- School of Pharmacy, South-Central University for Nationalities, Wuhan, China
Aims: This review aims to compare the use of herbal medicine used to treat women’s menstruation and the prevalence of menstrual diseases in different regions, which reveal the use of herbal medicine globally and provide scientific guidance for improving women’s health.
Materials and Methods: The information available on herbal medicines for women between the years 2000 and 2021 was systematically collected via the library and electronic search systems such as Google Scholar, PubMed, ScienceDirect, and Web of Science as well as secondary resources including books and conference proceedings.
Results: Totally, 571 ethnic medicines commonly used for women’s menstruation health in Asia, Europe, Oceania, Africa, and America were accounted. Zingiber officinale Roscoe (Ginger), Ruta graveolens L. (Common rue), Angelica sinensis (Oliv.) Diels (Angelica sinensis), Foeniculum vulgare Mill (Fennel), Catharanthus roseus (L.) G. Don (Catharanthus roseus) and other medicines which have obvious advantages and long-term usage are utilized in the treatment of menstrual diseases. Family Asteraceae, Lamiaceae, Apiaceae, Fabaceae, and Zingiberaceae are the most common medicinal plant families used for such treatments. In many instances, the application of fresh parts of plants was observed because of the healers’ belief regarding the higher efficiency of the medicine made from fresh plants. Edible plants are used in a wide range of countries.
Conclusion: Women’s menstruation health is directly related to their health condition. Traditional medicines of most ethnic groups have contributed to women’s health care and treatment of gynecological diseases. Practitioners in this field have gained elaborate experience in treatments and medication, and assembled a large number of effective drugs and prescriptions. These experiences have also been inherited and developed by modern clinical application and scientific research. However, the basic research on these drugs is not sufficient, the knowledge of drug use has not been fully popularized, the advantages of drugs have not been fully utilized, and the guiding potential to modern drug research continues to be insufficient. As such, it is necessary to further promote and make a significant contribution to women’s health.
1 Introduction
Herbal medicine has been widely used by women globally and increasingly more have shown the necessity of herbal medicines, both in treating diseases and maintaining health (Homaie Rad et al., 2021; Morehead and McInnis, 2021). Even in the modern world, there continue to be several health issues among women that cannot be cured using modern medicine; and in some regions having no modern medicines, it continues to be necessary to use herbal medicine as an alternative or supplement for women’s health and facilitate their life (Peltzer, 2009).
The menstrual pattern of a woman is indicative of her health status. Generally, menstruation occurs in regular intervals. Menstrual diseases (MD) include premenstrual syndrome (PMS), dysmenorrhea, amenorrhea, and menstrual disorders (MDs) (Kim, 2019). Ethnographic and epidemiological studies demonstrating significant variations in symptoms experienced by women with MDs living in different locales suggest that the expression of this biological event is mediated by many factors, including diet, lifestyle, cultural expectations and behaviors, and individual constitutions (Omani Samani et al., 2018). Hormonal therapy is the main treatment for MDs in modern medicine. However, considering the side effects of modern medicine, there are increasingly and more women who prefer to rely on herbal treatment based on their own traditional/national medicine.
Herbal medicines for women’s menstruation issues are used globally, and their efficacy and safety have been mentioned in previous reviews (Maleki-Saghooni et al., 2018). However, there continues to be a lack of references on the general character and differences for the administration of herbal medicine used by women all around the world. Therefore, this review aims to provide an overall blueprint on this theme by researching primary literature by gathering 130 families and 571 species of plants used by women from 22 countries and regions. The plants were categorized into four based on the types of diseases they treat. To the best of our knowledge, this is the first attempt to compile the list of herbal medicines used for women’s menstruation issues globally.
2 Methodology
2.1 Literature Search on Medicinal Plants for Menstrual Morbidity
We retrieved peer-reviewed scientific articles that documented traditional plant use in the study area related to MD. We followed the categories of menstrual morbidity defined by Harlow and Campbell (2004) and the definition of premenstrual syndrome (PMS) (Gnanasambanthan and Datta, 2019), and classified medicinal plants in four categories: 1) premenstrual syndrome; 2) dysmenorrhea; 3) amenorrhea; 4) menstrual disorders, including irregular cycles, such as a long duration of menstrual flow and excessive, heavy bleeding, (menorrhagia/polymenorrhagia) or delayed, infrequent menses (oligomenorrhea).
Literature reviews were performed during April-May 2021, using Google Scholar, PubMed, ScienceDirect, Web of Science and the keywords “menstruation,” “amenorrhea,” “arrested menstruation,” “obstructed menses,” “emmenagogue,” “dysmenorrhea,” “menses pain,” “menstrual pain,” “menstrual cramps,” “menstrual colic,” “excessive menses,” “excessive menstruation,” “menorrhagia,” “hypomenorrhea,” “oligomenorrhea,” “scanty menses,” “premenstrual syndrome,” “menstrual disorders,” “menses disturbance,” “abnormal menstruation,” “irregular menses” and “metrorrhagia” in combination with “herbs,” “medicinal plants” and “Africa,” “Asia,” “Latin America,” “Oceania,” “Europe” or specific countries in these geographical areas. Additional literature was found in reference lists of collected publications (snowball method). To limit the data to accessible digitized literature, we focused mostly on English literature published from 1980 onwards. Plant use information without a clear definition of the use, i.e., broad descriptions like “gynecological diseases” or “women’s health,” was not included in our review. Our geographical scope was restricted to countries or regions with detailed usage documents of medicinal plants. Our geographical review aimed to spread geographical coverage as much as possible over the continent, and used the most representative papers on this subject for each country/region (preferably the papers published in peer-reviewed journal and citing substantial ethnobotanical practices regarding our subject). The literatures cited in this article are evaluated according to the requirements of “the four pillars of best practice in ethnopharmacology (www.frontiersin.org/files/pdf/4_pillars_FULL_TEXT.pdf)”.
2.2 Methods of Screening Shortlisted Species
Relevant plants from the selected papers were entered in separate excel files for each of the five continents. Columns contained the four usage categories and rows represented the species. Individual cells contained the number of papers in which a particular use category for a particular species was reported. Scientific and author names were validated by the Plant List (http://www.theplantlist.org), and synonyms were merged. The most salient plants were defined as those most frequently cited in the literature (number of papers citing this species) and those mentioned for the most use categories. When describing the different countries and regions alphabetical order was applied in this paper, and Tables involving less than 20 kinds of medicinal plants are placed in the text, and tables involving more than 20 kinds of medicinal plants are provided as Supplementary Material.
3 Results
3.1 Ethnic Herbal Medicine Used for Premenstrual Syndrome
PMS is defined as a condition with emotional, physical, and behavioral symptoms that increase in severity during the luteal phase of the menstrual cycle and resolve by the end of menstruation. By definition, there must be a symptom-free interval after menstruation and before ovulation. Generally, symptoms are observed up to 14 days before the start of menses, causing impairment of life, with anger and irritability being the most severe and long lasting symptoms. The exact cause of PMS is unknown (Gnanasambanthan and Datta, 2019). However, studies have shown that 3–8% of menstruating women are affected by PMS and that 15–20% of women meet the criteria for subclinical PMS (O’Brien et al., 2011). A review reported incidences of PMS globally are 40, 85, 46, and 60% for Europe, Africa, Asia, and South America, respectively (Direkvand Moghadam et al., 2013).
The management of PMS is generally performed in a step-wise manner from non-pharmacological strategies, antidepressant medications, and hormonal strategies, with surgical options being considered as a last resort (Walsh et al., 2015). Studies have shown a more sustained but less rapid improvement with the use of selective serotonin reuptake inhibitors (SSRIs). Vitamin B6 is also well-known as the first-line treatment for PMS (Kashanian et al., 2007). However, peripheral neuropathy of pyridoxine is characterized at doses greater than 200 mg/day (Vrolijk et al., 2017). Therefore, herbs with lower costs, better benefits, and lesser side effects have become complementary and alternative treatments for women to improve PMS.
As a concept, PMS was put forward by western medicine doctors 70 years ago, and only a handful of herbal medicines are recorded in Western countries for the treatment (Gnanasambanthan and Datta, 2019). In Western countries, anti-depressive drugs, hormonal treatment, and analgesics dominate the treatment of PMS; and plant extracts such as Vitex agnus-castus L. is commonly considered as an alternative therapy in English-speaking countries (Weisz and Knaapen, 2009).
In China, the use of Chinese herbal medicine (CHM) is very common in the treatment of PMS. Liver qi stagnation and Yin Blood deficiency are proposed as the most common root causes of PMS, and the fundamental treatment principles for PMS involve measures to regulate Liver qi to resolve stagnation and tone blood (Chou and Morse, 2005). The most common medicines for the relief of PMS are Chaihu (Bupleurum chinense DC.), Xiangfu (Cyperus rotundus L.), Danggui (Angelica sinensis (Oliv.) Diels), Baishao (Paeonia lactiflora Pall.), and formulas such as Xiaoyao Powder and Jiawei Xiaoyao Powder (JXP). In Taiwan, JXP-centered CHM combinations were most commonly prescribed for PMS. The top 10 most commonly used single herbs for PMS are Cyperus rotundus L., Leonurus japonicus Houtt. (Oriental motherwort), Corydalis yanhusuo (Y. H. Chou and Chun C. Hsu) W. T. Wang ex Z. Y. Su and C. Y. Wu, Salvia miltiorrhiza Bge., Eucommia ulmoides Oliv., Scutellaria baicalensis Georgi, Dipsacus asperoides C. Y. Cheng at T. M. Ai, Cuscuta chinensis Lam. or Cuscuta japonica Choisy, Pueraria lobata (Willd.) Ohwi, Paeonia × suffruticosa Andrews. The top five most commonly used herbal formulas for the treatment of PMS are JXP, Danggui Shaoyao Powder, Guizhi Fuling Pills, Wenjing Decoction, and Shaofu Zhuyu Decoction (Chen et al., 2014). The ingredients of these Chinese herbal formulas are listed in Table 1.
In Iran, Salvia officinalis L. extract appears to be more effective in reducing the physical and psychological symptoms associated with PMS, when compared to placebo (Abdnezhad et al., 2019). Vitex agnus-castus L and Hypericum perforatum L. with lower doses of vitamin B6 are well tolerated and effective drugs to treat females with moderate to severe premenstrual syndrome in Iran (Ghazanfarpour et al., 2016). In Persian traditional medicine, saffron (dried stigma of Crocus sativus L.) is used for depression, which has been confirmed by modern medicine to be achieved through a serotonergic mechanism (Agha-Hosseini et al., 2008). A review about treatments in Iran has shown a reduction in PMS symptoms after consumption Hypericum perforatum L. (St. John’s wort), Vitex agnus-castus L. (Chasteberry), Crocus sativus L. (saffron), Ginkgo biloba L. (ginkgo), and soy (Golmakani et al., 2010). This is consistent with the data that we collected.
