Relationship between the novel and traditional anthropometric indices and subclinical atherosclerosis evaluated by carotid intima-media thickness (c-IMT)
- 1Department of Internal Medicine, Hospital Comarcal de la Axarquía, Málaga, Spain
- 2Department of Nursing, Nursing and Occupational Therapy College, University of Extremadura, Cáceres, Spain
- 3Department of Internal Medicine, Hospital San Pedro Alcántara, Cáceres, Spain
- 4Department of Internal Medicine, Hospital Virgen Del Puerto, Plasencia, Cáceres, Spain
- 5Department of Family Medicine, Hospital of Menorca, Minorca, Spain
- 6Department of Nursing, Faculty of Medicine and Health Science, University of Extremadura, Badajoz, Spain
- 7Department of Nursing, University of Évora, Evora, Portugal
- 8Department of Nursing, Comprehensive Health Research Centre (CHRC), Evora, Portugal
Introduction: Over the last few years, novel anthropometric indices have been developed as an alternative to body mass index (BMI) and other traditional anthropometric measurements to enhance the estimate of fat proportion and its relationship to a future cardiovascular event. The purpose of this study was to investigate the association of carotid intima-media thickness (c-IMT) estimated by Doppler ultrasound with current anthropometric indices (traditional and novel).
Methods: A cross-sectional study was conducted on a total of 789 Spanish patients. Traditional (BMI, WHR, and WHtR) and new (WWI, AVI, ABSI, BRI, BAI, CUN-BAE, and CI) anthropometric indices were determined, and carotid Doppler ultrasound was performed to evaluate c-IMT (≥0.90 mm).
Results: Most of the anthropometric indices analyzed were significantly higher among patients with pathological c-IMT, except for BMI, BAI, and CUN-BAE. In multiple linear regression analysis, c-IMT was positively related to ABSI, AVI, BRI, CI, and WWI but not to CUN-BAE, BAI, or traditional anthropometric indices. Similarly, in univariate analysis, all indices were associated with a c-IMT of ≥0.90 mm (p < 0.05), except BMI, BAI, and CUN-BAE; however, only ABSI (adjusted OR: 1.61; 95% CI: 1.08–2.40; p = 0.017), CI (adjusted OR: 1.73; 95% CI: 1.15–2.60; p = 0.008), and WWI (adjusted OR: 1.74; 95% CI: 1.14–2.64; p = 0.009) were significantly associated in multivariate analysis. Finally, CI, ABSI, and WWI provided the largest AUC, and BMI and CUN-BAE showed the lowest AUC.
Conclusion: ABSI, CI, and WWI were positively associated with pathological c-IMT (≥0.90 mm), independent of other confounders.
Introduction
Despite improvements in recent years, cardiovascular (CV) diseases remain to be the main cause of death worldwide (1, 2). Atherosclerotic injuries are the common cause of all of these diseases. The lesions are involved in a complex chronic degenerative process that evolves over years and occurs at the level of the arterial intimal layer, resulting in progressive asymmetric focal thickening composed of connective tissue elements, lipids, and debris (3). Detection of atherosclerosis in asymptomatic individuals using different strategies helps us to predict and thus prevent future CV events (4).
Carotid ultrasound, including carotid intima-media thickness (c-IMT) ultrasound, has been suggested as a potential technique to assist CV risk stratification, as it is a safe, low-cost, and commonly available method that directly evaluates arterial atherosclerosis (5–7). In multiple previous studies, c-IMT has been demonstrated to be associated with the incidence of CV events and CV risk factors (8–12).
On the other hand, anthropometric indices are accepted as low-cost, simple, and non-invasive methods for population screening and early identification of obesity. Body mass index (BMI), waist circumference (WC), waist-to-height ratio (WHtR), and waist-to-hip ratio (WHR) have always been the most frequently used in daily clinical practice (13). In the last few years, novel anthropometric indices have been developed as an alternative to traditional anthropometric measurements to enhance the estimation of fat content and its relationship to CV risk (14).
A body shape index (ABSI) assesses general and visceral adiposity and is better related to abdominal fat than BMI (15). The body roundness index (BRI) predicts the amount of total and regional fat and is considered a predictor of metabolic syndrome in heterogeneous populations, being superior to BMI in numerous studies (16). The body adiposity index (BAI) is derived from hip circumference and height to calculate the amount of corporal adiposity (17). The Clínica Universidad de Navarra-Body Adiposity Estimator (CUN-BAE) equation is an estimator of the fat content with age, sex, and BMI and has been proven to be useful for selecting patients at high metabolic risk (18). The abdominal volume index (AVI) measures the volume of abdominal fat volume and presents a positive association with metabolic syndrome (19). The weight-adjusted waist index (WWI) has shown an association with CV morbidity and mortality (20). The conicity index (CI) uses weight, height, and abdominal circumference variables to estimate the degree of obesity and fat distribution (21).
Each of the novel anthropometric measures has been related to CV risk factors, though more investigation is needed to establish their precision and accuracy (14). The present study aimed to evaluate the possible association between novel and traditional anthropometric measures and subclinical carotid atherosclerosis assessed by c-IMT measured with Doppler ultrasound.
Methodology
Study population and design
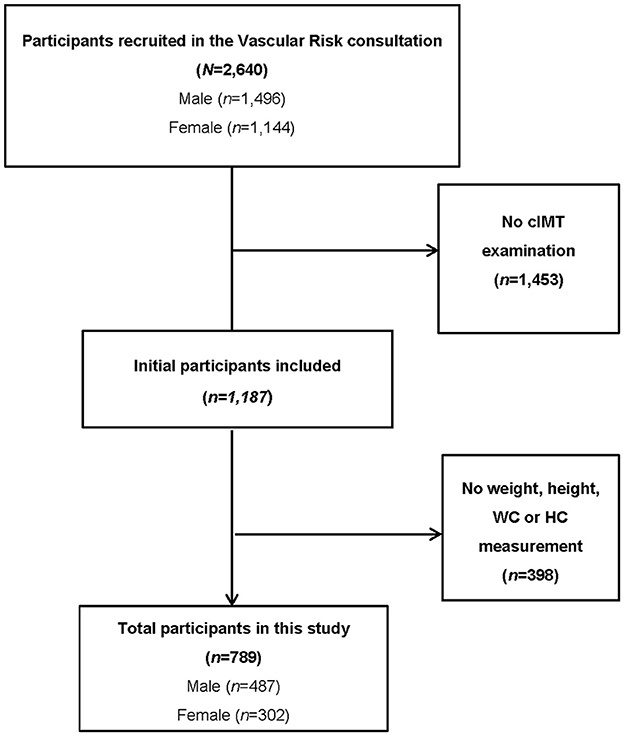
A cross-sectional study was carried out between June 2021 and September 2022, involving 789 subjects who consecutively attended the Vascular Risk consultation of the Grupo de Estudios de Enfermedades VASculares (GEEVAS) research group of Cáceres (Spain). The participant selection process is shown in Figure 1. Initially, 2,640 subjects were screened (of whom, 1,453 were excluded due to failure to complete the c-IMT assessment). A total of 1,187 participants were recruited, although 398 were excluded because no anthropometric measurement was performed. Finally, 789 patients aged between 18 and 80 were studied. Participants with anatomical disorders that made cervical examination difficult, institutionalized patients, chronic kidney disease in dialysis replacement treatment patients, pregnant women, mentally ill or incapacitated patients, and those who had been diagnosed with terminal diseases were excluded. Each participant gave written informed consent to participate in the study. The study protocol was in accordance with the Declaration of Helsinki and was previously approved by the Ethics Committee (Ref. 047-2021) of the University Hospital “San Pedro de Alcántara” of Cáceres (Spain).
