a Spanish Ministry of Economy and Competitiveness grant (PSI2012-39292 to AC). MP-M was supported by the Andalucía Talent Hub Program from the Andalusian Knowledge Agency, cofunded by the European Union's Seventh Framework Program, Marie Skłodowska-Curie actions (COFUND – Grant Agreement n° 291780 to MP-M) and the Ministry of Economy, Innovation, Science and Employment of the Junta de Andalucía.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Baumann, O., Borra, R. J., Bower, J. M., Cullen, K. E., Habas, C., Ivry, R. B., et al. (2015). Consensus paper: the role of the cerebellum in perceptual processes. Cerebellum 14, 197–220. doi: 10.1007/s12311-014-0627-7
Bingel, U., Herken, W., Teutsch, S., and May, A. (2008). Habituation to painful stimulation involves the antinociceptive system–a 1-year follow-up of 10 participants. Pain 140, 393–394. doi: 10.1016/j.pain.2008.09.030
Bocci, T., Santarcangelo, E., Vannini, B., Torzini, A., Carli, G., Ferrucci, R., et al. (2015). Cerebellar direct current stimulation modulates pain perception in humans. Restor. Neurol. Neurosci. 33, 597–609. doi: 10.3233/RNN-140453
Cauda, F., Palermo, S., Costa, T., Torta, R., Duca, S., Vercelli, U., et al. (2014). Gray matter alterations in chronic pain: a network-oriented meta-analytic approach. Neuroimage Clin. 4, 676–686. doi: 10.1016/j.nicl.2014.04.007
Chapman, C. R., and Vierck, C. J. (2017). The transition of acute postoperative pain to chronic pain: an integrative overview of research on mechanisms. J. Pain 18, 359.e1–e38. doi: 10.1016/j.jpain.2016.11.004
Diaz-Piedra, C., Guzman, M. A., Buela-Casal, G., and Catena, A. (2016). The impact of fibromyalgia symptoms on brain morphometry. Brain Imaging Behav. 10, 1184–1197. doi: 10.1007/s11682-015-9485-2
Elsenbruch, S., Schmid, J., Kullmann, J. S., Kattoor, J., Theysohn, N., Forsting, M., et al. (2014). Visceral sensitivity correlates with decreased regional gray matter volume in healthy volunteers: a voxel-based morphometry study. Pain 155, 244–249. doi: 10.1016/j.pain.2013.09.027
Emerson, N. M., Zeidan, F., Lobanov, O. V., Hadsel, M. S., Martucci, K. T., Quevedo, A. S., et al. (2014). Pain sensitivity is inversely related to regional grey matter density in the brain. Pain 155, 566–573. doi: 10.1016/j.pain.2013.12.004
Ginzburg, K., Tsur, N., Karmin, C., Speizman, T., Tourgeman, R., and Defrin, R. (2015). Body awareness and pain habituation: the role of orientation towards somatic signals. J. Behav. Med. 38, 876–885. doi: 10.1007/s10865-015-9676-8
Henssen, D. J., Kurt, E., Kozicz, T., van Dongen, R., Bartels, R. H., and van Cappellen van Walsum, A. M. (2016). New insights in trigeminal anatomy: a double orofacial tract for nociceptive input. Front. Neuroanat. 10:53. doi: 10.3389/fnana.2016.00053
Hotta, J., Zhou, G., Harno, H., Forss, N., and Hari, R. (2017). Complex regional pain syndrome: the matter of white matter? Brain Behav. 7:e00647. doi: 10.1002/brb3.647
Jenkinson, M., Beckmann, C. F., Behrens, T. E., Woolrich, M. W., and Smith, S. M. (2012). FSL. Neuroimage 62, 782–790. doi: 10.1016/j.neuroimage.2011.09.015
Jia, Z., and Yu, S. (2017). Grey matter alterations in migraine: a systematic review and meta-analysis. Neuroimage Clin. 14, 130–140. doi: 10.1016/j.nicl.2017.01.019
Jutzeler, C. R., Huber, E., Callaghan, M. F., Luechinger, R., Curt, A., Kramer, J. L., et al. (2016). Association of pain and CNS structural changes after spinal cord injury. Sci. Rep. 6:18534. doi: 10.1038/srep18534