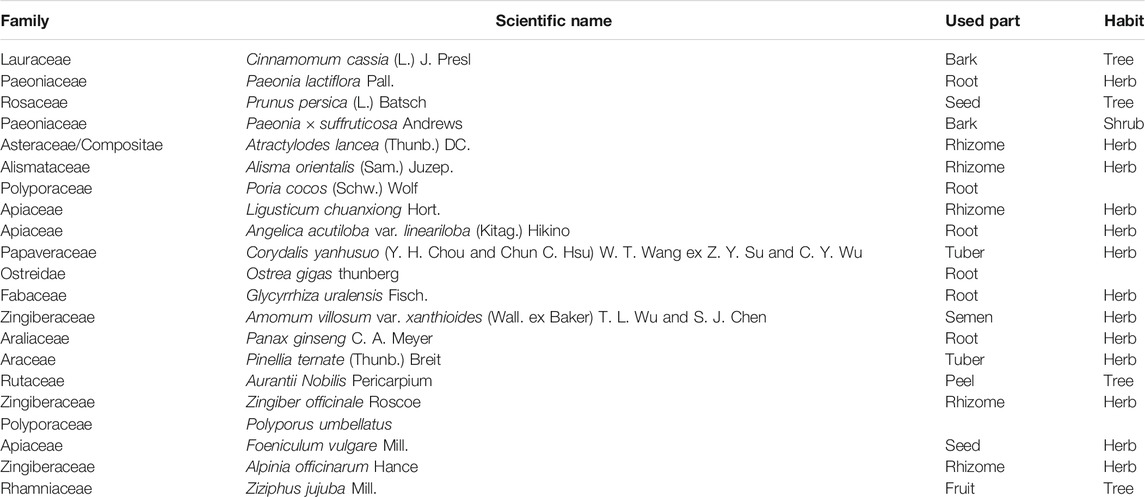
In Japan, Kampo medicine is the most preferred treatment choice for PMS. Kampo is a part of the official Japanese medical system and it is used alone or in combination with Western medicine for the treatment of complex health conditions, such as chronic health problems, age-related health problems, and lifestyle or stress-related disorders. We recorded 22 types of kampo’s that are the most commonly used ingredients (single herb) in PMS (Gepshtein et al., 2008) as shown in Table 2. Inochinohaha White is considered a medicine primarily used to treat PMS by attenuating anxiety-like behavior through GABAA receptor and brain-derived neurotrophic factor expression, which composed of 11 herbs: Angelica sinensis (Oliv.) Diels, Paeonia lactiflora Pall., Atractylodes lancea (Thunb.) DC., Cinnamomum verum J. Presl, Rheum palmatum L., Panax ginseng C. A. Meyer, Cnidium monnieri (L.) Cusson, Poria cocos (Schw.) Wolf, Alisma plantago-aquatica L., Paeonia suffruticosa Andr. and Prunus persica (L.) Batsch (Iba et al., 2021).
In Korea, herbal medicines for the treatment of PMS are Hypericum perforatum L. (St. John’s Wort), Odor of Crocus sativus L. (saffron), Vitex agnus-castus L. (Chasteberry), Ginkgo biloba L. (Ginkgo), Cirsium japonicum (Thunb.) Fisch. ex DC. (Cirsii Japonici Herba Carbonisata), Elsholtzia splendens Nakai ex F. Maekawa (Jang et al., 2012).
In South Africa, the pharmaceutical application of valerian (Valeriana officinalis L.) for the treatment of PMS is due to its sedative, anticonvulsant, hypnotic effects, and anxiolytic activity (Ghaderi and Jafari, 2014).
In summary, the most commonly used formula for the treatment of PMS in China is JXP. The most commonly used single drugs in the formulation are Cyperus rotundus L. and Angelica sinensis (Oliv.) Diels. In Western countries such as the United States, Vitex agnus-castus L. (chasteberry) and Matricaria chamomilla L. (chamomile) are regarded as the most available herbal alternative therapies.
3.2 Ethnic Herbal Medicine Used for Dysmenorrhea
Dysmenorrhea refers to the pain and swelling in the lower abdomen before and after menstruation or during menstruation, accompanied by backache or other discomfort (French, 2005). There are two types of dysmenorrhea: Primary dysmenorrhea refers to pain with no obvious pathological pelvic disease, whereas Secondary dysmenorrhea is caused by underlying pelvic conditions or pathology. Primary dysmenorrhea is considered to be caused by the release of prostaglandins in the menstrual fluid, which causes uterine contractions and pain. The reported prevalence of dysmenorrhea of any severity varies between 16 and 91% in women of reproductive age (Ju et al., 2014). Females who suffer from dysmenorrhea widely use non-steroidal anti-inflammatory drugs that reduce muscle spasm by inhibiting prostaglandin synthesis and vasopressin secretion (Sosorburam et al., 2019). In Western medicine, the main treatment trends tend to relieve prostaglandins synthesis and suppress their production from biosynthesis.
Native Americans commonly used whole plants of Artemisia californica Less. and fruits of Rhus glabra L. made a decoction to treat dysmenorrhea (Schmid and Moerman, 1998). Native American plants such as black haw (Viburnum prunifolium L.) and Viburnum opulus L. also utilized to treat painful menstruation (Lans et al., 2018).
According to the theories of CHM, the main cause of dysmenorrhea is Qi stasis caused by the invasion of the six exogenous pathogenic factors. Qi stasis results in the blockage of blood flow, which further leads to blood stasis and lumps. GeGen Decoction, Danggui Shaoyao Powder, and Guizhi Fuling Pillsare the famous Chinese prescriptions that are widely used in China to treat primary dysmenorrhea (Sosorburam et al., 2019). The ingredients of the Chinese herbal formulas are listed in Table 1. There are six types of Yao medicine used in treating dysmenorrhea, and among these three types of medicinal parts of plants are whole plants. Yao women are the best at using medicine baths to treat gynecological diseases, which is their ancient inheritance method (Long and Li, 2004; Li et al., 2006). As a famous herbal medicine used by Tujia and Miao Nationality, Panax japonicus (T. Nees) C. A. Mey is widely used for treating dysmenorrhea by local people (Deng et al., 2020). In Taiwan, Danggui Shaoyao Powder is the most frequently used formula that is prescribed by CHM doctors in Taiwan for treating menstrual cramps. The research shows that, among women with primary dysmenorrhea, CHM treatment is widely accepted by women in different ages, particularly those aged 21–30 years or those from lower income groups (Pan et al., 2014).
In India, a total of 38 types of herbs for the treatment of dysmenorrhea were collected from four pieces of literature (Jadhav and Bhutani, 2005; Vidyasagar and Prashantkumar, 2007; Bhatia et al., 2015; Das et al., 2015). Plants from the Asteraceae family are the main ones used to prepare dosages in the forms of decoction and infusion. Generally, they are administered orally. The leaf is the most important part of the plant that is used for medicinal purposes. Among them, 23 species are herbs, nine species are trees and two species are shrubs. Vitex negundo L. is the plant with the highest usage frequency. These four plants have been used in more than two countries: Artemisia vulgaris L., Achyranthes aspera L., Matricaria chamomilla L., and Foeniculum vulgare Mill. Artemisia vulgaris L. has been used to treat dysmenorrhea in India, Italy and Vietnam. Its multiple parts are effective in the treatment of dysmenorrhea.
In Italy, a total of 53 types of herbs were noted for the treatment of dysmenorrhea (Motti et al., 2019). The most common family of the plants are Asteraceae. The main forms of dosages are decoction and infusion. The most commonly used route of administration is oral administration. The most common medicinal parts are leaves. Among them, 37 species are herbs, eight species are trees, two species are shrubs and two species are vines. The herbal remedies mostly used for dysmenorrhea disorders are chamomile (Matricaria chamomilla L.), maidenhair fern (Adiantum capillus-veneris L.), yarrow (Achillea millefolium L.), and laurel (Laurus nobilis L.), which are taken orally, or as an infusion or decoction.
In South Africa, 30 types of plants are used to treat dysmenorrhea (Steenkamp, 2003). Roots are the medicinal parts of a majority of herbs. The most common dosage form is decoction. South Africa has a rich species of the herbs and most of them are local and unique species, such as Commelina africana L. Further, most of their names are related to the functional significance of the respective plants, such as Pterocarpus angolensis DC. (bloodwood), which is will used to treat dysmenorrhea, menorrhagia, and related diseases in South Africa. Euclea crispa Thunb. G˝urke is administered as enemas.
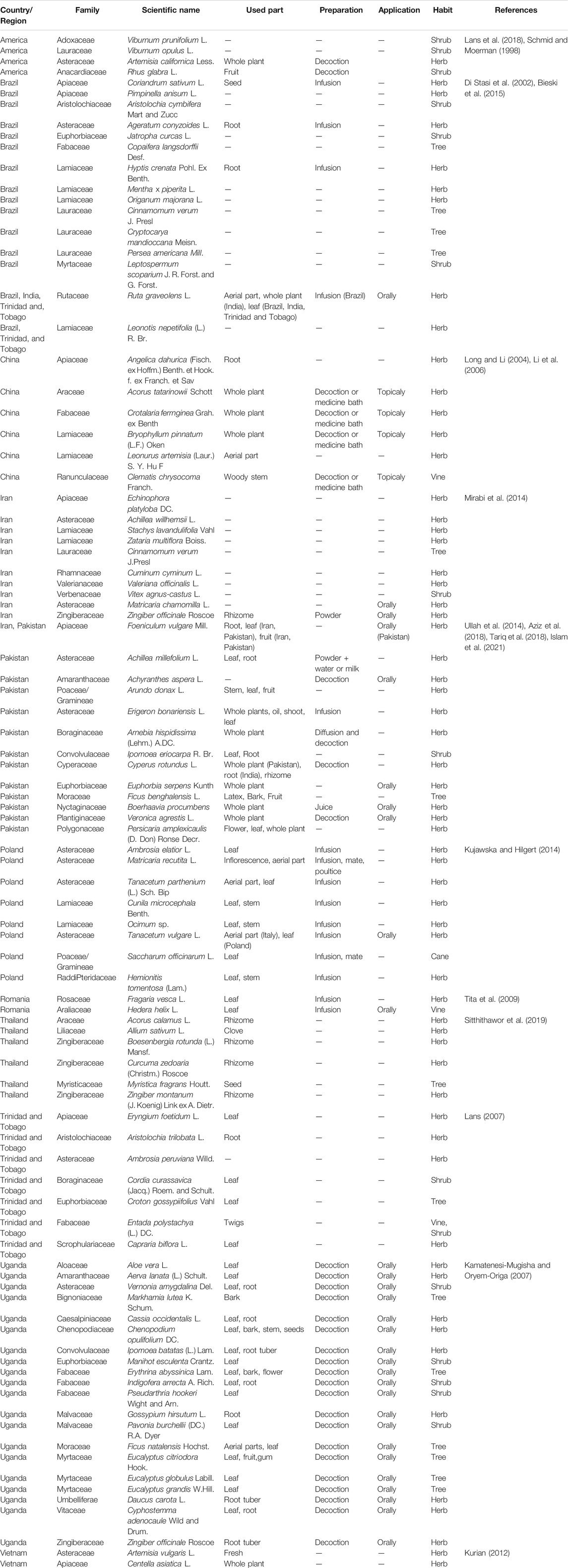
Herbs used in other countries to treat dysmenorrhea are listed in Table 3. See the Supplementary Material “Dysmenorrhea” for other specific contents.