Study variables
Clinical variables associated with CV risk (age, smoking status, sedentary lifestyle, presence of dyslipidemia, hypertension, diabetes mellitus, metabolic syndrome, and obesity), current medical treatment, and previous CV events were extracted from the patient's medical history. After a period longer than 10 h of fasting, a blood test was performed including coagulation, biochemistry with hepatic and renal function, a complete blood count, and glycaemic and lipid profiling.
Each subject completed the physical assessment. Blood pressure (BP) readings were taken in the first hour in the morning with the patient relaxed and seated in accordance with the latest recommendations of the European Society of Hypertension (22). A total of three measurements of systolic (SBP) and diastolic blood pressure (DBP) were performed, and their values were estimated as the average values of the last two readings taken with an oscillometric device (OMRON model HEM-907). Consequently, pulse pressure (PP) was determined: PP = SBP-DBP.
Weight was measured with a precision biomedical scale and the height was determined with a Harpenden stadiometer. Both measures were carried out with participants wearing light clothing and no shoes. A non-elastic tape was used to assess the hip circumference (HC) and WC following the Spanish Society for the Study of Obesity recommendations (23). Novel and traditional anthropometric indices were calculated using the formulas shown in Table 1.
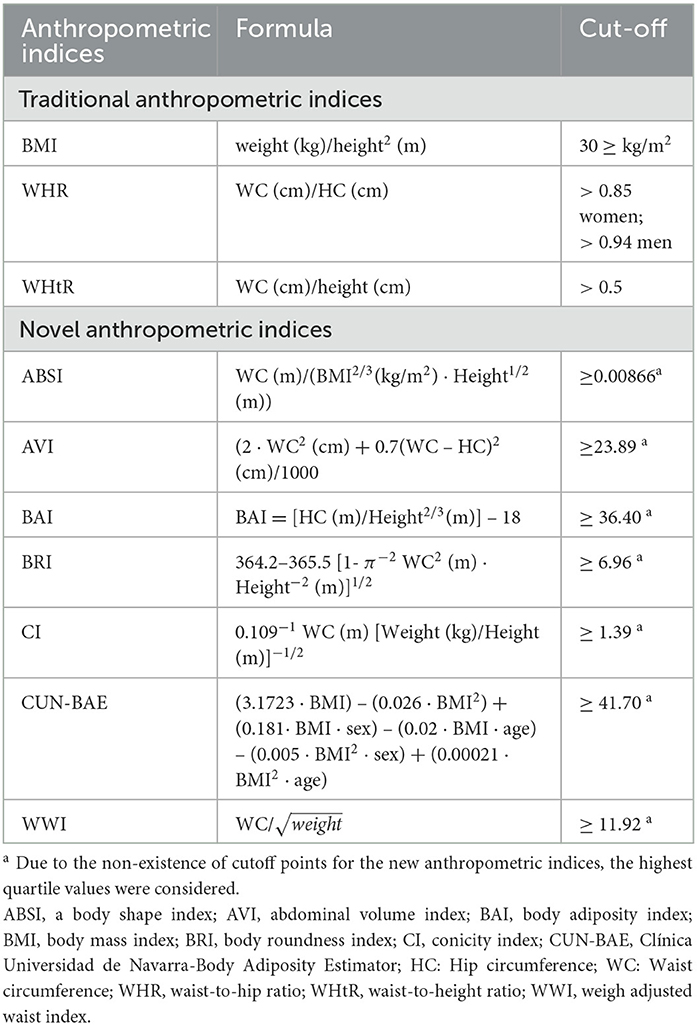
Table 1. Formulas to calculate traditional and novel anthropometric indices and cut-off considered in this study.
Carotid ultrasonography assessment (c-IMT)
Carotid ultrasonography was carried out according to the Mannheim Consensus recommendations (24) by a single well-trained operator. A LOGIQ S7® ultrasound device (General Electric Healthcare, United Kingdom) with an 8-MHz linear probe was used. The c-IMT was determined automatically with the specific software included in the ultrasound device. All the measurement was performed with the patient in the supine position, the head lightly rotated away from the carotid artery was assessed, and the neck hyperextended. A mean c-IMT of ≥0.90 mm was considered pathological (carotid subclinical atherosclerosis) (25).
Statistical analysis
Categorical variables are presented as frequencies (%) and continuous variables are presented as the averages ± standard deviations (sd). Subjects were compared according to the presence or absence of pathological c-IMT. The distribution was considered normal when a p > 0.05 was found in the Kolmogorov–Smirnov test. Categorical variables were compared utilizing the χ2 test or Fisher's exact test when in any of the groups, the observed frequency was <5. Moreover, the Student's t-test (if normal distribution) or the Mann–Whitney U-test (if non-normal distribution) was used to compare continuous variables. Pearson's correlations were utilized to investigate the relation between c-IMT and the novel and traditional anthropometric measures. Multiple linear regression applying the enter method was employed to assess whether the studied variables were predictive of mean c-IMT.
In addition, uni- and multivariate logistic regression analyses were carried out to assess the association between dependent (pathological c-IMT) and independent variables. Due to the lack of cutoff points for the novel anthropometric measures, the values of the greatest quartile were considered while for traditional anthropometric measures, previously published pathological cutoff points were assumed. Table 1 shows the pathological cutoff used in this study. Odds ratios (ORs) and subsequent 95% confidence intervals (CIs) were analyzed. When the independent variables had a p < 0.10 in the univariate analysis, they were incorporated into the multivariate analysis.
Finally, the predictive performance of anthropometric indices for identifying carotid subclinical atherosclerosis (c-IMT ≥ 0.90 mm) was analyzed by receiver operating characteristic (ROC) analysis. The optimal cutoff values of anthropometric indices to detect pathological c-IMT (≥0.90 mm) from ROC analyses were determined by the maximum Youden's index (sensitivity + specificity −1).
Statistical analysis was carried out using IBM SPSS V.27 software (IBM Corporation, Armonk, NY, USA).
Results
A total of 789 (61.8% men) patients with an average age of 64.14 ± 12.20 years were analyzed. Of these, 195 had a c-IMT of ≥ 0.90 mm. The variables were compared between patients with non-pathological c-IMT (<0.90 mm) and patients with pathological c-IMT (≥ 0.90 mm) (Table 2). Significant differences were observed in favor of subjects with a c-IMT ≥ 0.90 mm in terms of age, male sex, diabetes, hypertension, metabolic syndrome, and CV events. Smoking, dyslipidemia, obesity, and a sedentary lifestyle were not significant. Patients with pathological c-IMT (≥ 0.90 mm) had significantly higher values of systolic and diastolic blood pressure, pulse pressure, fast plasma glucose, glycated hemoglobin, and creatine clearance. The use of antidiabetic and antihypertensive treatments was significantly greater. However, values of total cholesterol and low-density lipoprotein cholesterol were significantly lower in patients with c-IMT≥ 0.90 mm. With respect to the anthropometric indices analyzed, the ABSI, AVI, BRI, WWI, WHR, and WHtR were significantly higher among patients with pathological c-IMT (≥ 0.90 mm). However, non-significant differences were found with respect to BMI, BAI, and CUN-BAE.
