- School of Nursing, Yangzhou University, Yangzhou, China
Background: Patients with chronic heart failure and their family caregivers may experience adverse emotional problems, such as depression. Mutuality, which refers to the relationship between caregivers and those they care for, is an important factor affecting depression in the dyads. The purpose of this study was to investigate the relationship between mutuality and depression in patients with CHF and their caregivers in China.
Methods: In this cross-sectional study, we used the Mutuality Scale and the Self-Rating Depression Scale to measure mutuality and depression of patients and caregivers. We used SPSS version 26.0 and AMOS version 21.0 to analyze the data. An APIM was established to analyze the actor-partner effects of patient-caregiver mutuality and depression.
Results: A total of 250 dyads of patients and caregivers were included in the study. There were statistically significant differences in mutuality and depression between CHF patients and caregivers. The 4 dimensions of patients’ mutuality all have the actor effect on depression. There were 3 partner effects of caregivers’ “pleasurable activities”, “shared values”, and “reciprocity” on depression. Regarding caregiver depression, we only found an actor effect of caregivers’ “shared values” on depression.
Conclusion: The relationship between patients and caregivers should be evaluated in the clinical setting, and it is very important to develop intervention measures to improve the adverse emotional problems affecting both patients and their caregivers.
Introduction
Chronic heart failure (CHF) is a syndrome of cardiac insufficiency caused by various heart diseases, and it is also the end stage of heart disease (Chinese Association of Cardiology Heart Failure Group, 2018). The American Heart Association predicts that 8 million Americans will suffer from HF by 2030 (Virani et al., 2020). The Writing Committee of the Report on Cardiovascular Health and Diseases in China reported that 8.9 million patients suffered from HF in 2019 (The Writing Committee of the Report on Cardiovascular Health and Diseases in China, 2020) and its prevalence continues to rise according to Expert Committee of Chinese Heart Failure Center (Expert Committee of Chinese Heart Failure Center, 2018). The prevalence of CHF in the population of China is 0.9% (Chen et al., 2015). Symptoms of CHF can recur, and patients usually need to be hospitalized more than once. In China, the one-year readmission rate for patients with CHF was 56% in 2018 (Al-Omary et al., 2018). CHF is characterized by high prevalence, high readmission rate, and high medical expense (Benjamin et al., 2019), and it causes great distress and burden to patients and their families (Liu et al., 2020).
The high prevalence, mortality, and readmission rates of CHF lead to negative emotions, such as depression in both patients and their caregivers. People with depression are more likely to develop HF and depression increases the probability of death in patients with HF (Adelborg et al., 2016; Chobufo et al., 2020). Caregivers with HF also have a higher prevalence of depression, and caregiver depression is associated with an increased risk of poor quality of life (Clements et al., 2020). In addition, depression in patients with HF has been shown to be associated with poorer emotional health among caregivers (Chung et al., 2016).
Mutuality refers to the relationship between caregivers and those they care for, and it can reflect the positive quality of the relationship between patients and caregivers (Archbold et al., 1990). Mutuality is a feeling of intimacy, connection, and understanding of others. It is a feeling of sharing, participating, and satisfying others (Liu, 2006). It represents the emotional connection between patients and caregivers. Mutuality is composed of 4 dimensions, which reflect love and affection, pleasurable activities, shared values, and reciprocity. Some scholars have studied the relationship between patients with HF and their main family caregivers in the United States and Italy, and the results showed that mutuality was above the average level and that patients perceived a higher mutuality than did their main family caregivers (Hooker et al., 2018; Vellone et al., 2018; Dellafiore et al., 2019). Similar results were found in a Chinese study (Zhang et al., 2020). In patients with cancer, higher levels of patient-caregiver dyads interactions were associated with lower anxiety and depression in patients (Schumacher et al., 2007). Similar findings were reported for patients with dementia (Shyu et al., 2010) and coronary heart disease (Halm and Bakas, 2007). Studies showed that the mutuality was associated with positive emotions in CHF patients and caregivers in China (Gong et al., 2021; Peng et al., 2021). Patients and family caregivers are interdependent interactive systems when facing the disease together, in which they can perceive, assess, communicate and cope with stress. The dyads who perceive better mutuality may adopt positive coping behaviors, such as positive and timely communication between the dyads, which can reduce conflict and negative emotions (Li et al., 2022). To date, the relationship between mutuality and depression in CHF patients and caregivers is rarely reported. The question of how does mutuality between patients and caregivers impact dyads’ emotions remains.