This section contains a total of 80 families and 217 species of plants from 16 countries and regions that are used for the treatment of dysmenorrhea. Asteraceae is the most commonly used among such species and there are five plants that have records of treating dysmenorrhea in three countries Ruta graveolens L. can treat dysmenorrhea and this is mentioned in two Brazilian documents. Italian women use its aerial parts to make decoctions, while women from Trinidad and Tobago use its leaves. Leaves, flowers, stems, and fruits of Artemisia vulgaris L. are used in India to treat dysmenorrhea and amenorrhea. The fresh whole plant is used by Vietnamese women, while Italian women use its aerial parts to make an infusion to treat dysmenorrhea. Considering Cyperus rotundus L., Indian women use its root and rhizome, while Pakistani women use the whole plant to make a decoction for oral administration and Yunnan Yao women in China use its root. Considering Foeniculum vulgare Mill. (Fennel), Pakistani women use its leaves and fruits orally; Iranian women use its roots, leaves, and fruits; Italian women use a decoction made from its seeds; and Chinese women use its dried and mature fruit. All three countries use the rhizome of Zingiber officinale Roscoe (ginger) to treat menstrual pain but the dosage forms are different: Malaysians make a lotion, Indians make a decoction, and Iranians make a powder.
3.3 Ethnic Herbal Medicine Used for Amenorrhoea
Amenorrhea (loss of menstrual period) is the absence of menstruation or absence of periods. There are two types of amenorrhea: Primary amenorrhea and Secondary amenorrhea. Primary amenorrhea can be diagnosed if a patient has normal secondary sexual characteristics but no menarche by 16 years of age. Secondary amenorrhea is the absence of menses for 3 months in women with previously normal menstruation and for 9 months in women with oligomenorrhea previously (Master-Hunter and Heiman, 2006). Secondary amenorrhea is more common than primary amenorrhea. The normal menstrual cycle involves a complex interaction between the hypothalamic-pituitary-ovarian axis; any disruption in this interaction can cause amenorrhea (Edmonds, 2007). Among women of reproductive age, the prevalence of amenorrhea ranged from approximately 5–13% (Harlow and Campbell, 2004). Hormonal therapy based on estrogen and progesterone compounds is the mainstay of the treatment for such conditions (Bergeron et al., 2010).
In native American herbs used to treat amenorrhea, the roots of Acorus calamus L. are made into infusion, while the rhizomes of Acorus calamus L. are used to treat dysmenorrhea in Thailand (Schmid and Moerman, 1998).
CHM often uses herbs that promote blood circulation, remove blood stasis, regulate menstruation and relieve pain to treat amenorrhea. Generally, these herbs can simultaneously treat dysmenorrhea. Angelica sinensis (Oliv.) Diels, Leonurus japonicus Houtt., and Ligusticum chuanxiong Hort. (Miao et al., 2019) are the three typical examples. Curcuma longa L. is the herbal medicine used by Chinese and Malaysians to treat amenorrhea. Barks and twigs of Cinnamomum cassia (L.) J. Presl both appear in Chinese and Japanese herbal medicines for the treatment of amenorrhea.
Japanese Herbal (Kampo) Medicine, which is covered by national health insurance in Japan, is often prescribed in the primary care field, and is also applied as an alternative remedy for several gynecological diseases, such as MDs and menopausal symptoms. Tokishakuyakusan (Chinese name, Dang gui shao yao san), Keishibukuryogan (Chinese name, Gui zhi fu ling wan), Kamishoyosan (Chinese name, Jia wei xiao yao san) and Unkeito (Chinese name, Wen jing tang) are most commonly used by Japanese women. Paeonia lactiflora Pall. is the most frequently ingredient contained in all the four herbal formulas (Kogure, 2011). The ingredients of the Japanese herbal formulas are listed in Table 4.
Traditional Persian medicine (TPM), as a holistic system of medicine and based on temperament, has been used in Iran since thousands of years ago (Hosseinkhani et al., 2021). Temperament is made of action and reaction of four pivotal elements (fire, air, water, and soil) and creates different characteristics in living things. In TPM, temperament has been classified in different types: hot, cold, wet, and dry (Akhtari et al., 2020). Amenorrhea, oligomenorrhea, and hypomenorrhea are defined as “Ehtebas Tams” in TPM. From TPM viewpoint, anatomical and functional disorders (mal-temperaments) system are the main causes of oligomenorrhea and amenorrhea (Rahimi and Ardekani, 2013). The most prevalent temperaments of plants used to treat amenorrhea in Iranian medicine were warm and dry. Foeniculum vulgare Mill., Mentha longifolia (L.) L., Paeonia lactiflora Pall., Sesamum indicum L., and Vitex agnus-castus L. are the five most effective and documented herbs for treating amenorrhea (Moini Jazani et al., 2018).
In South Africa, plants belonging to 15 families are used for the treatment of amenorrhea. The most common plant families reported are the Fabaceae (five species) and Asteraceae (two species). Asparagus buchananii Baker is burnt and its smoke is directed into the vagina. Boscia foetida Schinz shows potential toxicity with hemorrhagic diarrhea. Powdered plant material is also applied to underwear: Albizia brevifolia Schinz, Brackenridgea zanguebarica Oliver, and Pterocarpus angolensis DC. are used for all for the treatment of amenorrhea (Steenkamp, 2003). The roots of Rhoicissus digitata (L. f.) Gilg and M. Brandt are chopped and mixed with the same number of chopped roots of Bridelia cathartica G. Bertol. and Peltophorum africanum Sond. Four handfuls of the mixed plant material are boiled in 5 L of water for 1 h in a pot with a lid on. Half a cup of the decoction is taken orally two to three times a day (depending on one’s preference). This decoction treats amenorrhea (de Wet and Ngubane, 2014).
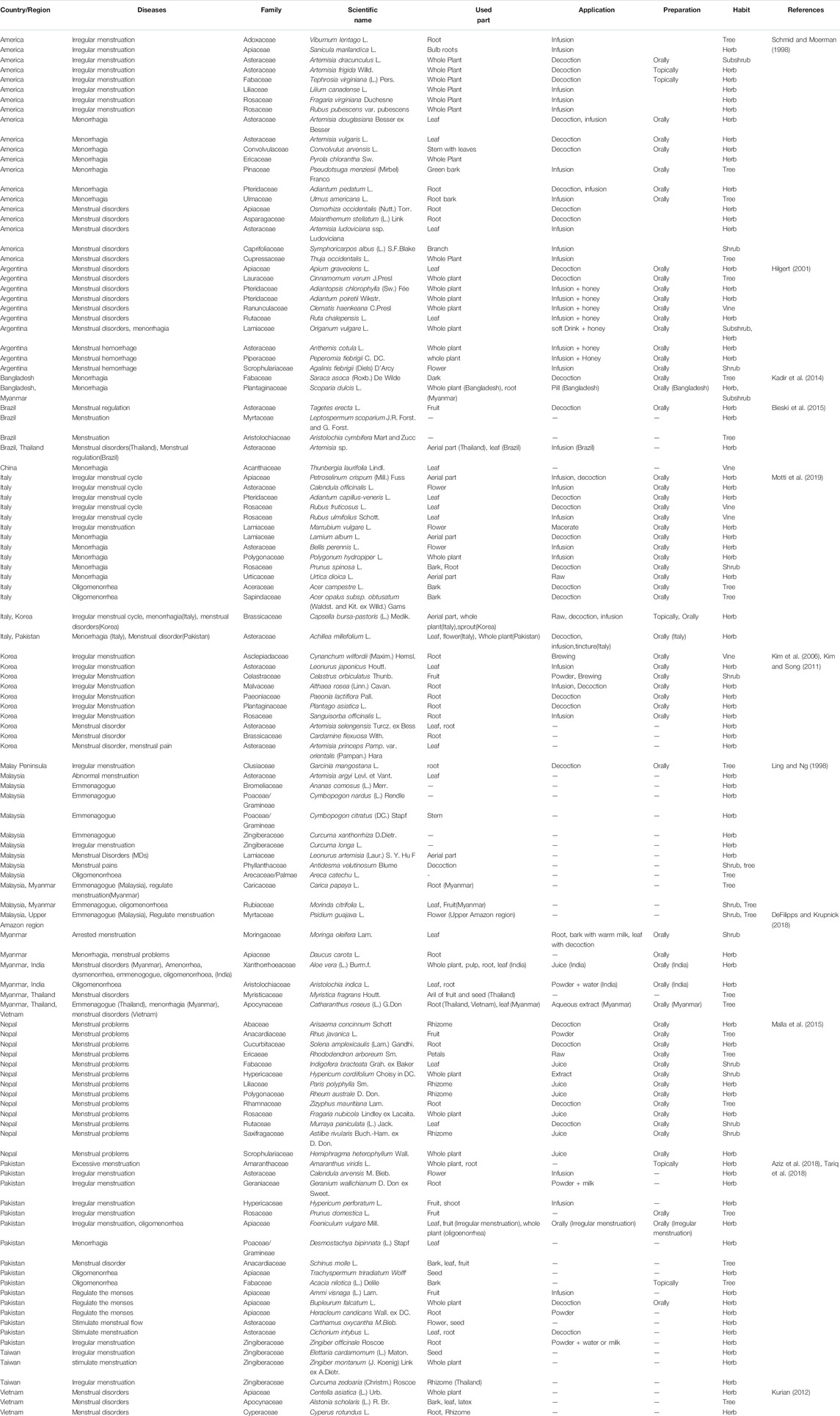
Herbs used in other countries and regions to treat amenorrhea are listed in Table 4. See the Supplementary Material “Amenorrhea” for other specific contents.