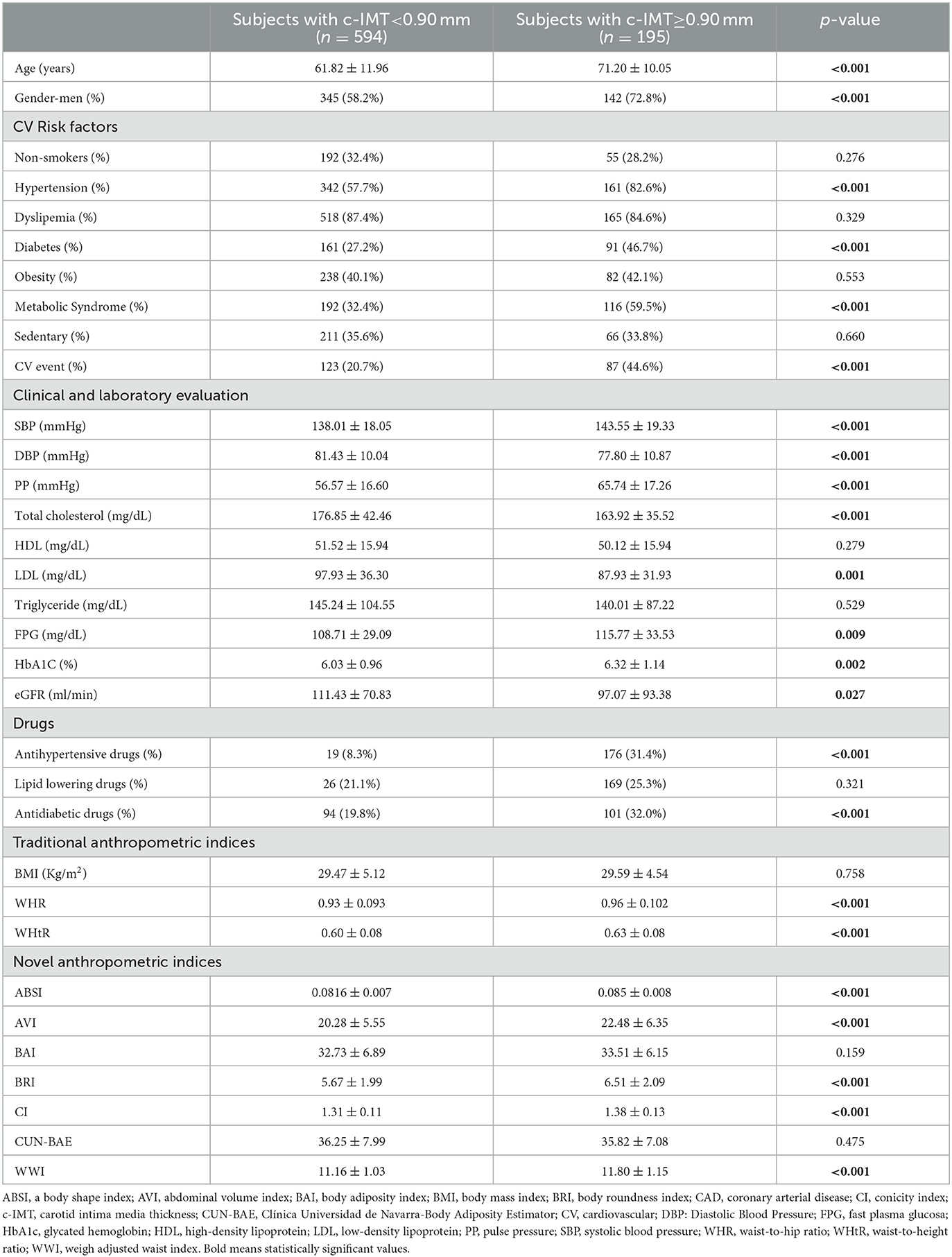
Table 2. Baseline characteristics among patients according to the presence of pathological c-IMT (≥0.90 mm).
On the other hand, c-IMT was significantly correlated with all anthropometric indices studied, except for CUN-BAE (Table 3). We further investigated the possible significant relationship of c-IMT with the anthropometric indices studied by multiple linear regression. This analysis was adjusted for confounding variables. C-IMT was positively related (p < 0.05) to ABSI, AVI, BRI, CI, and WWI but not to CUN-BAE, BAI, or the traditional anthropometric indices.
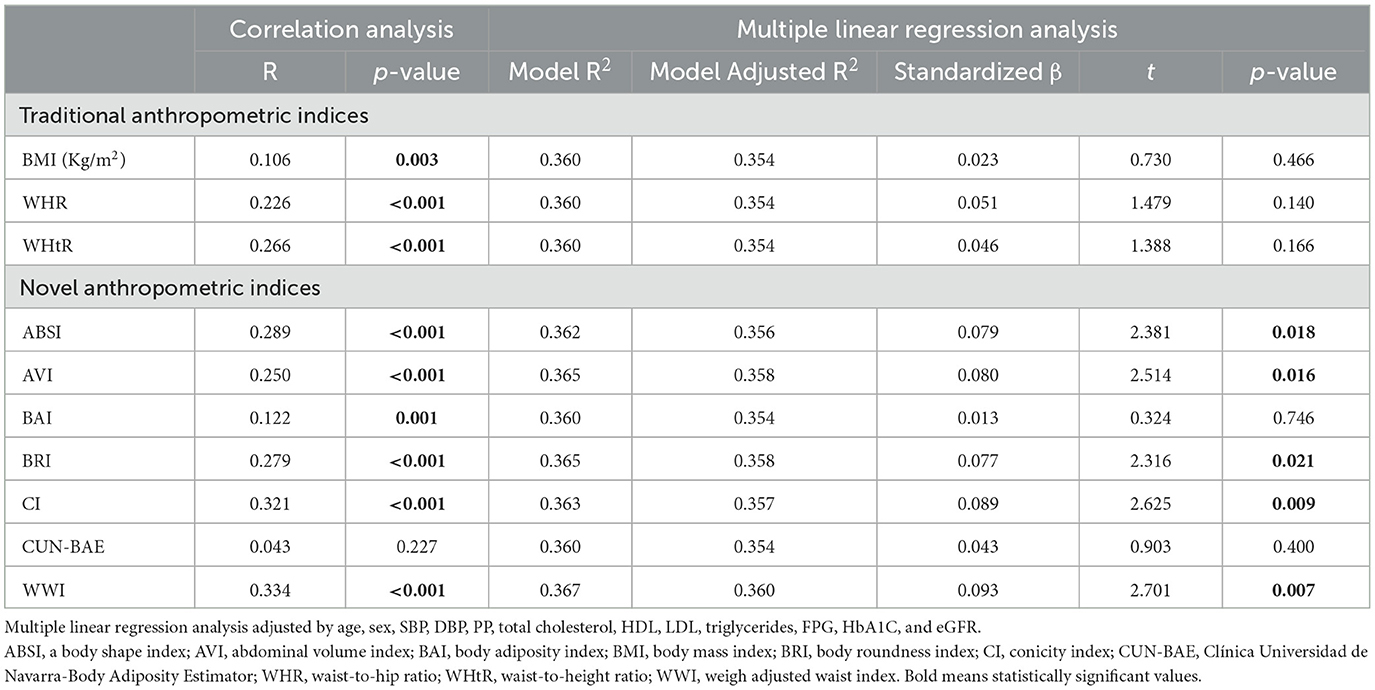
Table 3. Correlation and multiple linear regression analysis between c-IMT and anthropometric indices.