There is limited information about whether patients’ and caregivers’ mutuality are related to their depression. In addition, most previous studies examined the relationship between mutuality and depression at the individual level. Therefore, it is necessary to explore the interaction between patients and caregivers at the dyad level.
Both patients and caregivers are affected by the patients’ illness, and there are also interactions between the dyads. The actor-partner interdependence model (APIM) can be used to examine the relationship between dyadic variables (Lyons and Lee, 2018). The individual dependent variable is not only affected by the individual independent variable but also by the independent variable of others (Kenny and Cook, 1999). The effect of a person’s independent variable on the person’s own dependent variable is called the actor effect. The effect of a person’s independent variable on his/her dyadic partner’s dependent variable called the partner effect. The model takes into account the non-independence of the individual data in the dyadic relationship, and the interdependence of the dyadic data can be controlled using the model. In China, researchers have applied the APIM to study the effect of intimate relationships on quality of life of colorectal cancer patients and their family caregivers (Wu et al., 2020). However, the APIM has not been used to explore the relationship between mutuality and depression in CHF patients and their caregivers. Therefore, the objectives of this study were to compare the level of mutuality and depression between patients with CHF and their caregivers and evaluate whether the depression of patients and caregivers is related to their mutuality.
Materials and methods
Design
This cross-sectional study was a secondary analysis from data collected in a study evaluating the effects of mutuality, unmet needs on depression in CHF patient-caregiver dyads. The study was powered to answer the main outcome of the parent study. In order to better understand the effect of mutuality on depression. In this secondary analysis, we also analyzed the effects of four dimensions of mutuality on depression. The Ethics Committee of the School of Nursing, Yangzhou University approved the research protocol (approval number: YZUHL20200013).
Sample and setting
In the parent study, patients with CHF who were admitted to two grade A general hospitals in Yangzhou, China from March to May 2021 and their family caregivers were investigated. Inclusion criteria for patients were: (1) meeting the diagnostic and grading criteria for CHF set by the New York College of Cardiology and being diagnosed as having CHF with New York Heart Association class ranging from I to IV; diagnosed for ≥ 1 month; (2) 18 years or older; (3) having at least one family caregiver; (4) able to complete the questionnaire in written or oral form; and (5) provided informed consent and voluntary participation. Exclusion criteria for patients were: (1) having other critical diseases, such as malignant tumor, renal failure, or respiratory failure; or (2) cognitive impairment or mental disease. Inclusion criteria for family caregivers were: (1) being the primary caregiver of the patient, who provided free care; (2) 18 years or older; (3) able to complete the questionnaire in written or oral form; and (4) provided informed consent and voluntary participation. Exclusion criteria for family caregivers were: (1) receiving payment for care; (2) having cognitive impairment or mental disease; or (3) having serious physical diseases, such as cancer or severe organ failure.
Measurements
We used the Mutuality Scale (MS), developed by Archbold (Archbold et al., 1990) in 1990, to explore the relationship between patients and caregivers. The scale contains 15 items included in the dimensions of love and affection, pleasurable activities, shared values, and reciprocity. A Likert 5-level scoring method was used for all items, with 0 indicating not at all and 4 indicating a great deal, and the average scoring method was adopted. Mutuality scores were converted to a standardized score of 0-100 for each domain (converted score = [(actual raw data-0)/(4-0)] × 100). A score of 0 indicates the worse mutuality, and a score of 100 indicates the better mutuality. Higher scores indicate better mutuality, whereas a score <2.5 (converted score <62.5) indicated poor mutuality (Kneeshaw et al., 1999; Zhang et al., 2020; Gong et al., 2021). This scale was introduced to China by Liu in 2006 (Liu, 2006). The total Cronbach’s alpha was 0.94.
We used the Self-Rating Depression Scale (SDS) to evaluate the depression status of patients and caregivers. The scale consists of 20 items, and a Likert 4-level scoring method was used. The scores of the 20 items are summed to obtain the total rough score, which is then multiplied by 1.25 and rounded to obtain the standard score. A higher score indicates greater likelihood of being depressed. Liu et al. (1995) used the Chinese version of the SDS to evaluate 560 people and the Cronbach’s alpha was 0.86. The results of structural validity analysis were in line with the evaluation requirements of the scale, indicating that the SDS has good reliability and validity. The total Cronbach’s alpha was 0.82.