This part contains a total of 53 families and 99 species of plants from nine countries and regions used for the treatment of amenorrhea. Ranunculaceae family is the most commonly used among these species and some plants have records of treating amenorrhea in two countries: women use leaves of Aloe barbadensis Mill. in both India and Pakistan, but the dosage forms are different. Indian women make a gel for usage, while Pakistani women use its powder and milk. The whole plant of Amaranthus spinosus L. is made into a decoction in Pakistan and its roots are squeezed into a juice in Bangladesh.
3.4 Ethnic Herbal Medicine Used for Menstrual Disorders
MDs are some of the most common conditions to affect reproductive-aged women globally. They include abnormal menstrual cycle length, hypomenorrhea, and menorrhagia (Harlow et al., 2000). An epidemiological survey found that 27.2% of women suffered from MDs in five European countries (Fraser et al., 2015). Although estrogen therapy is beneficial in patients with MDs, its side effects such as nausea and vomiting had led to significant distress (Wang et al., 2020).
In America, Artemisia dracunculus L. (tarragon), whose whole plants are used for treating irregular menstruation by the Indians of the Missouri River Region, has long been used in traditional Asian medicine such as Myanmar while known as a spice species in Asia, Europe and the America (Ekiert et al., 2021). Native Americans use leaves of Artemisia vulgaris L. to treat irregular menstruation, while Indians, Italians and Vietnamese use it to treat dysmenorrhea (Schmid and Moerman, 1998).
The traditional Chinese medication experience and modern application of herbal medicine in treating MDs have enhanced people’s recognition of its importance and necessity. Dried products of herbal medicine are often used in traditional Chinese medicine which is convenient for transportation and storage. Rehmannia glutinosa (Rehjnannia glutinosa Libosch.) and its processed products play an important role in the treatment of irregular menstruation. Modern research shows (Zhang et al., 2008) that Chinese Rehmanniae Radix can prevent an inducement of the peripheral microcirculation of various chronic diseases through the improvement of hemorheology. Chinses angelica (Angelica sinensis (Oliv.) Diels) is a Chinese herbal medicine traditionally used for replenishing blood. Studies have shown that Angelica sinensis polysaccharide significantly reduced the apoptosis rate of platelets and had an anti-apoptosis effect on cryopreserved platelet (Nai et al., 2021).
In India, there are 73 species of plants used to treat MDs (Jadhav and Bhutani, 2005; Vidyasagar and Prashantkumar, 2007; Bhatia et al., 2015; Das et al., 2015). The major used family being Fabaceae; its leaves and roots are used often. Juice is the most frequently used method of administration, and oral administration is the most commonly used route of administration.
In Iran, a review suggests that the average prevalence of MDs is substantial (Omani Samani et al., 2018). Tansaz et al. (2015) summarized a variety of herbal medicines used for treating menorrhagia in Iran, including two forms, namely simple medicines and compound medicines. Plantain (Plantago asiatica L.) is one of the best medicinal plants used for menorrhagia treatment that is used by some of the traditional Iranian women. This plant is used either orally or vaginally. The other plant that is used frequently by Iranian traditional women is Punica granatum L., which grows in the wild in Iran, and it can be used either orally or topically. In the medical approach, traditional Iranian medicine physicians apply multiple drug dosage forms, such as oral, vaginal suppository, sitz bath, lotion, cleansing, and balm. These varieties increase a physician’s options in the management of menorrhagia and improve the compliance of patients.
In South Africa, Fabaceae is the most common family that appears in the treatment of menorrhagia among 31 plants (Steenkamp, 2003). Adenia gummifera (Harv.) Harms (Passifloraceae) and Xylopia longipetala De Wild. and T. Durand. (Annonaceae) are used as vaginal douches.
In Thailand, 25 species of plants are used to treat MDs (Sitthithawor et al., 2019). Zingiberaceae is the prominent family of species, while the primary part used is rhizome and oral administration is the major route of administration.
Herbs used in other countries and regions to treat MDs are listed in Table 5. See the Supplementary Material “Menstrual disorders” for other specific contents.
This section contains a total of 96 families and 287 species of plants from 15 countries and regions used for the treatment of MDs. Fabaceae is very common some plants have a record in treating MDs in more than two countries. There are three ways to use Punica granatum L. to treat menorrhagia in Iran: vaginal suppository, lotion, and balm (marham). In India, its raw dried peels are used for menorrhagia. Myanmar women use their leaves and roots to make decoctions. Women in Myanmar and Thailand use garlic (Allium sativum L.) bulbs to regulate menstruation.
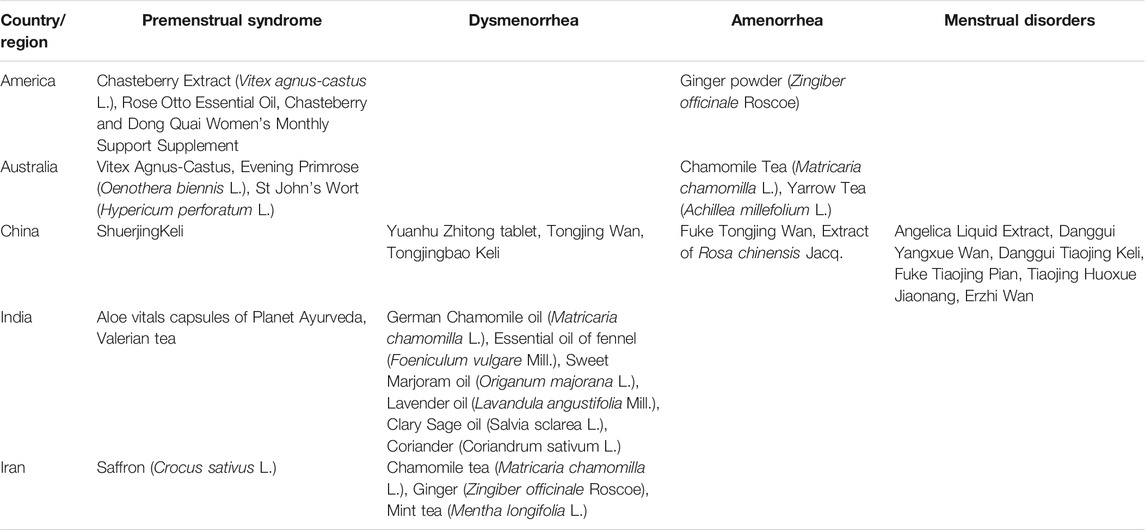
4 Herbal Medicine Products
The utilization of herbal medicine is increasing every year, which is reflected in the statistics of various countries. A study of participants from 23 countries reveals that 28.9% reported the use of herbal medicines in pregnancy (Kennedy et al., 2013). Approximately 35% of adults in the United States reported current use of herbal medicine (Rashrash et al., 2017). The sale of herbal medicines is growing by 20% annually and forms are the largest growth area in retail pharmacy. The sales of such products have moved from specialty stores to mainline shopping environments (Flanagan, 2001). The popularity of herbal medicine has spawned many health care industries, which have many herbal products on the market for menstrual problems. Table 6 lists some herbal products from various countries.
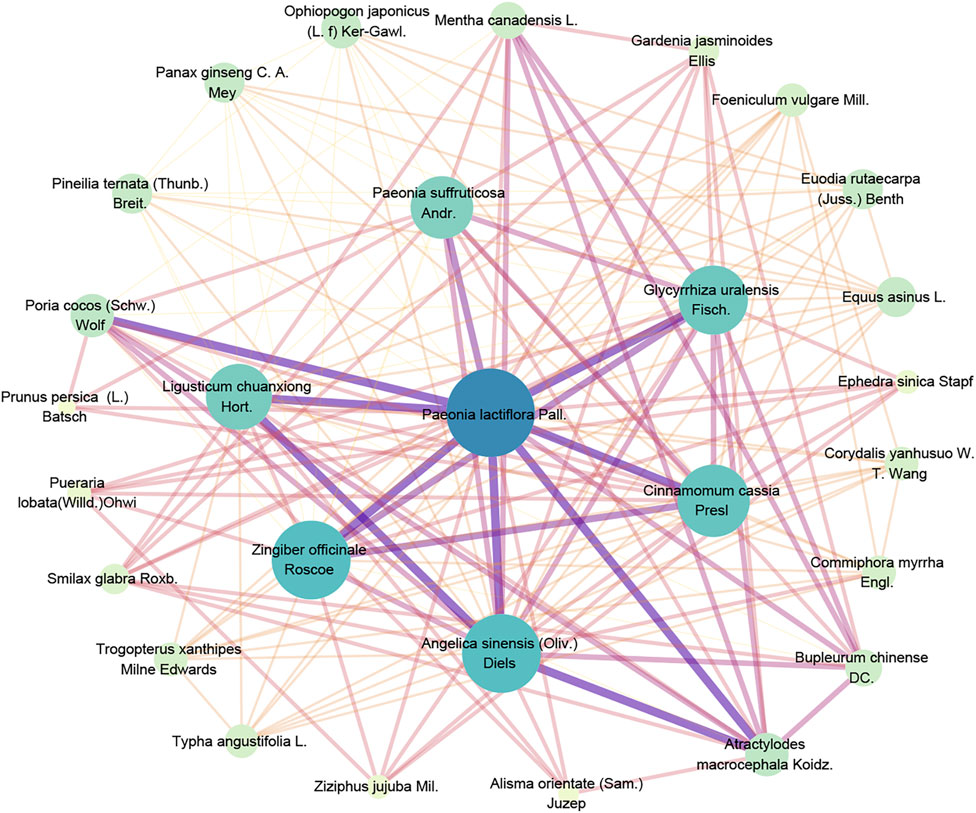
Compound Recipes are a major feature of herbal medicine in the treatment of MD. According to the most commonly used traditional Chinese medicine compound (TCMC) in MD showed in Table 1 as an example, there are seven formulae including nonredundant 28 herbs, which totally occurs 57 times, the main herb-pairs and compatibility laws of traditional Chinese medicine prescriptions are listed in Figure 1 as a network diagram obtained by the association rule algorithm-Apriori algorithm.