Kuner, R., and Flor, H. (2017). Structural plasticity and reorganisation in chronic pain. Nat. Rev. Neurosci. 18:113. doi: 10.1038/nrn.2017.5
Lewis, G. N., Parker, R. S., Sharma, S., Rice, D. A., and McNair, P. J. (2018). Structural brain alterations before and after total knee arthroplasty: a longitudinal assessment. Pain Med. 19, 2166–2176. doi: 10.1093/pm/pny108
Lieberman, G., Shpaner, M., Watts, R., Andrews, T., Filippi, C. G., Davis, M., et al. (2014). White matter involvement in chronic musculoskeletal pain. J. Pain 15, 1110–1119. doi: 10.1016/j.jpain.2014.08.002
Lin, J. C., Mueller, C., and Younger, J. W. (2018). Thermal stimulation changes diffusivity of the spinothalamic tract. Spine 43, E697–E702. doi: 10.1097/BRS.0000000000002472
Liu, J., Liu, H., Mu, J., Xu, Q., Chen, T., Dun, W., et al. (2017). Altered white matter microarchitecture in the cingulum bundle in women with primary dysmenorrhea: a tract-based analysis study. Hum. Brain Mapp. 38, 4430–4443. doi: 10.1002/hbm.23670
Malfliet, A., Coppieters, I., Van Wilgen, P., Kregel, J., De Pauw, R., Dolphens, M., et al. (2017). Brain changes associated with cognitive and emotional factors in chronic pain: a systematic review. Eur. J. Pain 21, 769–786. doi: 10.1002/ejp.1003
Moayedi, M., Weissman-Fogel, I., Salomons, T. V., Crawley, A. P., Goldberg, M. B., Freeman, B. V., et al. (2012). White matter brain and trigeminal nerve abnormalities in temporomandibular disorder. Pain 153, 1467–1477. doi: 10.1016/j.pain.2012.04.003
Ruscheweyh, R., Wersching, H., Kugel, H., Sundermann, B., and Teuber, A. (2018). Gray matter correlates of pressure pain thresholds and self-rated pain sensitivity: a voxel-based morphometry study. Pain 159, 1359–1365. doi: 10.1097/j.pain.0000000000001219
Schmieder, G., Stankov, G., Zerle, G., Schinzel, S., and Brune, K. (1993). Observer-blind study with metamizole versus tramadol and butylscopolamine in acute biliary colic pain. Arzneimittelforschung 43, 1216–1221.
Senes, A. M., Calvo, A. M., Colombini-Ishikiriama, B. L., Goncalves, P. Z., Dionisio, T. J., Sant'ana, E., et al. (2015). Efficacy and safety of 2% and 4% articaine for lower third molar surgery. J. Dent. Res. 94, 166S−73S. doi: 10.1177/0022034515596313
Shokouhi, M., Clarke, C., Morley-Forster, P., Moulin, D. E., Davis, K. D., and St. Lawrence, K. (2018). Structural and functional brain changes at early and late stages of complex regional pain syndrome. J. Pain 19, 146–157. doi: 10.1016/j.jpain.2017.09.007
Smith, S. M. (2002). Fast robust automated brain extraction. Hum. Brain Mapp. 17, 143–155. doi: 10.1002/hbm.10062
Stankewitz, A., Valet, M., Schulz, E., Woller, A., Sprenger, T., Vogel, D., et al. (2013). Pain sensitisers exhibit grey matter changes after repetitive pain exposure: a longitudinal voxel-based morphometry study. Pain 154, 1732–1737. doi: 10.1016/j.pain.2013.05.019
Teutsch, S., Herken, W., Bingel, U., Schoell, E., and May, A. (2008). Changes in brain gray matter due to repetitive painful stimulation. Neuroimage 42, 845–849. doi: 10.1016/j.neuroimage.2008.05.044
Tian, T., Guo, L., Xu, J., Zhang, S., Shi, J., Liu, C., et al. (2016). Brain white matter plasticity and functional reorganization underlying the central pathogenesis of trigeminal neuralgia. Sci. Rep. 6:36030. doi: 10.1038/srep36030
Vachon-Presseau, E., Tetreault, P., Petre, B., Huang, L., Berger, S. E., Torbey, S., et al. (2016). Corticolimbic anatomical characteristics predetermine risk for chronic pain. Brain 139, 1958–1970. doi: 10.1093/brain/aww100