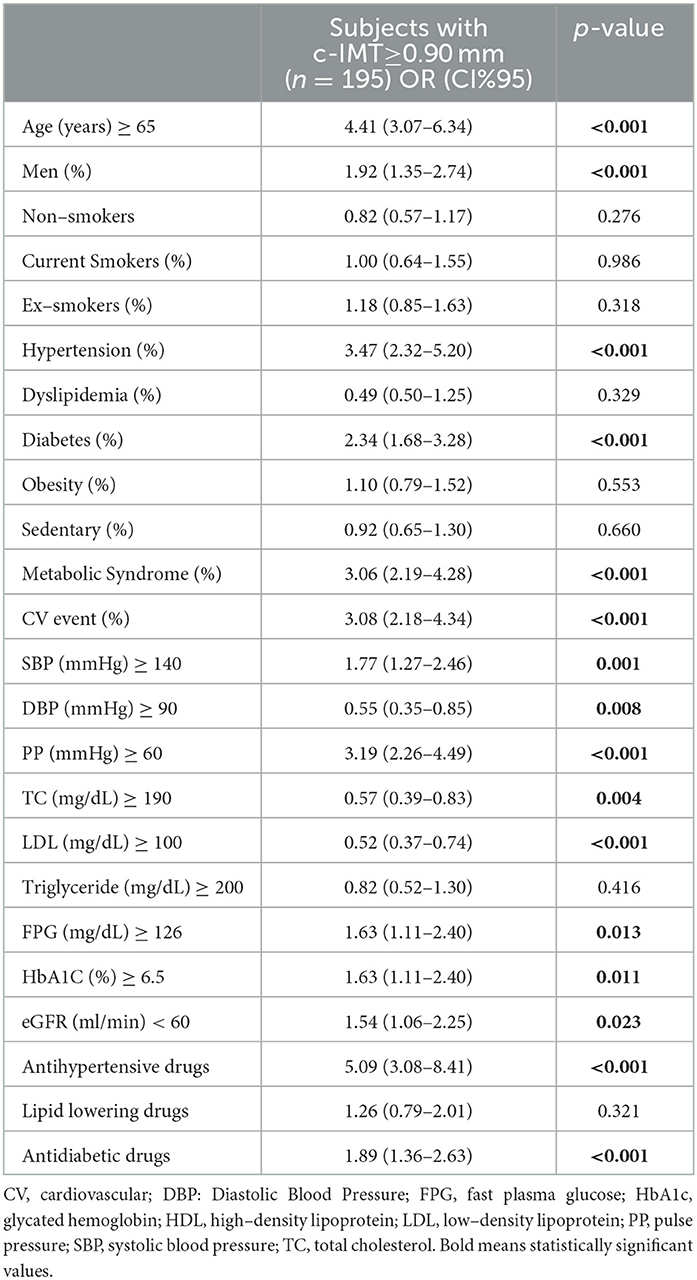
In the univariate analysis (Table 4), the variables that were significantly associated with a c-IMT ≥ 0.90 mm were male sex, age ≥ 65 years, diabetes, hypertension, metabolic syndrome, cardiovascular event, eGFR < 60 ml/min, FPG ≥ 126 mg/dL, HbA1C ≥ 6.5%, TC ≥ 190 mg/dL, LDL ≥ 100 mg/dL, SBP ≥140 mmHg, DBP ≥ 90 mmHg, and PP ≥ 60 mmHg.
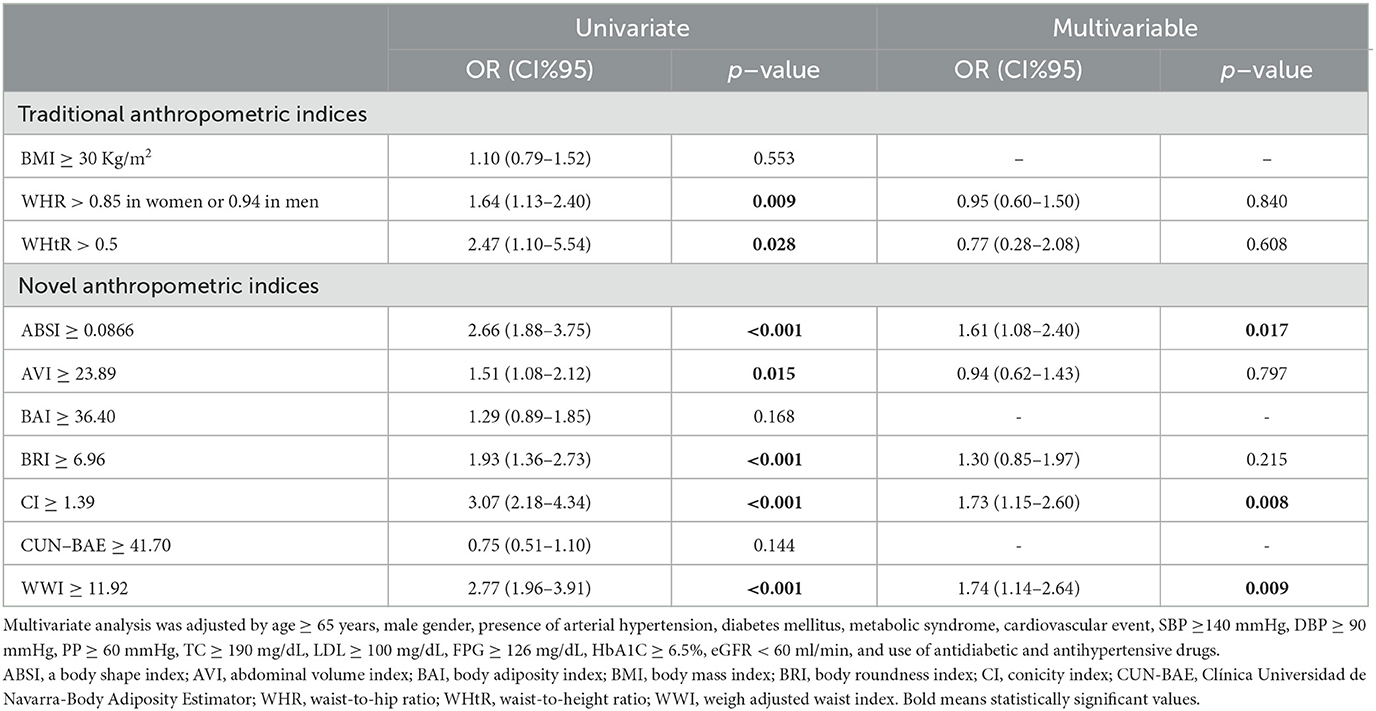
In the univariate analysis of anthropometric indices (Table 5), WHR (OR: 1.64; 95% CI: 1.13–2.40; p = 0.009), WHtR (OR: 2.47; 95% CI: 1.10–5.54; p = 0.028), ABSI (OR: 2.66; 95% CI: 1.88–3.75; p < 0.001), AVI (OR: 1.51; 95% CI: 1.08–2.12; p = 0.015), BRI (OR: 1.93; 95% CI: 1.36–2.73; p < 0.001), CI (OR: 3.07; 95% CI: 2.18–4.34; p < 0.001), and WWI (OR: 2.77; 95% CI: 1.96–3.91; p < 0.001) presented a significantly positive association with a c–IMT of ≥ 0.90 mm. However, only ABSI (adjusted OR: 1.61; 95% CI: 1.08–2.40; p = 0.017), CI (adjusted OR: 1.73; 95% CI: 1.15–2.60; p = 0.008), and WWI (adjusted OR: 1.74; 95% CI: 1.14–2.64; p = 0.009) were significant in the multivariate analysis.