According to the network, Paeonia lactiflora Pall. was in the central with the most relationship with other herbs; Angelica sinensis (Oliv.) Diels., Zingiber officinale Roscoe., Cinnamomum cassia Presl., Glycyrrhiza uralensis Fisch., Ligusticum chuanxiong Hort., Paeonia suffruticosa Andr., Poria cocos (Schw.) Wolf., and Atractylodes macrocephala Koidz. within the second core layer, with extensive compatibility with other herbs, they are all the backbone medication of TCMC in treating MD.
Among them, according to the theory of TCMC, the Bupleurum-white peony drug pair can regulate menstruation and relieve pain and is also a frequently used drug pair for the treatment of various gynecological diseases. Ginger functions as warming menstruation and is most widely used in TCMC prescriptions for gynecological diseases. It can also be used as a “guiding herb” (which acts an ingredient added to enhance the efficacy of a dose of medicine), which is of great significance to improve the accuracy and efficacy of the medication. Licorice is commonly used in TCMC. It also plays a role in reconciling the medicinal properties and improving the taste. As such, it has a wide range of applications. Licorice can also play a role in pain relief, which is very beneficial in the relieving gynecological disease symptoms such as dysmenorrhea. Angelica is the holy medicine used in gynecology, Chuanxiong is the holy medicine used to activate blood stasis, and cinnamon functions as warming meridians, and atractylodes functions as drying dampness, invigorating the spleen, and relieving pain, which is of great significance for eliminating the cause of the disease.
As a creative contribution of CHM, the compound medicine experience of CHM has affected the traditional medical development of many countries in East Asia, and it will also provide a reference for the development of other ethnic medicines in the future.
5 Discussion and Conclusion
In this study, we screened 93 literatures on the topic of MD, among which a review “Medicinal plants used for menstrual disorders in Latin America, the Caribbean, sub-Saharan Africa, South and Southeast Asia and their uterine properties: A review” (van Andel et al., 2014) is similar on this theme, it mainly focuses on MDs and pay more attention on adverse reactions of related herbs. In our study, we systematically analyzed the herbal medicines used in countries and regions in treating different MD, compared the medication common characters and differences, and analyzed the compatibility law of classical prescriptions. As we know, our review is an unprecedented work on comprehensive analysis traditional herbs for MD globally.
Among the herbs used to treat MD, we analyzed 130 families and 571 species of plants used by women from different countries and regions. Among them, 451 are herbs, 178 are trees, 72 are shrubs, 21 are vines, five are climbers and 37 are of other types. The five main families are Asteraceae, Lamiaceae, Apiaceae, Fabaceae, and Zingiberaceae, while the five frequently used plants are Zingiber officinale Roscoe. (Ginger), Ruta graveolens L. (Common rue), Angelica sinensis (Oliv.) Diels (Angelica sinensis), Foeniculum vulgare Mill. (Fennel), and Catharanthus roseus (L.) G. Don (Catharanthus roseus). The general dosage of these herbs is 3–15 g.
Among them, some herbal medicines can treat three MD concurrently such as: Angelica sinensis (Oliv.) Diels (Angelica sinensis), Foeniculum vulgare Mill Ligusticum chuanxiong Hort., Cyperus rotundus L., Spatholobus suberectus Dunn, Leonurus japonicus Houtt., Salvia miltiorrhiza Bge., Prunus persica (L.) Batsch, Rosa chinensis Jacq., Curcuma longa L. while some herbal medicines that can treat two MD concurrently such as: Ruta graveolens L., Cinnamomum cassia (L.) J.Presl, Sargentodoxa cuneata (Oliv.) Rehd. et Wils., Corydalis yanhusuo W. T.Wang, Zingiber officinale Roscoe.
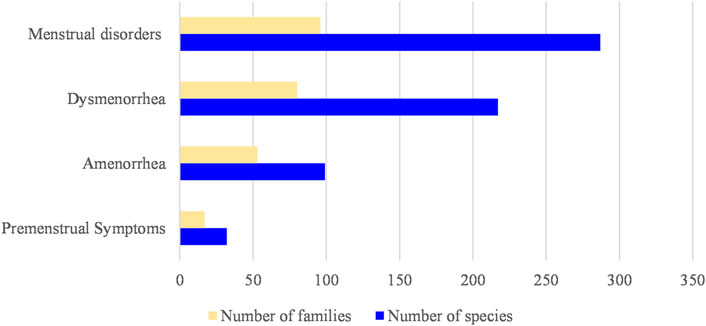
The number of families and species of plants corresponding to each disease type is listed in Figure 2. Most types of herbs treat MDs, for there are different symptom categories in MDs; however, considering a single symptom, most types of herbs treat dysmenorrhea. The number of herbs in treating PMS is the least in the four categories of MD, mainly because of PMS was proposed the latest.
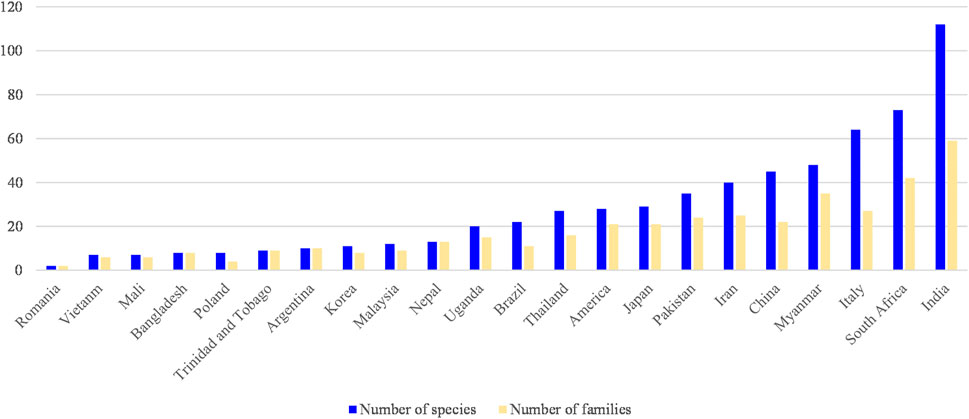
The number of families and species of plants corresponding to each country and region is listed in Figure 3, which shows that India has the most types of individual herbs used to treat MD. The selected literature indicted that India has more medical plant species resources and medication experience in MD, and it was similar for South Africa, Italy and Myanmar, for some literatures specifically collected and summarized herbs in treating MD in these countries or regions, but the application experience and pharmacological differences of many related plants need further research. In China, there are abundant medication experiences in treating MD, but the number of herbs was not increased indefinitely in a long application history, chiefly due to the concept of combined medication in CHM to solve many complex disease problems.
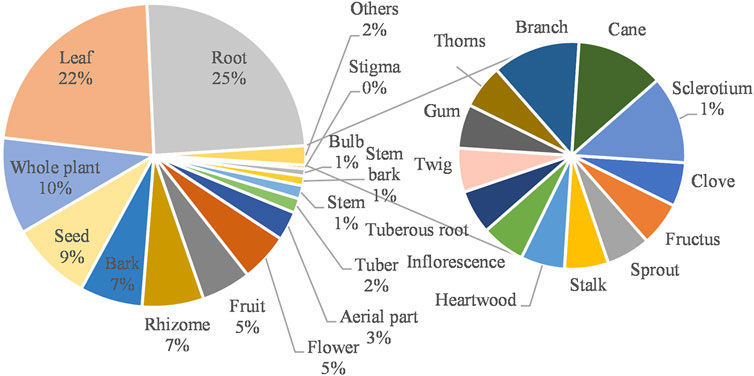
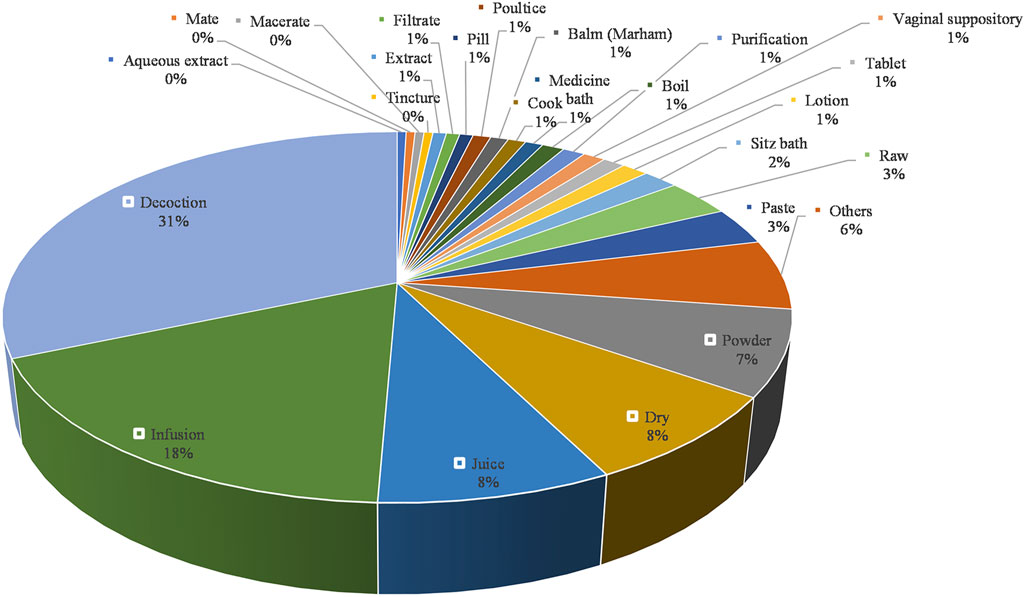
The usage of medicinal parts is listed in Figure 4, which presents the most commonly used parts which are root, leaf, whole plant, seed, bark, rhizome, fruit, flower, and aerial part. The usage of all the herbal medicines mentioned in the article is listed in Figure 5, which illustrates the three most commonly used preparations are decoction, infusion, and juice. Among the recorded routes of administration, 263 are oral administration and 50 are topical administration. The most commonly used type of dosage forms include decoction, infusion, juice, powder, dry, raw, paste, sitz bath, lotion, balm (Marham), and vaginal suppository. The most frequently used ingredients to match the dosage form are honey, milk, sugar, and other excipients, which may improve the taste of herbal medicines, moisturize the intestines and improve patient compliance for usage.