Wang, Y., Cao, D. Y., Remeniuk, B., Krimmel, S., Seminowicz, D. A., and Zhang, M. (2017). Altered brain structure and function associated with sensory and affective components of classic trigeminal neuralgia. Pain 158, 1561–1570. doi: 10.1097/j.pain.0000000000000951
Warbrick, T., Fegers-Stollenwerk, V., Maximov, I. I., Grinberg, F., and Shah, N. J. (2016). Using structural and functional brain imaging to investigate responses to acute thermal pain. J. Pain 17, 836–844. doi: 10.1016/j.jpain.2016.03.009
Williams, J. R. (2008). The declaration of Helsinki and public health. Bull. World Health Organ. 86, 650–652. doi: 10.2471/BLT.08.050955
Xie, S., Zuo, N., Shang, L., Song, M., Fan, L., and Jiang, T. (2015). How does B-value affect HARDI reconstruction using clinical diffusion MRI data? PLoS ONE 10:e0120773. doi: 10.1371/journal.pone.0120773
Yeh, F. C., Badre, D., and Verstynen, T. (2016). Connectometry: a statistical approach harnessing the analytical potential of the local connectome. Neuroimage 125, 162–171. doi: 10.1016/j.neuroimage.2015.10.053
Yeh, F. C., Verstynen, T. D., Wang, Y., Fernandez-Miranda, J. C., and Tseng, W. Y. (2013). Deterministic diffusion fiber tracking improved by quantitative anisotropy. PLoS ONE 8:e80713. doi: 10.1371/journal.pone.0080713
Yeh, F. C., Wedeen, V. J., and Tseng, W. Y. (2010). Generalized q-sampling imaging. IEEE Trans. Med. Imaging 29, 1626–1635. doi: 10.1109/TMI.2010.2045126
Yeh, F. C., Wedeen, V. J., and Tseng, W. Y. (2011). Estimation of fiber orientation and spin density distribution by diffusion deconvolution. Neuroimage 55, 1054–1062. doi: 10.1016/j.neuroimage.2010.11.087
Yoon, E. J., Kim, Y. K., Shin, H. I., Lee, Y., and Kim, S. E. (2013). Cortical and white matter alterations in patients with neuropathic pain after spinal cord injury. Brain Res. 1540, 64–73. doi: 10.1016/j.brainres.2013.10.007
Yu, D., Yuan, K., Qin, W., Zhao, L., Dong, M., Liu, P., et al. (2013). Axonal loss of white matter in migraine without aura: a tract-based spatial statistics study. Cephalalgia 33, 34–42. doi: 10.1177/0333102412466964
Yuan, C., Shi, H., Pan, P., Dai, Z., Zhong, J., Ma, H., et al. (2017). Gray matter abnormalities associated with chronic back pain: a meta-analysis of voxel-based morphometric studies. Clin. J. Pain 33, 983–990. doi: 10.1097/AJP.0000000000000489
Keywords: analgesia - trends, anesthesia, acute pain, tractography, fractional anisotropy, white matter structure
Citation: Torrecillas-Martínez L, Catena A, O'Valle F, Solano-Galvis C, Padial-Molina M and Galindo-Moreno P (2020) On the Relationship Between White Matter Structure and Subjective Pain. Lessons From an Acute Surgical Pain Model. Front. Hum. Neurosci. 14:558703. doi: 10.3389/fnhum.2020.558703
Received: 03 May 2020; Accepted: 26 October 2020;
Published: 24 November 2020.
Edited by:
Stephen John Sawiak, University of Cambridge, United KingdomReviewed by:
Anna Carolyna Lepesteur Gianlorenco, Federal University of São Carlos, BrazilXiaoluan Xia, Taiyuan University of Technology, China
Copyright © 2020 Torrecillas-Martínez, Catena, O'Valle, Solano-Galvis, Padial-Molina and Galindo-Moreno. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Laura Torrecillas-Martínez, ltorrecillasm@gmail.com
 Laura Torrecillas-Martínez
Laura Torrecillas-Martínez Andrés Catena
Andrés Catena Francisco O'Valle
Francisco O'Valle César Solano-Galvis2
César Solano-Galvis2  Pablo Galindo-Moreno
Pablo Galindo-Moreno