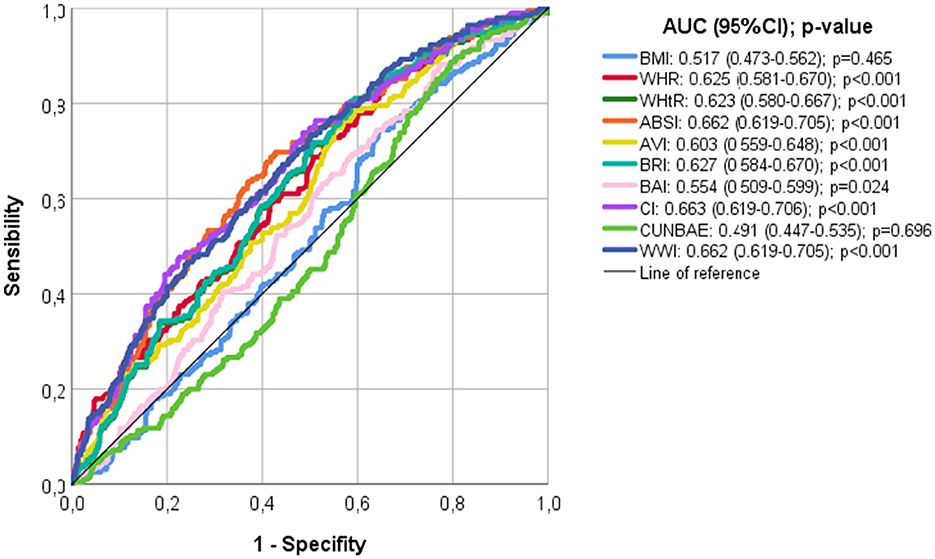
Finally, according to the ROC analyses (Figure 2), CI, ABSI, and WWI showed the largest area under the curve (AUC: 0.663, 0.662, and 0.663, respectively), and BMI and CUN-BAE showed the smallest AUC (0.491 and 0.517, respectively). The optimal cut-off values to detect pathological c-IMT (>0.9 mm) from ROC analyses were 0.0824 for ABSI, 1.31 for CI, and 11.07 for WWI.
Discussion
In this cross-sectional study that included 789 Spanish subjects, ABSI, CI, and WWI were significantly associated with subclinical carotid atherosclerosis assessed by c-IMT measured with Doppler ultrasound after multivariate adjustment.
In multiple previous studies, increased c-IMT has been associated with CV risk factors and the occurrence of CV events (9–11). Furthermore, increased c-IMT has been associated with atherosclerosis in different arterial beds, involvement of other systemic organs (11), and prediction of future CV events (4). Similarly, the carotid plaque has been demonstrated to be related to CV risk factors (26) and outperform c-IMT in predicting myocardial infarction (5), being a good prognostic marker of future CV events (27). In the latest 2019 European Society of Cardiology and European Atherosclerosis Society guidelines for the management of dyslipidemias (28), assessment of carotid atherosclerotic burden by ultrasound has a predictive value for CV events comparable to that of coronary calcium measurement by computed tomography (29–31); in contrast, c-IMT measurement is inferior to carotid plaque detection (32, 33).
Some studies support that c-IMT and carotid plaque represent different phases of atherogenesis, such that the progressive increase in c-IMT (wall growth) would be a state before the development of carotid plaque (34–37). According to this theory, c-IMT would be a predictor of the formation of new plaques and would highlight its importance as a tool for detecting individuals at high risk for future CVD in its early stages. On the other hand, other studies argue that c-IMT and carotid plaque represent two different phases of vascular remodeling (38, 39), supported by genetic studies that have revealed the existence of different genes associated with c-IMT and carotid plaque (40, 41).
Following this controversy, a meta-analysis was performed in 2019 of seven cohort studies including a total of 9,341 subjects who showed a significant relationship between the occurrence of first carotid plaque and increased baseline c-IMT, although this would not necessarily involve a direct association between the two. There is a possibility that the considerable number of risk factors they share may have played a role, despite multivariate adjustment (7). It is clear that both measurements have been shown to be associated with CV risk factors and with the incidence of CV events, with the union of both measures being a better predictor of future CV events than separately (5, 42, 43).
On the other hand, obesity, which is considered a public health problem, is a chronic disease linked with an increased risk of CV disease and all-cause mortality (44–46). Currently, scientific societies recommend BMI and WC as indicators of obesity (13, 47, 48). However, these measures have several limitations, as they neither discriminate between fat and muscle mass nor do they take into account fat distribution, which is one of the main predictors of metabolic disease risk (18, 49). In recent years, new anthropometric indices have emerged with the aim of improving the estimation of fat proportion and its relation with CV risk (14).
In our study, all anthropometric indices, except BMI, CUN-BAE, and BAI, showed an association with pathological c-IMT in the univariate analysis, but only ABSI, CI, and WWI did so after accounting for confounders in the multivariate analysis. Recently, our research group has published the relationship between subclinical atherosclerosis in this study population assessed by the presence of carotid plaques, with the new and traditional anthropometric indices, finding that only the ABSI independently showed an association with subclinical atherosclerosis (50).
The ABSI is a good estimator of central obesity and visceral adiposity (15) and is considered a non-invasive and simple tool, which can be easily applied to daily clinical practice. A significant association between ABSI and c-IMT has been shown in two previous studies (51). This relationship has also been observed between ABSI and the presence of carotid plaque (52). Similarly, this new anthropometric index has been related to an increase in diabetes mellitus, hypertension, and CV disease, outperforming WC and BMI in predicting CV and all-cause mortality (53, 54).
The CI hypnotized that subjects with less fat around the abdomen have a cylinder shape while those with more fat accumulation in the central area have a double-cone shape and was proposed as a predictor of corporal fat distribution and obesity (19, 21). Its value increases as a function of fat accumulation in the abdominal region of the body. In previous studies, the CI has been positively associated with insulin resistance, diabetes, hypertension, and dyslipidemia, although with exclusively older adult samples and divided by sex (55, 56). However, in a previous study, this anthropometric index was not associated with c-IMT (57). No other articles have studied this association.