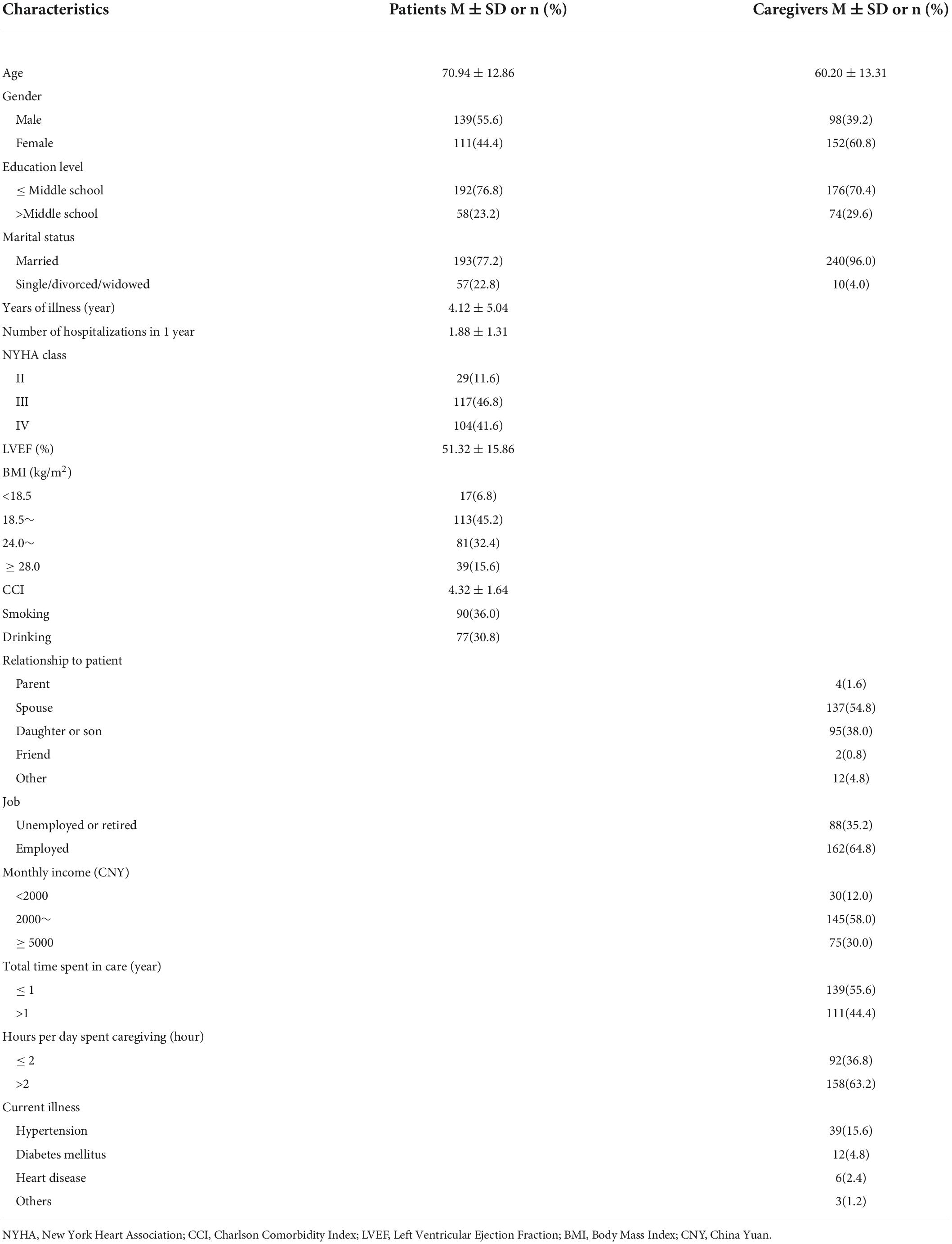
We also collected patients’ demographic information and clinical data (e.g., age, gender, education level, marital status, time of illness, times of hospitalization, New York Heart Association class (NYHA), Charlson Comorbidity Index (CCI), Left Ventricular Ejection Fraction (LVEF), Body Mass Index (BMI), smoking and drinking). Caregivers’ demographic information (age, gender, relationship to patient, education level, marital status, employment, monthly income, total time spent in care, hours per day spent caregiving, current illness) was collected.