Among the recorded plants, many have culinary use in the population, such as Coriandrum sativum L. (Coriander Herb), Cuminum cyminum L. (Cumin), Crocus sativus L. (Saffron), Mentha pulegium L. (Pennyroyal), Mentha x piperita L. (Peppermint), Cinnamomum verum J. Presl (Ceylon cinnamon), Zingiber officinale Roscoe (Ginger), Allium sativum L. (Garlic), Foeniculum vulgare Mill. (Fennel), Capsella bursa-pastoris (Linn.) Medic. (Shepherd’s purse), Raphanus sativus L. (Radish), and Apium graveolens L. (Celery). Edible herbs are used in a wide range of countries or regions or have multiple effects on MD. This may mean that the edibility of herbal medicine has expanded its promotion. As such, it can be spread and applied in many countries and regions.
Some herbs have the same purpose in different countries. For example, ginger (Zingiber officinale Roscoe) is used to treat dysmenorrhea in India, Iran, and Malaysia; and the coriander herb (Coriandrum sativum L.) can treat menorrhagia in both India and Iran. Some herbs have different uses in different countries, such as Catharanthus roseus (Catharanthus roseus (L.) G. Don) is used to treat dysmenorrhea in India, amenorrhea in Myanmar, MDs in Vietnam, and as an emmenagogue in Thailand. East Asia, Pakistan, Malaysia, and some other places have recorded using fresh herbs. This may be because local therapists believe that fresh herbs are more effective (Pharmacopoeia Commission, 2020).
The application of some drugs is peculiar to this region. For example, Indian women use Vitex negundo L. to treat dysmenorrhea and amenorrhea, while Iranian women often use pomegranate (Punica granatum L.) to treat menorrhagia. Chinese women usually use roots of Angelica sinensis (Oliv.) Diels. for curing various MDs. The whole plant of Cirsium souliei (Franch.) Mattf. is applied to treat menorrhagia and the aerial part of Lagotis brevituba Maxim is used for menstrual regulation by Tibetan women (Zhu et al., 2017). Mongols frequently apply the aerial part of Panzeria alaschanica Kupr. to treat dysmenorrhea (Lei et al., 2017). As a traditional medicine of Uygur nationality, aerial part of Saussurea involucrata (Kar. et Kir.) Sch. -Bip is used for the treatment of excessive leucorrhea, but in CHM, it is used for irregular menstruation.
The sources of information on women’s use of plants come from herbal works, multi-media, the internet, medical education, ancestral medical inheritance, doctor-patient communication, neighborhood introduction, and self-exploration. For example, the elder Red-headed Yao women in China play an important role in the spread and utility of medicinal plants in treating gynecological diseases to young women. They can classify medicinal plants, and remember their functions and methods of disease treatment transferred to them from their previous generation.
East Asia has a long-standing habit of using herbal medicines, while in Western countries, herbal medicines have always been used as complementary and alternative treatments. In CHM, the specific details of the menstrual cycle (duration, volume, the appearance of flow, etc.) are not only the surface phenomena, which hint at the underlying causes of MD such as the dysfunction of the internal organs, disharmony of Qi, Blood and Body Fluids, imbalance of the Ren and Du meridians, and the irregularity of Kidney Essence, but symptomatic and causal treatment is required based on these phenomena (Zhou and Qu, 2009). As mentioned above, affected by the culture of Chinese medicine, Japan and South Korea have similar concepts in the treatment of MD, which is also reflected in their medication.
In conclusion, this study compares and summarizes the use of herbal medicines by women in different countries and regions globally. We hope to enlighten people working in these areas, and provide some insight on women’s medication.
Author Contributions
YR, MJ, and ZM conceived and designed the review. MJ, XL, YW, LC, YuL, YaL, TZ, WW, and YR wrote and reversed the paper.
Funding
This work was supported by National Natural Science Foundation of China grants (No. 81773893); National Major Scientific and Technological Special Project for “Significant New Drugs Development” (No. 2017ZX09301060-001); National Key R&D Plan of China (2018YFC1708004); Hubei Province Key R&D Programme (No. 2020BED017 and No.2020BGB004); Jiangxi Province “Thousand Talents Plan” of Scientific and Technological Innovation (No. JXSQ2019201105); Technological Innovation Project of Hubei province (2019AGB110).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fphar.2021.751207/full#supplementary-material
Abbreviations
CHM, Chinese herbal medicine; JXP, jiawei xiaoyao powder; MD, menstrual diseases; MDs, menstrual disorders; PMS, premenstrual syndrome; TPM, traditional Persian medicine.
References
Abdnezhad, R., Simbar, M., Sheikhan, Z., Mojab, F., Nasiri, M., Simbar, M., et al. (2019). Salvia Officinalis Reduces the Severity of the Premenstrual Syndrome. Complement. Med. Res. 26 (1), 39–46. doi:10.1159/000490104
Agha-Hosseini, M., Kashani, L., Aleyaseen, A., Ghoreishi, A., Rahmanpour, H., Zarrinara, A. R., et al. (2008). Crocus Sativus L. (Saffron) in the Treatment of Premenstrual Syndrome: a Double-Blind, Randomised and Placebo-Controlled Trial. BJOG 115 (4), 515–519. doi:10.1111/j.1471-0528.2007.01652.x
Akhtari, M., Moeini, R., Mojahedi, M., and Gorji, N. (2020). Assessment the Studies on the Concept of Mizaj (Temperament) in Persian Medicine. J. Complement. Integr. Med. 17 (3), 8. doi:10.1515/jcim-2018-0122
Aziz, M. A., Khan, A. H., Ullah, H., Adnan, M., Hashem, A., and Abd_Allah, E. F. (2018). Traditional Phytomedicines for Gynecological Problems Used by Tribal Communities of Mohmand Agency Near the Pak-Afghan Border Area. Rev. Bras. Farmacog. 28 (4), 503–511. doi:10.1016/j.bjp.2018.05.003
Bergeron, C., Nogales, F. F., Rechberger, T., Tatarchjuk, T., and Zipfel, L. (2010). Ultra Low Dose Continuous Combined Hormone Replacement Therapy with 0.5mg 17beta-Oestradiol and 2.5mg Dydrogesterone: protection of the Endometrium and Amenorrhoea Rate. Maturitas 66 (2), 201–205. doi:10.1016/j.maturitas.2010.03.007
Bhatia, H., Pal Sharma, Y., Manhas, R. K., and Kumar, K. (2015). Traditional Phytoremedies for the Treatment of Menstrual Disorders in District Udhampur, J&K, India. J. Ethnopharmacol. 160, 202–210. doi:10.1016/j.jep.2014.11.041
Bieski, I. G., Leonti, M., Arnason, J. T., Ferrier, J., Rapinski, M., Violante, I. M., et al. (2015). Ethnobotanical Study of Medicinal Plants by Population of Valley of Juruena Region, Legal Amazon, Mato Grosso, Brazil. J. Ethnopharmacol. 173, 383–423. doi:10.1016/j.jep.2015.07.025
Chai, C., Hong, F., Yan, Y., Yang, L., Zong, H., Wang, C., et al. (2020). Effect of Traditional Chinese Medicine Formula GeGen Decoction on Primary Dysmenorrhea: A Randomized Controlled Trial Study. J. Ethnopharmacol. 261, 113053. doi:10.1016/j.jep.2020.113053
Chen, H. Y., Huang, B. S., Lin, Y. H., Su, I. H., Yang, S. H., Chen, J. L., et al. (2014). Identifying Chinese Herbal Medicine for Premenstrual Syndrome: Implications from a Nationwide Database. BMC Complement. Altern. Med. 14 (1), 206. doi:10.1186/1472-6882-14-206
Chou, P. B., and Morse, C. A. (2005). Understanding Premenstrual Syndrome from a Chinese Medicine Perspective. J. Altern. Complement. Med. 11 (2), 355–361. doi:10.1089/acm.2005.11.355
Das, D., Sinha, N., and Das, M. (2015). The Use of Medicinal Plants for the Treatment of Gynaecological Disorders in the Eastern Parts of India. Indian J. Obstet. Gynaecol. 2, 16–27.
de Wet, H., and Ngubane, S. C. (2014). Traditional Herbal Remedies Used by Women in a Rural Community in Northern Maputaland (South Africa) for the Treatment of Gynaecology and Obstetric Complaints. South Afr. J. Bot. 94, 129–139. doi:10.1016/j.sajb.2014.06.009
DeFilipps, R. A., and Krupnick, G. A. (2018). The Medicinal Plants of Myanmar. PhytoKeys (102), 1–341. doi:10.3897/phytokeys.102.24380
Deng, X., Ren, Y. S., Lei, L., Zheng, Y., Li, Y., Liao, M. C., et al. (2020). Effects of Fufang Zhujieshen Granules on Oxytocin-Induced Primary Dysmenorrea. Chin. Tradit. Patent Med. 42 (01), 55–61. doi:10.3969/j.issn.1001-1528.2020.01.013
Di Stasi, L. C., Oliveira, G. P., Carvalhaes, M. A., Queiroz, M., Tien, O. S., Kakinami, S. H., et al. (2002). Medicinal Plants Popularly Used in the Brazilian Tropical Atlantic Forest. Fitoterapia 73 (1), 69–91. doi:10.1016/S0367-326X(01)00362-8
Direkvand Moghadam, A., Kaikhavani, S., and Sayehmiri, K. (2013). The Worldwide Prevalence of Premenstrual Syndrome: A Systematic Review and Meta-Analysis Study. Iranian J. Obstet. Gynecol. Infertility 16 (65), 8–17. doi:10.22038/IJOGI.2013.1877
Edmonds, D. K. (2007). “Primary Amenorrhoea,” in Dewhurst Postgraduate Textbook in Obstetrics & Gynaecology. Hoboken: Wiley-Blackwell, 369–376.