In 2018, Park et al. suggested WWI as a novel simple anthropometric index of obesity to assess adiposity by standardizing WC by weight, showing a significant relationship with both CV mortality and morbidity (20). In contrast to BMI and WC, fat and muscle mass components could be better reflected (58). In subsequent studies, WWI has been shown to be a superior predictor of hypertension than WC and BMI and has been related to increased risk of diabetes (59, 60). In a prospective study with a cohort of 12,000 patients conducted earlier this year in southern China, higher levels of WWI were associated with an increased risk of CV and all-cause mortality (61). This is the first study to investigate the relationship between WWI and c-IMT.
In this study, ABSI, CI, and WWI were the anthropometric indices that were independently associated with pathological c-IMT (≥0.90 mm). These anthropometric indices have in common the result of adjusting WC for weight or BMI, being better indicators of central obesity and visceral adiposity than traditional anthropometric indices (14). Visceral adiposity is known to secrete vasoactive compounds that act as inflammatory mediators, such as protein C reactive or adipokines (e.g., interleukin-6, leptin, and TNF-α), possibly inducing changes in arterial structure and function (62–65), which may explain our findings. Inflammation plays an important role in all phases of atherosclerosis, including the initial activation of endothelial cells, progression, and, ultimately, its final complication of thrombosis (66).
Currently, there are no studies that provide the optimal cut-off values of novel anthropometric indices to detect pathological c-IMT (≥0.90 mm), so this study is the first to report such values.
This cross-sectional study has various limitations. First, this was an observational study; consequently, our results only suggest association and not cause–effect. Furthermore, all the individuals enrolled were from our province; therefore, the findings may not be appropriate for populations from other regions. On the other hand, most of the participants had a moderate or high risk of CV disease, and our results may not be applicable to lower-risk populations. Finally, age was statistically different between the two groups, and it is known that increasing the age also increases the cardiovascular risk in normoponderal subjects.
In conclusion, the results of our study, associated with the previous literature, indicate that the ABSI, CI, and WWI could be good predictors of subclinical atherosclerotic measured by c-IMT. Combinations of several anthropometric measures could further enhance CV risk prediction, and we suggest that its use should be implemented in daily clinical practice for the prevention and control of CV events.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author (sergiorico@unex.es).
Ethics statement
The studies involving human participants were reviewed and approved by Clinical Research and Ethics Committee (Ref. 047-2021) of Cáceres (Spain). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conceptualization and writing—original draft preparation: CC-M, JC-G, SR-M, and JFSM-T. Methodology: CC-M, CS-B, JG-G, GE-S, FR-V, and ES-M. Validation: CC-M, JC-G, and SR-M. Formal analysis and writing—review and editing: JFSM-T and SR-M. Investigation: CC-M, JC-G, CS-B, JG-G, GE-S, FR-V, CF, and ES-M. Data curation: SR-M. Supervision: SR-M, JC-G, and JFSM-T. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by FEDER, Programa Interreg VA España-Portugal (POCTEP), Instituto Internacional de Investigação e Inovação em Envelhecimento–Capitaliza. 0786_CAP4ie_4_P.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke statistics-2022 update: a report from the american heart association. Circulation. (2022) 145:e153–639. doi: 10.1161/CIR.0000000000001052
2. Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur Heart J. (2022) 43:716–99. doi: 10.1093/eurheartj/ehab892
3. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. (2005) 352:1685–95. doi: 10.1056/NEJMra043430
4. Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. (2007) 115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875
5. Naqvi TZ, Lee M-S. Carotid intima-media thickness and plaque in cardiovascular risk assessment. JACC Cardiovasc Imaging. (2014) 7:1025–38. doi: 10.1016/j.jcmg.2013.11.014
6. Redberg RF, Vogel RA, Criqui MH, Herrington DM, Lima JAC, Roman MJ. 34th Bethesda Conference: task force #3–what is the spectrum of current and emerging techniques for the noninvasive measurement of atherosclerosis? J Am Coll Cardiol. (2003) 41:1886–98. doi: 10.1016/S0735-1097(03)00360-7
7. Willeit P, Tschiderer L, Allara E, Reuber K, Seekircher L, Gao L, et al. Carotid intima-media thickness progression as surrogate marker for cardiovascular risk: meta-analysis of 119 clinical trials involving 100 667 patients. Circulation. (2020) 142:621–42. doi: 10.1161/CIRCULATIONAHA.120.046361
8. Polak JF, Pencina MJ, Pencina KM, O'Donnell CJ, Wolf PA, D'Agostino RB. Carotid-wall intima-media thickness and cardiovascular events. N Engl J Med. (2011) 365:213–21. doi: 10.1056/NEJMoa1012592
9. Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987-1993. Am J Epidemiol. (1997) 146:483–94. doi: 10.1093/oxfordjournals.aje.a009302
10. O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson Jr SK. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med. (1999) 340:14–22. doi: 10.1056/NEJM199901073400103
11. Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE. Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation. (1997) 96:1432–7. doi: 10.1161/01.CIR.96.5.1432
12. Sinning C, Wild PS, Echevarria FMO, Wilde S, Schnabel R, Lubos E, et al. Sex differences in early carotid atherosclerosis (from the community-based Gutenberg-Heart Study). Am J Cardiol. (2011) 107:1841–7. doi: 10.1016/j.amjcard.2011.02.318
13. Jensen MD, Ryan DH, Apovian CM, Ard JD, Comuzzie AG, Donato KA, et al. 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the obesity society. J Am Coll Cardiol. (2013) 63:2985–3023. doi: 10.1161/01.cir.0000437739.71477.ee
14. Jayawardena R, Ranasinghe P, Ranathunga T, Mathangasinghe Y, Wasalathanththri S, Hills AP. Novel anthropometric parameters to define obesity and obesity-related disease in adults: a systematic review. Nutr Rev. (2020) 78:498–513. doi: 10.1093/nutrit/nuz078