Statistical analysis
Microsoft Excel 2019, IBM Statistical Package for Social Sciences (SPSS) version 26.0 and IBM SPSS AMOS version 21.0 were used to analyze the data. Descriptive statistics were used to describe patient-caregiver dyads mutuality and depression scores. Paired-sample t tests were used to compare the scores of each variable between patients and family caregivers. We compared patient-caregiver dyads mutuality and depression scores using radar maps. Radar map is a common graph used for multivariate comparative analysis. In a radar map, each variable has its own numerical axis. These numerical axes have a common center and radiate around this center to form a radar-like image, also like a spider’s web, so it is called radar map or spider’s web (Zhu, 2006). It can clearly reflect the evaluation of the overall development of the individual. Pearson correlation was used to analyze the relationship between patient and caregiver mutuality and depression. We used Amos 21.0 to analyze dyadic data. An APIM was established to analyze the actor-partner effects of patient-caregiver mutuality and depression. The mutuality was taken as independent variable and depression as dependent variable. A separate APIM for each dimension of mutuality was fitted. P < 0.05 was considered to be statistically significant.
Results
Characteristics of patients with chronic heart failure and their caregivers
A total of 250 dyads of patients and their caregivers were included in this study (Table 1). Most patients were male (55.6%) and married (77.2%). The average age was 70.94 + 12.86 years. The average number of years of illness was more than 4 years, and the average number of hospitalizations was more than one time a year. The education level of the patients is low, with only 23.2% receiving education beyond middle school. Most patients were classified as New York Heart Association class III or IV (46.8% or 41.6%). The LVEF (51.32 ± 15.86) and CCI (4.32 ± 1.64) of patients indicated that patient’s condition was poor. Few of patients smoke (36.0%) and drink alcohol (30.8%). Most of the patients (45.2%) had a body mass index in the normal range.