Ekiert, H., Świątkowska, J., Knut, E., Klin, P., Rzepiela, A., Tomczyk, M., et al. (2021). Artemisia Dracunculus (Tarragon): A Review of its Traditional Uses, Phytochemistry and Pharmacology. Front. Pharmacol. 12 (567), 653993. doi:10.3389/fphar.2021.653993
Flanagan, K. (2001). Preoperative Assessment: Safety Considerations for Patients Taking Herbal Products. J. Perianesth Nurs. 16 (1), 19–26. doi:10.1053/jpan.2001.20639
Fraser, I. S., Mansour, D., Breymann, C., Hoffman, C., Mezzacasa, A., and Petraglia, F. (2015). Prevalence of Heavy Menstrual Bleeding and Experiences of Affected Women in a European Patient Survey. Int. J. Gynaecol. Obstet. 128 (3), 196–200. doi:10.1016/j.ijgo.2014.09.027
Gao, L., Jia, C., Zhang, H., and Ma, C. (2017). Wenjing Decoction (Herbal Medicine) for the Treatment of Primary Dysmenorrhea: a Systematic Review and Meta-Analysis. Arch. Gynecol. Obstet. 296 (4), 679–689. doi:10.1007/s00404-017-4485-7
Gepshtein, Y., Plotnikoff, G. A., and Watanabe, K. (2008). Kampo in Women's Health: Japan's Traditional Approach to Premenstrual Symptoms. J. Altern. Complement. Med. 14 (4), 427–435. doi:10.1089/acm.2007.7064
Ghaderi, N., and Jafari, M. (2014). Efficient Plant Regeneration, Genetic Fidelity and High-Level Accumulation of Two Pharmaceutical Compounds in Regenerated Plants of Valeriana Officinalis L. South Afr. J. Bot. 92, 19–27. doi:10.1016/j.sajb.2014.01.010
Ghazanfarpour, M., Abdolahian, S., Khadivzadeh, T., and Kaviani, M. (2016). Hypericum Perforutum and Vitamin B6 as a Treatment for Premenstrual Syndrome. Jundishapur J. Nat. Pharm. Prod. 12 (2), 3. doi:10.5812/jjnpp.34093
Gnanasambanthan, S., and Datta, S. (2019). Premenstrual Syndrome. Obstet. Gynaecol. Reprod. Med. 29 (10), 281–285. doi:10.1016/j.ogrm.2019.06.003
Golmakani, N., Ebrahimzadeh, S., Homaie Rad, E., Hajizadeh, M., Rezaei, S., Reihanian, A., et al. (2010). Use of Medicinal Plants in the Treatment of Premenstrual Syndrome: A Review Utilization and Expenditures on Traditional and Herbal Medicines in Iran: 2009–2016. J. Am. Sci. 7, 100414. doi:10.1016/j.hermed.2020.100414
Harlow, S. D., and Campbell, O. M. (2004). Epidemiology of Menstrual Disorders in Developing Countries: a Systematic Review. BJOG 111 (1), 6–16. doi:10.1111/j.1471-0528.2004.00012.x
Harlow, S. D., Windham, G., and Paramsothy, P. (2000). “Menstruation and Menstrual Disorders,” in Women and Health. Waltham: Academic Press.
Hilgert, N. I. (2001). Plants Used in home Medicine in the Zenta River basin, Northwest Argentina. J. Ethnopharmacol. 76 (1), 11–34. doi:10.1016/S0378-8741(01)00190-8
Homaie Rad, E., Hajizadeh, M., Rezaei, S., Reihanian, A., Ehsani-Chimeh, E., and Davoudi-Kiakalayeh, A. (2021). Utilization and Expenditures on Traditional and Herbal Medicines in Iran: 2009-2016. J. Herbal Med. 25, 100414. doi:10.1016/j.hermed.2020.100414
Hosseinkhani, A., Ziaian, B., Hessami, K., Kashkooe, A., and Pasalar, M. (2021). An Evidence-Based Review of Antitussive Herbs Containing Essential Oils in Traditional Persian Medicine. Curr. Drug Discov. Technol. 18 (2), 179–185. doi:10.2174/1568009620666200421091245
Iba, H., Watanabe, T., Motomura, S., Harada, K., Uesugi, H., Shibahara, T., et al. (2021). A Japanese Herbal Medicine Attenuates Anxiety-like Behavior through GABAA Receptor and Brain-Derived Neurotrophic Factor Expression in a Rat Model of Premenstrual Syndrome. J. Pharmacol. Sci. 145 (1), 140–149. doi:10.1016/j.jphs.2020.11.003
Islam, M., InamullahAhmad, I., Ahmad, I., Akhtar, N., Alam, J., Razzaq, A., et al. (2021). Medicinal Plants Resources of Western Himalayan Palas Valley, Indus Kohistan, Pakistan: Their Uses and Degrees of Risk of Extinction. Saudi J. Biol. Sci. 28 (5), 3076–3093. doi:10.1016/j.sjbs.2021.02.051
Jadhav, A. N., and Bhutani, K. K. (2005). Ayurveda and Gynecological Disorders. J. Ethnopharmacol. 97 (1), 151–159. doi:10.1016/j.jep.2004.10.020
Jang, S.-H., Lee, E.-S., and Kim, D.-I. (2012). Review on the Treatment Methods of Korean Oriental Medicine for PMS. Soc. Korean Med. Obstet. Gynecol. 25 (2), 185–199. doi:10.15204/JKOBGY.2012.25.2.185
Ju, H., Jones, M., and Mishra, G. (2014). The Prevalence and Risk Factors of Dysmenorrhea. Epidemiol. Rev. 36 (1), 104–113. doi:10.1093/epirev/mxt009
Kadir, M. F., Bin Sayeed, M. S., Setu, N. I., Mostafa, A., and Mia, M. M. (2014). Ethnopharmacological Survey of Medicinal Plants Used by Traditional Health Practitioners in Thanchi, Bandarban Hill Tracts, Bangladesh. J. Ethnopharmacol. 155 (1), 495–508. doi:10.1016/j.jep.2014.05.043
Kamatenesi-Mugisha, M., and Oryem-Origa, H. (2007). Medicinal Plants Used in Some Gynaecological Morbidity Ailments in Western Uganda. Afr. J. Ecol. 45 (s1), 34–40. doi:10.1111/j.1365-2028.2007.00735.x
Kashanian, M., Mazinani, R., and Jalalmanesh, S. H. (2007). Pyridoxine (B6) for the Treatment of Premenstrual Syndrome (PMS). Eur. Psychiatry 22, S276. doi:10.1016/j.eurpsy.2007.01.932
Kennedy, D. A., Lupattelli, A., Koren, G., and Nordeng, H. (2013). Herbal Medicine Use in Pregnancy: Results of a Multinational Study. BMC Complement. Altern. Med. 13 (1), 355. doi:10.1186/1472-6882-13-355
Kim, H., and Song, M. J. (2011). Analysis and Recordings of Orally Transmitted Knowledge about Medicinal Plants in the Southern Mountainous Region of Korea. J. Ethnopharmacol. 134 (3), 676–696. doi:10.1016/j.jep.2011.01.024
Kim, H., Song, M. J., and Potter, D. (2006). Medicinal Efficacy of Plants Utilized as temple Food in Traditional Korean Buddhism. J. Ethnopharmacol. 104 (1), 32–46. doi:10.1016/j.jep.2005.08.041
Kim, S. M. (2019). CHAPTER 4. Negotiating Gynecology: Constant Imperatives, Evolving Options. Honolulu: University of Hawaii Press, 108–132.
Kogure, T. (2011). “Recent Clinical Applications of Kampo Medicine in Amenorrhea,” in Amenorrhea. Editor A. Chatterjee. :Slavka Krautzeka: InTech
Kujawska, M., and Hilgert, N. I. (2014). Phytotherapy of Polish Migrants in Misiones, Argentina: Legacy and Acquired Plant Species. J. Ethnopharmacol. 153 (3), 810–830. doi:10.1016/j.jep.2014.03.044
Kurian, J. C. (2012). Ethno-medicinal Plants of India, Thailand and Vietnam. J. Biodiversity 3 (1), 61–75. doi:10.1080/09766901.2012.11884737
Lans, C., Taylor-Swanson, L., and Westfall, R. (2018). Herbal Fertility Treatments Used in North America from Colonial Times to 1900, and Their Potential for Improving the success Rate of Assisted Reproductive Technology. Reprod. Biomed. Soc. Online 5, 60–81. doi:10.1016/j.rbms.2018.03.001
Lans, C. (2007). Ethnomedicines Used in Trinidad and Tobago for Reproductive Problems. J. Ethnobiol. Ethnomed. 3 (1), 13. doi:10.1186/1746-4269-3-13
Lee H, H., Choi, T. Y., Myung, C. S., Lee, J. A., and Lee, M. S. (2016). Herbal Medicine (Shaofu Zhuyu Decoction) for Treating Primary Dysmenorrhea: A Systematic Review of Randomized Clinical Trials. Maturitas 86, 64–73. doi:10.1016/j.maturitas.2016.01.012
Lee HW, H. W., Jun, J. H., Kil, K. J., Ko, B. S., Lee, C. H., and Lee, M. S. (2016). Herbal Medicine (Danggui Shaoyao San) for Treating Primary Dysmenorrhea: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Maturitas 85, 19–26. doi:10.1016/j.maturitas.2015.11.013
Lei, G. F., Zhao, X. P., and Zhu, D. (2017). Progress of Mongolian Herb Panzeria Alaschanica Kupr. In Chemical Components and Clinical Application. China J. Tradit. Chin. Med. Pharm. 32 (07), 3083–3085.
Li, S., Long, C., Liu, F., Lee, S., Guo, Q., Li, R., et al. (2006). Herbs for Medicinal Baths Among the Traditional Yao Communities of China. J. Ethnopharmacol. 108 (1), 59–67. doi:10.1016/j.jep.2006.04.014
Li, M., Bi, J., Lv, B., Zheng, W., Wang, Z., Xiao, W., et al. (2019). An Experimental Study of the Anti-dysmenorrhea Effect of Chinese Herbal Medicines Used in Jin Gui Yao Lue. J. Ethnopharmacol. 245, 112181. doi:10.1016/j.jep.2019.112181
Ling, S. K., and Ng, L. T. (1998). Medicinal Plants Used for Treating Female Diseases in Malaysia--a Review. Am. J. Chin. Med. 26 (02), 211–222. doi:10.1142/S0192415X98000269
Liu, X. J., Wang, Y. Z., Wei, F. X., Lv, M., Qu, P., Chen, S. J., et al. (2021). The Synergistic Anti-depression Effects of Different Efficacy Groups of Xiaoyaosan as Demonstrated by the Integration of Network Pharmacology and Serum Metabolomics. J. Pharm. Biomed. Anal. 197, 113949. doi:10.1016/j.jpba.2021.113949
Long, C. L., and Li, R. (2004). Ethnobotanical Studies on Medicinal Plants Used by the Red-Headed Yao People in Jinping, Yunnan Province, China. J. Ethnopharmacol. 90 (2), 389–395. doi:10.1016/j.jep.2003.10.021
Maleki-Saghooni, N., Karimi, F. Z., Behboodi Moghadam, Z., and Mirzaii Najmabadi, K. (2018). The Effectiveness and Safety of Iranian Herbal Medicines for Treatment of Premenstrual Syndrome: A Systematic Review. Avicenna J. Phytomed. 8 (2), 96–113. doi:10.22038/AJP.2018.22810.1848
Malla, B., Gauchan, D. P., and Chhetri, R. B. (2015). An Ethnobotanical Study of Medicinal Plants Used by Ethnic People in Parbat District of Western Nepal. J. Ethnopharmacol. 165, 103–117. doi:10.1016/j.jep.2014.12.057
Master-Hunter, T., and Heiman, D. L. (2006). Amenorrhea: Evaluation and Treatment. Am. Fam. Phys. 73 (8), 1374–1382.