15. Krakauer NY, Krakauer JC, A. new body shape index predicts mortality hazard independently of body mass index. PLoS ONE. (2012) 7:e39504. doi: 10.1371/journal.pone.0039504
16. Rico-Martín S, Calderón-García JF, Sánchez-Rey P, Franco-Antonio C, Martínez Alvarez M, Sánchez Muñoz-Torrero JF. Effectiveness of body roundness index in predicting metabolic syndrome: a systematic review and meta-analysis. Obes Rev. (2020) 21:e13023. doi: 10.1111/obr.13023
17. Bergman RN, Stefanovski D, Buchanan TA, Sumner AE, Reynolds JC, Sebring NG, et al. Better index of body adiposity. Obesity (Silver Spring). (2011) 19:1083–9. doi: 10.1038/oby.2011.38
18. Gómez-Ambrosi J, Silva C, Catalán V, Rodríguez A, Galofré JC, Escalada J, et al. Clinical usefulness of a new equation for estimating body fat. Diabetes Care. (2012) 35:383–8. doi: 10.2337/dc11-1334
19. Guerrero-Romero F, Rodriguez-Morán M. Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. (2003) 34:428–32. doi: 10.1016/S0188-4409(03)00073-0
20. Park Y, Kim NH, Kwon TY, Kim SG. A novel adiposity index as an integrated predictor of cardiometabolic disease morbidity and mortality. Sci Rep. (2018) 8:16753. doi: 10.1038/s41598-018-35073-4
21. Valdez R. A simple model-based index of abdominal adiposity. J Clin Epidemiol. (1991) 44:955–6. doi: 10.1016/0895-4356(91)90059-I
22. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 Practice guidelines for the management of arterial hypertension of the european society of hypertension and the european society of cardiology: ESH/ESC task force for the management of arterial hypertension. J Hypertens. (2018) 36:2284–309. doi: 10.1097/HJH.0000000000001961
23. Salas-Salvadó J, Rubio MA, Barbany M, Moreno B, Grupo Colaborativo de la SEEDO. SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria. Med Clin (Barc). (2007) 128:184–96. doi: 10.1016/S0025-7753(07)72531-9
24. Touboul P-J, Hennerici MG, Meairs S, Adams H, Amarenco P, Bornstein N, et al. Mannheim carotid intima-media thickness and plaque consensus (2004-2006-2011). An update on behalf of the advisory board of the 3rd, 4th and 5th watching the risk symposia, at the 13th, 15th and 20th European Stroke Conferences, Mannheim, Germany, 2004, Brussels, Belgium, 2006, and Hamburg, Germany, 2011. Cerebrovasc Dis. (2012) 34:290–6. doi: 10.1159/000343145
25. Vlachopoulos C, Xaplanteris P, Aboyans V, Brodmann M, Cífková R, Cosentino F, et al. The role of vascular biomarkers for primary and secondary prevention a position paper from the European Society of Cardiology Working Group on peripheral circulation: Endorsed by the Association for Research into Arterial Structure and Physiology (ARTERY) Society. Atherosclerosis. (2015) 241:507–32. doi: 10.1016/j.atherosclerosis.2015.05.007
26. Herder M, Johnsen SH, Arne A, Mathiesen EB. Risk factors for progression of carotid intima-media thickness and total plaque area: a 13-year follow-up study: the Tromsø study. Stroke. (2012) 43:1818–23. doi: 10.1161/STROKEAHA.111.646596
27. Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima-media thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis. (2011) 220:128–33. doi: 10.1016/j.atherosclerosis.2011.06.044
28. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. (2020) 41:111–88. doi: 10.1093/eurheartj/ehz455
29. Baber U, Mehran R, Sartori S, Schoos MM, Sillesen H, Muntendam P, et al. Prevalence, impact, and predictive value of detecting subclinical coronary and carotid atherosclerosis in asymptomatic adults: the BioImage study. J Am Coll Cardiol. (2015) 65:1065–74. doi: 10.1016/j.jacc.2015.01.017
30. McDermott MM, Kramer CM, Tian L, Carr J, Guralnik JM, Polonsky T, et al. Plaque composition in the proximal superficial femoral artery and peripheral artery disease events. JACC Cardiovasc Imaging. (2016) 10:1003–12. doi: 10.1016/j.jcmg.2016.08.012
31. Sillesen H, Sartori S, Sandholt B, Baber U, Mehran R, Fuster V. Carotid plaque thickness and carotid plaque burden predict future cardiovascular events in asymptomatic adult Americans. Eur Heart J Cardiovasc Imaging. (2018) 19:1042–50. doi: 10.1093/ehjci/jex239
32. Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, et al. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. (2012) 308:788–95. doi: 10.1001/jama.2012.9624
33. den Ruijter HM, Peters SAE, Anderson Todd J, Britton AR, Dekker JM, Eijkemans MJ, et al. Common carotid intima-media thickness measurements in cardiovascular risk prediction: a meta-analysis. JAMA. (2012) 308:796–803. doi: 10.1001/jama.2012.9630
34. Eigenbrodt ML, Bursac Z, Tracy RE, Mehta JL, Rose KM, Couper DJ. B-mode ultrasound common carotid artery intima-media thickness and external diameter: cross-sectional and longitudinal associations with carotid atherosclerosis in a large population sample. Cardiovasc Ultrasound. (2008) 6:10. doi: 10.1186/1476-7120-6-10
35. Xie W, Liu J, Wang W, Wang M, Li Y, Sun J, et al. Five-year change in systolic blood pressure is independently associated with carotid atherosclerosis progression: a population-based cohort study. Hypertens Res. (2014) 37:960–5. doi: 10.1038/hr.2014.93
36. Zureik M, Ducimetière P, Touboul PJ, Courbon D, Bonithon-Kopp C, Berr C, et al. Common carotid intima-media thickness predicts occurrence of carotid atherosclerotic plaques: longitudinal results from the Aging Vascular Study (EVA) study. Arterioscler Thromb Vasc Biol. (2000) 20:1622–9. doi: 10.1161/01.ATV.20.6.1622
37. Prati P, Vanuzzo D, Casaroli M, Bader G, Mos L, Pilotto L, et al. Determinants of carotid plaque occurrence A long-term prospective population study: the San Daniele Project. Cerebrovasc Dis. (2006) 22:416–22. doi: 10.1159/000094993
38. Spence JD. Measurement of intima-media thickness vs. carotid plaque: uses in patient care, genetic research and evaluation of new therapies. Int J Stroke. (2006) 1:216–21. doi: 10.1111/j.1747-4949.2006.00068.x
39. Finn A, Kolodgie FD, Virmani R. Correlation between carotid intimal/medial thickness and atherosclerosis: a point of view from pathology. Arterioscler Thromb Vasc Biol. (2009) 30:177–81. doi: 10.1161/ATVBAHA.108.173609
40. Bis JC, Kavousi M, Franceschini N, Isaacs A, Abecasis GR, Schminke U, et al. Meta-analysis of genome-wide association studies from the CHARGE consortium identifies common variants associated with carotid intima media thickness and plaque. Nat Genet. (2011) 43:940–7.