Among caregivers, there were 98 male caregivers (39.2%) and 152 female caregivers (60.8%). The average age was 60.20 + 13.31 years. Most of the caregivers are married (96.0%), and low level of education (70.4%). The most type of dyadic relationship between patient and caregiver is mostly spouse (54.8%). 64.8% of caregivers are employed. Most caregivers have moderate incomes. The majority of the caregivers spent less than one year providing care and more than two hours per day. 15.6% of caregivers had hypertension.
Mutuality and depression scores in patients with chronic heart failure and their caregivers
The Table 2 and the radar map (Supplementary Figure 1) showed that CHF patients total score of mutuality and the scores of mutuality dimensions were higher than those of caregivers. It indicated that better mutuality perceived by patients. Compared with caregivers, CHF patients had significantly higher depression scores. It is also clear from the radar map that the depression of the patients was worse than that of the caregivers.

Table 2. Comparisons of mutuality scale scores and SDS scores between patients and caregivers (n = 250 dyads).
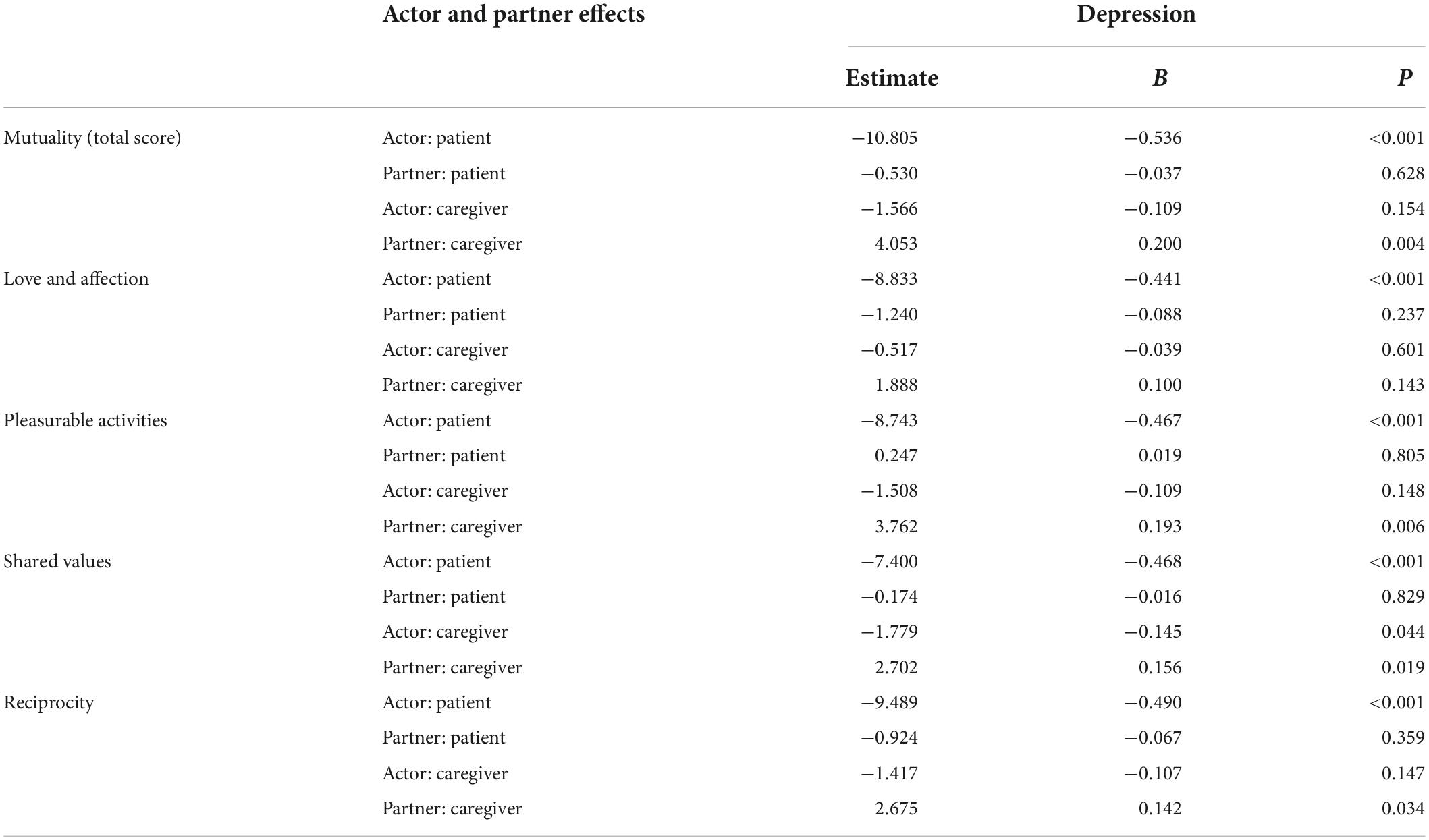
Table 3 shows the relationship between mutuality dimensions and depression. Overall and all dimensions of mutuality were associated with depression. Caregivers’ overall mutuality and some mutuality dimensions were weakly associated with depression. Patients’ overall mutuality and mutuality dimensions were not associated with caregivers’ depression. Caregivers’ “love and affection” was associated with patients’ depression.
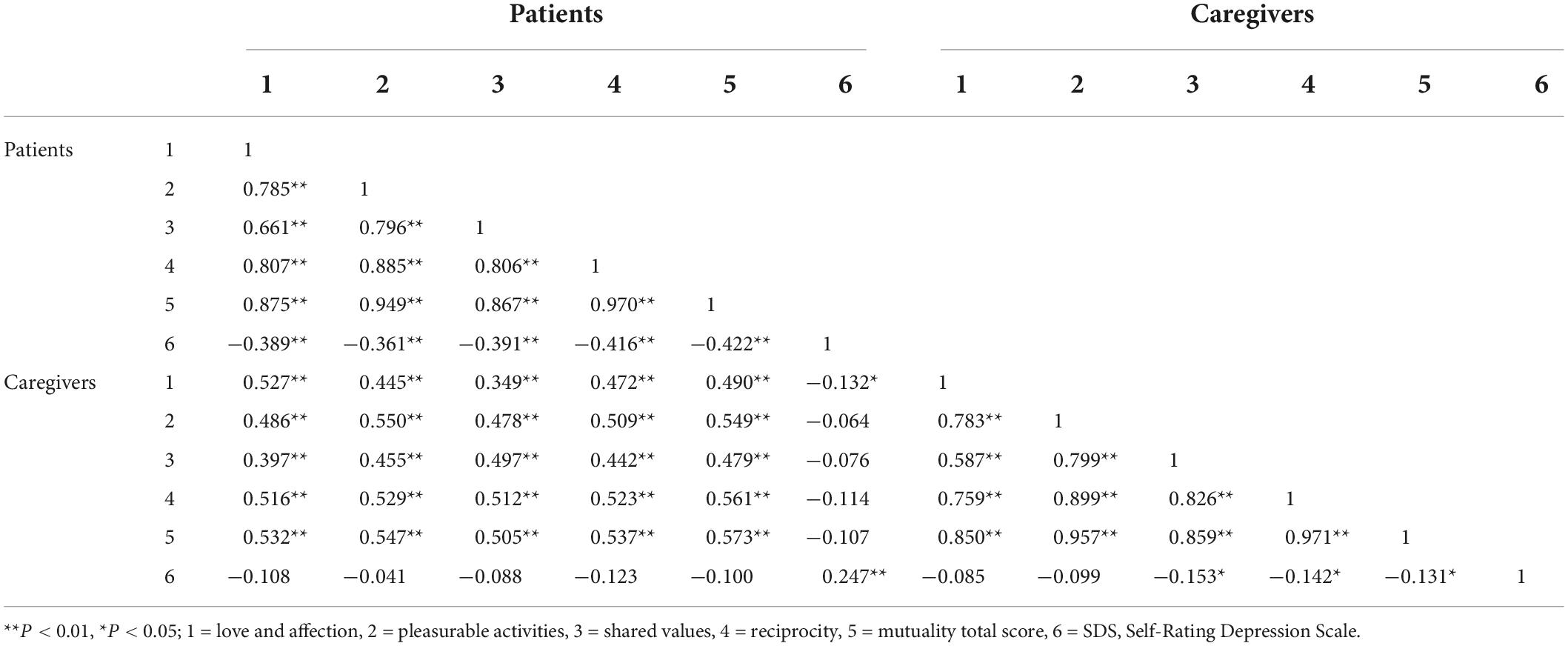
Table 3. Correlations of mutuality scale scores and SDS scores between patients and caregivers (n = 250 dyads).
Actor–partner effects of mutuality on depression
The results (Table 4 and Supplementary Figure 2) showed that there was an actor effect of CHF patients’ mutuality total score on depression (B = −0.536, P<0.001). Caregivers’ mutuality total score had a significant partner effect on patients’ depression (B = 0.200, P = 0.004). However, there were no partner effect of patients’ mutuality total score on caregivers’ depression and no actor effect of caregivers’ mutuality total score on depression.