Miao, L. L., Zhou, Q. M., Peng, C., Liu, Z. H., and Xiong, L. (2019). Leonurus Japonicus (Chinese Motherwort), an Excellent Traditional Medicine for Obstetrical and Gynecological Diseases: A Comprehensive Overview. Biomed. Pharmacother. 117, 109060. doi:10.1016/j.biopha.2019.109060
Mirabi, P., Alamolhoda, S. H., Esmaeilzadeh, S., and Mojab, F. (2014). Effect of Medicinal Herbs on Primary Dysmenorrhoea- a Systematic Review. Iran J. Pharm. Res. 13 (3), 757–767. doi:10.22037/IJPR.2014.1547
Moini Jazani, A., Hamdi, K., Tansaz, M., Nazemiyeh, H., Sadeghi Bazargani, H., Fazljou, S. M. B., et al. (2018). Herbal Medicine for Oligomenorrhea and Amenorrhea: A Systematic Review of Ancient and Conventional Medicine. Biomed. Res. Int. 2018, 3052768. doi:10.1155/2018/3052768
Morehead, A., and McInnis, L. A. (2021). Herbal Supplements for Common Women's Health Issues. Nurs. Clin. North Am. 56 (1), 69–78. doi:10.1016/j.cnur.2020.10.006
Motti, R., Bonanomi, G., Emrick, S., and Lanzotti, V. (2019). Traditional Herbal Remedies Used in Women's Health Care in Italy: a Review. Hum. Ecol. 47 (6), 941–972. doi:10.1007/s10745-019-00125-4
Nai, J., Zhang, C., Shao, H., Li, B., Li, H., Gao, L., et al. (2021). Extraction, Structure, Pharmacological Activities and Drug Carrier Applications of Angelica Sinensis Polysaccharide. Int. J. Biol. Macromol. 183, 2337–2353. doi:10.1016/j.ijbiomac.2021.05.213
O’Brien, S., Rapkin, A., and Dennerstein, L. (2011). Diagnosis and Management of Premenstrual Disorders. BMJ 343, d5032. doi:10.1136/bmj.d5032
Omani Samani, R., Almasi Hashiani, A., Razavi, M., Vesali, S., Rezaeinejad, M., Maroufizadeh, S., et al. (2018). The Prevalence of Menstrual Disorders in Iran: A Systematic Review and Meta-Analysis. Int. J. Reprod. Biomed. 16 (11), 665–678.
Pan, J. C., Tsai, Y. T., Lai, J. N., Fang, R. C., and Yeh, C. H. (2014). The Traditional Chinese Medicine Prescription Pattern of Patients with Primary Dysmenorrhea in Taiwan: A Large-Scale Cross Sectional Survey. J. Ethnopharmacol. 152 (2), 314–319. doi:10.1016/j.jep.2014.01.002
Peltzer, K. (2009). Utilization and Practice of Traditional/complementary/alternative Medicine (TM/CAM) in South Africa. Afr. J. Tradit. Complement. Altern. Med. 6 (2), 175–185.
Pharmacopoeia Commission (2020). Pharmacopoeia of the People's Republic of China. Beijing: China Medical Science Press.
Rahimi, R., and Ardekani, M. R. (2013). Medicinal Properties of Foeniculum Vulgare Mill. In Traditional Iranian Medicine and Modern Phytotherapy. Chin. J. Integr. Med. 19 (1), 73–79. doi:10.1007/s11655-013-1327-0
Rashrash, M., Schommer, J. C., and Brown, L. M. (2017). Prevalence and Predictors of Herbal Medicine Use Among Adults in the United States. J. Patient Exp. 4 (3), 108–113. doi:10.1177/2374373517706612
Schmid, R., and Moerman, D. E. (1998). Native American Ethnobotany. Taxon 47, 980. doi:10.2307/1224232
Sitthithawor, W., Weerasathien, L., and Onsawang, C. (2019). The Use of Medicinal Plants for Gynecologic Ailments by Thai Traditional Folk Healers in Nakhonnayok Province. Thai Pharm. Health Sci. J. 14 (3), 111–121.
Sosorburam, D., Wu, Z.-g., Zhang, S.-c., Hu, P., Zhang, H.-y., Jiang, T., et al. (2019). Therapeutic Effects of Traditional Chinese Herbal Prescriptions for Primary Dysmenorrhea. Chin. Herbal Med. 11 (1), 10–19. doi:10.1016/j.chmed.2018.11.001
Steenkamp, V. (2003). Traditional Herbal Remedies Used by South African Women for Gynaecological Complaints. J. Ethnopharmacol. 86 (1), 97–108. doi:10.1016/S0378-8741(03)00053-9
Sun, L., Liu, L., Zong, S., Wang, Z., Zhou, J., Xu, Z., et al. (2016). Traditional Chinese Medicine Guizhi Fuling Capsule Used for Therapy of Dysmenorrhea via Attenuating Uterus Contraction. J. Ethnopharmacol. 191, 273–279. doi:10.1016/j.jep.2016.06.042
Tansaz, M., Memarzadehzavareh, H., Qaraaty, M., Eftekhar, T., Tabarrai, M., and Kamalinejad, M. (2015). Menorrhagia Management in Iranian Traditional Medicine. J. Evid. Based Complement. Altern. Med. 21 (1), 71–76. doi:10.1177/2156587215589522
Tariq, A., Adnan, M., Iqbal, A., Sadia, S., Fan, Y., Nazar, A., et al. (2018). Ethnopharmacology and Toxicology of Pakistani Medicinal Plants Used to Treat Gynecological Complaints and Sexually Transmitted Infections. South Afr. J. Bot. 114, 132–149. doi:10.1016/j.sajb.2017.11.004
Tita, I., Mogosanu, G., and Tita, M. (2009). Ethnobotanical Inventory of Medicinal Plants from the South-West of Romania. Farmacia 57, 141–156.
Ullah, S., Rashid Khan, M., Ali Shah, N., Afzal Shah, S., Majid, M., and Asad Farooq, M. (2014). Ethnomedicinal Plant Use Value in the Lakki Marwat District of Pakistan. J. Ethnopharmacol. 158, 412–422. doi:10.1016/j.jep.2014.09.048
van Andel, T., de Boer, H. J., Barnes, J., and Vandebroek, I. (2014). Medicinal Plants Used for Menstrual Disorders in Latin America, the Caribbean, Sub-Saharan Africa, South and Southeast Asia and Their Uterine Properties: A Review. J. Ethnopharmacol. 155 (2), 992–1000. doi:10.1016/j.jep.2014.06.049
Vidyasagar, G. M., and Prashantkumar, P. (2007). Traditional Herbal Remedies for Gynecological Disorders in Women of Bidar District, Karnataka, India. Fitoterapia 78 (1), 48–51. doi:10.1016/j.fitote.2006.06.017
Vrolijk, M. F., Opperhuizen, A., Jansen, E. H. J. M., Hageman, G. J., Bast, A., and Haenen, G. R. M. M. (2017). The Vitamin B6 Paradox: Supplementation with High Concentrations of Pyridoxine Leads to Decreased Vitamin B6 Function. Toxicol. Vitro 44, 206–212. doi:10.1016/j.tiv.2017.07.009
Walsh, S., Ismaili, E., Naheed, B., and O'Brien, S. (2015). Diagnosis, Pathophysiology and Management of Premenstrual Syndrome. Obstet. Gynecol. 17 (2), 99–104. doi:10.1111/tog.12180
Wang, C., Lv, X., Liu, W., Liu, S., and Sun, Z. (2020). Uncovering the Pharmacological Mechanism of Motherwort (Leonurus Japonicus Houtt.) for Treating Menstrual Disorders: A Systems Pharmacology Approach. Comput. Biol. Chem. 89, 107384. doi:10.1016/j.compbiolchem.2020.107384
Weisz, G., and Knaapen, L. (2009). Diagnosing and Treating Premenstrual Syndrome in Five Western Nations. Soc. Sci. Med. 68 (8), 1498–1505. doi:10.1016/j.socscimed.2009.01.036
Zhang, R. X., Li, M. X., and Jia, Z. P. (2008). Rehmannia Glutinosa: Review of Botany, Chemistry and Pharmacology. J. Ethnopharmacol. 117 (2), 199–214. doi:10.1016/j.jep.2008.02.018
Zhou, J., and Qu, F. (2009). Treating Gynaecological Disorders with Traditional Chinese Medicine: a Review. Afr. J. Tradit. Complement. Altern. Med. 6 (4), 494–517. doi:10.4314/ajtcam.v6i4.57181
Keywords: herb medicine, ethnomedicine, premenstrual syndrome, dysmenorrhea, amenorrhea, menstrual disorders, women's health
Citation: Jiao M, Liu X, Ren Y, Wang Y, Cheng L, Liang Y, Li Y, Zhang T, Wang W and Mei Z (2022) Comparison of Herbal Medicines Used for Women’s Menstruation Diseases in Different Areas of the World. Front. Pharmacol. 12:751207. doi: 10.3389/fphar.2021.751207
Received: 31 July 2021; Accepted: 16 December 2021;
Published: 04 February 2022.
Edited by:
Ashwell Rungano Ndhlala, University of Limpopo, South AfricaReviewed by:
Cheng Lu, Chinese Academy of Medical Sciences and Peking Union Medical College, ChinaSefirin Djiogue, University of Yaounde I, Cameroon
Semakaleng Mpai, University of Limpopo, South Africa
Copyright © 2022 Jiao, Liu, Ren, Wang, Cheng, Liang, Li, Zhang, Wang and Mei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongshen Ren, godreny@mail.scuec.edu.cn
†These authors have contributed equally to this work and share first authorship
 Majing Jiao
Majing Jiao Xinqiao Liu†
Xinqiao Liu† Yongshen Ren
Yongshen Ren Wen Wang
Wen Wang Zhinan Mei
Zhinan Mei