41. Franceschini N, Giambartolomei C, de Vries PS, Finan C, Bis JC, Huntley RP, et al. GWAS and colocalization analyses implicate carotid intima-media thickness and carotid plaque loci in cardiovascular outcomes. Nat Commun. (2018) 9:5141. doi: 10.1038/s41467-018-07340-5
42. Nambi V, Chambless L, Folsom AR, Max H, Hu Y, Mosley T, et al. Carotid intima-media thickness and presence or absence of plaque improves prediction of coronary heart disease risk: the ARIC (Atherosclerosis Risk In Communities) study. J Am Coll Cardiol. (2010) 55:1600–7. doi: 10.1016/j.jacc.2009.11.075
43. Nicolaides AN, Panayiotou AG, Maura G, Tyllis T, Bond D, Georgiou N, et al. Arterial ultrasound testing to predict atherosclerotic cardiovascular events. J Am Coll Cardiol. (2022) 79:1969–82. doi: 10.1016/j.jacc.2022.03.352
44. Cameron AJ, Magliano DJ, Shaw JE, Zimmet PZ, Carstensen B, Alberti KGM, et al. The influence of hip circumference on the relationship between abdominal obesity and mortality. Int J Epidemiol. (2012) 41:484–94. doi: 10.1093/ije/dyr198
45. Mottillo S, Filion KB, Genest J, Joseph L, Pilote L, Poirier P, et al. The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. (2010) 56:1113–32. doi: 10.1016/j.jacc.2010.05.034
46. Ortega FB, Sui X, Lavie CJ, Blair SN. Body mass index, the most widely used but also widely criticized index: would a criterion standard measure of total body fat be a better predictor of cardiovascular disease mortality? Mayo Clin Proc. (2016) 91:443–55. doi: 10.1016/j.mayocp.2016.01.008
47. Visseren FLJ, Mach F, Smulders YM, Carballo D, Koskinas KC, Bäck M, et al. 2021 ESC guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. (2021) 42:3227–337. doi: 10.1093/eurheartj/ehab484
48. Bray GA, Heisel WE, Afshin A, Jensen MD, Dietz WH, Long M, et al. The science of obesity management: an endocrine society scientific statement. Endocr Rev. (2018) 39:79–132. doi: 10.1210/er.2017-00253
49. Nevill AM, Stewart AD, Olds T, Holder R. Relationship between adiposity and body size reveals limitations of BMI. Am J Phys Anthropol. (2006) 129:151–6. doi: 10.1002/ajpa.20262
50. Costo-Muriel C, Calderón-Garcia JF, Rico-Martin S, Sánchez-Bacaicoa C, Escudero-Sánchez G, Galán-González J, et al. Association of subclinical carotid atherosclerosis assessed by high-resolution ultrasound with traditional and novel anthropometric indices. Curr Probl Cardiol. (2022) 48:101574. doi: 10.1016/j.cpcardiol.2022.101574
51. Gomez-Marcos MA, Gomez-Sanchez L, Patino-Alonso MC, Recio-Rodriguez JI, Gomez-Sanchez M, Rigo F, et al. A body shape index and vascular structure and function in Spanish adults (MARK study): a cross-sectional study. Medicine (Baltimore). (2018) 97:e13299. doi: 10.1097/MD.0000000000013299
52. Ma X, Chen L, Hu W, He L. Association between a body shape index and subclinical carotid atherosclerosis in population free of cardiovascular and cerebrovascular diseases. J Atheroscler Thromb. (2021) 29:1140–52. doi: 10.5551/jat.62988
53. Calderón-Garcia JF, Roncero-Martín R, Rico-Martín S, De Nicolás-Jiménez JM, López-Espuela F, Santano-Mogena E, et al. Effectiveness of body roundness index (BRI) and a body shape index (ABSI) in predicting hypertension: a systematic review and meta-analysis of observational studies. Int J Environ Res Public Health. (2021) 18:ijerph182111607. doi: 10.3390/ijerph182111607
54. Ji M, Zhang S, An R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev. (2018) 19:737–59. doi: 10.1111/obr.12666
55. Andrade MD, Freitas MCP de, Sakumoto AM, Pappiani C, Andrade SC de, Vieira VL, et al. Association of the conicity index with diabetes and hypertension in Brazilian women. Arch Endocrinol Metab. (2016) 60:436–42. doi: 10.1590/2359-3997000000187
56. Nkwana MR, Monyeki KD, Lebelo SL. Body roundness index, a body shape index, conicity index, and their association with nutritional status and cardiovascular risk factors in South African rural young adults. Int J Environ Res Public Health. (2021) 18:ijerph18010281. doi: 10.3390/ijerph18010281
57. Sánchez E, Sánchez M, Àngels B, Rius F, Torres G, Purroy F, et al. Are obesity indices useful for detecting subclinical atheromatosis in a middle-aged population? Obes Facts. (2020) 13:29–39. doi: 10.1159/000502696
58. Kim NH, Park Y, Kim NH, Kim SG. Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults. Age Ageing. (2021) 50:780–6. doi: 10.1093/ageing/afaa208
59. Li Q, Qie R, Qin P, Zhang D, Guo C, Zhou Q, et al. Association of weight-adjusted-waist index with incident hypertension: the rural Chinese cohort study. Nutr Metab Cardiovasc Dis. (2020) 30:1732–41. doi: 10.1016/j.numecd.2020.05.033
60. Liu Y, Liu X, Zhang S, Qibo Z, Fu X, Chen H, et al. Association of anthropometric indices with the development of diabetes among hypertensive patients in china: a cohort study. Front Endocrinol (Lausanne). (2021) 12:736077. doi: 10.3389/fendo.2021.736077
61. Ding C, Shi Y, Li J, Li M, Hu L, Rao J, et al. Association of weight-adjusted-waist index with all-cause and cardiovascular mortality in China: a prospective cohort study. Nutr Metab Cardiovasc Dis. (2022) 32:1210–7. doi: 10.1016/j.numecd.2022.01.033
62. Singhal A, Farooqi IS, Cole TJ, O'Rahilly S, Fewtrell M, Kattenhorn M, et al. Influence of leptin on arterial distensibility: a novel link between obesity and cardiovascular disease? Circulation. (2002) 106:1919–24. doi: 10.1161/01.CIR.0000033219.24717.52
63. Rocha VZ, Libby P. The multiple facets of the fat tissue. Thyroid. (2008) 18:175–83. doi: 10.1089/thy.2007.0296
64. Kim K, Valentine RJ, Shin Y, Gong K. Associations of visceral adiposity and exercise participation with C-reactive protein, insulin resistance, and endothelial dysfunction in Korean healthy adults. Metabolism. (2008) 57:1181–9. doi: 10.1016/j.metabol.2008.04.009
65. Tsuriya D, Morita H, Morioka T, Takahashi N, Ito T, Oki Y, et al. Significant correlation between visceral adiposity and high-sensitivity C-reactive protein (hs-CRP) in Japanese subjects. Intern Med. (2011) 50:2767–73. doi: 10.2169/internalmedicine.50.5908
Keywords: anthropometric indices, carotid intima-media thickness, cardiovascular risk factors, subclinical atherosclerosis, carotid ultrasonography
Citation: Costo-Muriel C, Calderón-García JF, Rico-Martín S, Galán-González J, Escudero-Sánchez G, Sánchez-Bacaicoa C, Rodríguez-Velasco FJ, Santano-Mogena E, Fonseca C and Muñoz-Torrero JFS (2023) Relationship between the novel and traditional anthropometric indices and subclinical atherosclerosis evaluated by carotid intima-media thickness (c-IMT). Front. Nutr. 10:1170450. doi: 10.3389/fnut.2023.1170450
Received: 14 March 2023; Accepted: 12 June 2023;
Published: 30 June 2023.
Edited by:
Michael Schmidt, Sovaris Aerospace, LLC, United StatesReviewed by:
Naoko Nakanishi, Kyoto Prefectural University of Medicine, JapanRamona Stroescu, Victor Babes University of Medicine and Pharmacy, Romania
Copyright © 2023 Costo-Muriel, Calderón-García, Rico-Martín, Galán-González, Escudero-Sánchez, Sánchez-Bacaicoa, Rodríguez-Velasco, Santano-Mogena, Fonseca and Muñoz-Torrero. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sergio Rico-Martín, sergiorico@unex.es
†These authors have contributed equally to this work
 Clara Costo-Muriel1†
Clara Costo-Muriel1†  Sergio Rico-Martín
Sergio Rico-Martín Javier Galán-González
Javier Galán-González Francisco J. Rodríguez-Velasco
Francisco J. Rodríguez-Velasco César Fonseca
César Fonseca