Table 4 and Supplementary Figure 3 showed the actor-partner effect of mutuality dimensions on depression. We found that patients’ “love and affection” had an actor effect on depression (B = −0.441, P < 0.001). There were an actor effect of patients’ “pleasurable activities” on depression (B = −0.467, P < 0.001) and a partner effect of caregivers’ “pleasurable activities” on patients’ depression (B = 0.193, P = 0.006). Patients’ “shared values” (B = −0.468, P < 0.001) and caregivers’ “shared values” (B = 0.156, P = 0.019) influenced patients’ depression. We also found an actor effect of caregivers’ “shared values” on caregivers’ depression (B = −0.145, P = 0.044). In addition, the lower the patient “reciprocity” score (B = −0.490, P < 0.001) and the higher the caregiver “reciprocity” score (B = 0.142, P = 0.034), the lower the patient’s depression score.
Discussion
The purpose of this study was to evaluate the relationship between depression and mutuality in patients with CHF and their family caregivers. Our main finding was that higher patient mutuality and lower caregiver mutuality were associated with decreased patient depression, but we didn’t find these associations in the caregivers. To our knowledge, this is an earlier study in China to explore the relationship between mutuality and depression in patients with CHF and their caregivers in China using an APIM.
The results showed that mutuality scores of patients and caregivers were 2.91 ± 0.68 and 2.64 ± 0.67. The patient-caregiver mutuality was at a moderate level in our study. The level of mutuality of patients was higher than that of caregivers, which was consistent with the results reported by Hooker et al. (2018), who studied 99 dyads of HF patients and their caregivers. The caregivers’ mutuality score in our study was higher than that of caregivers of stroke (Pan et al., 2017) and pancreatic cancer patients (Zhang et al., 2020). This difference may be due to the severity of stroke and pancreatic cancer, which can affect communication between caregiver and patient and which requires complex and difficult tasks that may affect the caregivers’ mutuality.
Depression is a common psychological symptom of patients with CHF. It leads to adverse problems such as increased level of cardiac function and decreased functional ability of CHF patients (Lossnitzer et al., 2020). The depression scores of patients with chronic heart failure in this study were higher than those of previous studies (Chung et al., 2016; Matsuda et al., 2021). The possible reasons are as follows: (1) In this study, 81.6% of elderly patients with chronic heart failure had higher NYHA class. The complexity of the disease and the high cost of medical treatment led to many patients have negative emotions. (2) Differences in depression evaluation methods adopted by researchers. The survey tool used in this study is the SDS, which has been used to assess emotional states in China for a long time. Some studies have also confirmed that the SDS has high specificity and can accurately reflect patients’ mood disorders (Zhang et al., 2008). Depression also causes burden on caregivers. In this study, we found that patients scored significantly higher for depression than caregivers. An Italian study of 366 patients with HF and their caregivers reported the same result (Dellafiore et al., 2019). Both patients and caregivers are affected by CHF, but patients tend to be much more affected than caregivers. As a result, their emotional health is adversely affected.
In the dyadic analysis, we found that patient mutuality influenced patient depression, which was consistent with Lyons et al. who found that better relationship quality was significantly associated with decreased depressive symptoms for patients (Lyons et al., 2020). More specifically, our study demonstrated that all the 4 dimensions of patients’ mutuality had negative influence on patients’ depression. Mutuality is an important factor in the treatment of patients with CHF. Patients with high level of mutuality are mostly able to actively cope with the disease, constantly adjust their psychological state, and reduce the generation of negative emotions (Peng et al., 2021).
In addition, we also found significant actor effect on caregivers. Caregivers’ “shared values” inversely influenced their depression. In other words, as their “shared values” increased their depression scores decreased. This is an important finding for caregivers because we did not find the effect of caregiver mutuality total scores on their depression. In other studies, mutuality was analyzed as a total score, making it difficult to see small effects. Through the analysis of caregiver mutuality dimensions, we found that “shared values” was an important factor. “Shared values” reflects the convergence of views between the patient and the caregiver on some issues. For caregivers, they hope to reach an agreement with patients when dealing with their disease problems, so as to avoid conflicts and negative emotions (Bouldin Aikens et al., 2019).
We found a partner effect of caregiver mutuality on patient depression. In other words, caregivers’ better mutuality was associated with patients’ greater depression. Specifically, caregiver higher scores in “pleasurable activities,” “shared values,” and “reciprocity” were associated with patient greater depression. The results were unexpected because it showed that caregiver mutuality did not improve patient depression. It’s hard to interpret these results. This may be because the patients’ disease condition in this study is very serious, and caregivers with a high level of mutuality care too much about the patients. Thus, increasing the patients’ disease treatment pressure and negative emotions. The effect of caregiver’s mutuality on the patient’s depression could be different depending on the level of mutuality. However, this relationship needs to be further studied.
To sum up, this study emphasizes the interdependence theory. This theory holds that there is strong interpersonal interaction between dyads with intimate relationship. Individual emotion, cognition or behavior are easily transferred between dyads, and may eventually affect the health outcome of the partner (Wickham and Knee, 2012). Our results also demonstrate the interaction between CHF patients and caregivers.
This study has several advantages and limitations. The study was based on analysis using the APIM, thus the interdependence of dyadic data was well controlled. We used radar maps to compare patient-caregiver dyads variables and it was able to see the difference visually. However, the sample size included in this study was small, and a larger sample is needed to verify our results. Finally, this study only included CHF patients from two hospitals in one city in China, thus the results should be cautiously generalized to other locations.
Conclusion
We assessed the relationship between depression and mutuality in patients with CHF and caregivers in China. The level of mutuality and depression of patients was significantly higher than that of caregivers. Our results highlight the importance of evaluating mutuality in patients and caregivers in clinical settings to improve outcomes for the patient-caregiver dyads.
Relevance for clinical practice
This study determined the relationship between depression and mutuality in patients with chronic heart failure and their family caregivers. The results of this study indicate the importance of evaluating the relationship between patients and caregivers. However, caregiver’s physical and mental health is often ignored by medical staff in clinical settings. In most cases, patients view intimate family caregivers as the most important emotional and support resources in their lives. When the primary family caregiver has negative emotions, they provide less care to the patient than usual. This will lead to a decrease in the patient’s perceived emotions and support. Thus, the assessment of mutuality in patients and caregivers should be strengthened in clinical settings, as it is an important factor in improving the adverse mood of family caregivers.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
TZ was responsible for drafting the manuscript, as well as the acquisition, analysis, and interpretation of data. JQ collected, analyzed, and interpreted the data. HS and MX collected the data. YL provided professional advice and performed much of the editing of the manuscript. All authors read and approved the final manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.928311/full#supplementary-material
Supplementary Figure 1 | Comparisons of mutuality scale scores and SDS scores between patients and caregivers.
Supplementary Figure 2 | Actor and partner effects of CHF patient’s mutuality and caregiver’s mutuality on depression. **P < 0.01; ***P < 0.001.
Supplementary Figure 3 | Actor and partner effects of CHF patient’s mutuality dimensions and caregiver’s mutuality dimensions on depression. *P < 0.05; **P < 0.01; ***P < 0.001.
References
Adelborg, K., Schmidt, M., Sundbøll, J., Pedersen, L., Videbech, P., Bøtker, H. E., et al. (2016). Mortality Risk Among Heart Failure Patients With Depression: A Nationwide Population-Based Cohort Study. J. Am. Heart Assoc. 5:e004137. doi: 10.1161/JAHA.116.004137
Al-Omary, M. S., Davies, A. J., Evans, T. J., Bastian, B., Fletcher, P. J., Attia, J., et al. (2018). Mortality and Readmission Following Hospitalisation for Heart Failure in Australia: A Systematic Review and Meta-Analysis. Heart Lung Circ. 27, 917–927. doi: 10.1016/j.hlc.2018.01.009
Archbold, P. G., Stewart, B. J., Greenlick, M. R., and Harvath, T. (1990). Mutuality and preparedness as predictors of caregiver role strain. Res. Nurs. Health 13, 375–384. doi: 10.1002/nur.4770130605
Benjamin, E. J., Muntner, P., Alonso, A., Bittencourt, M. S., Callaway, C. W., Carson, A. P., et al. (2019). Heart Disease and Stroke Statistics-2019 Update: A Report From the American Heart Association. Circulation 139:e56–e528. doi: 10.1161/CIR.0000000000000659
Bouldin Aikens, J. E., Piette, J. D., and Trivedi, R. B. (2019). Relationship and communication characteristics associated with agreement between heart failure patients and their Carepartners on patient depressive symptoms. Aging Ment. Health 23, 1122–1129. doi: 10.1080/13607863.2018.1481923
Chen, W. W., Gao, R. L., Liu, L. S., Zhu, M. L., Wang, W., Wang, Y. J., et al. (2015). Summary of China Cardiovascular Disease Report 2014. Chin. Circ. J. 30, 617–622. doi: 10.3969/j.issn.1000-3614.2015.07.001
Chinese Association of Cardiology Heart Failure Group. (2018). Heart Failure Professional Committee of Chinese Medical Doctor Association, Editorial Board of Chinese Journal of Cardiovascular Diseases. Guidelines for diagnosis and treatment of heart failure in China 2018. Chin. J. Cardiol. 2, 196–225. doi: 10.3760/cma.j.issn.0253-3758.2018.10.004
Chobufo, M. D., Khan, S., Agbor, V. N., Rahman, E., Foryoung, J. B., Jolayemi, A., et al. (2020). 10-Year trend in the prevalence and predictors of depression among patients with heart failure in the USA from 2007-2016. Int. J. Cardiol. 301, 123–126. doi: 10.1016/j.ijcard.2019.09.028
Chung, M. L., Lennie, T. A., Mudd-Martin, G., Dunbar, S. B., Pressler, S. J., and Moser, D. K. (2016). Depressive symptoms in patients with heart failure negatively affect family caregiver outcomes and quality of life. Eur. J. Cardiovasc. Nur. 15, 30–38. doi: 10.1177/1474515114535329
Clements, L., Frazier, S. K., Moser, D. K., Lennie, T. A., and Chung, M. L. (2020). The Mediator Effects of Depressive Symptoms on the Relationship between Family Functioning and Quality of Life in Caregivers of Patients with Heart Failure. Heart Lung. 49, 737–744. doi: 10.1016/j.hrtlng.2020.08.011
Dellafiore, F., Chung, M. L., Alvaro, R., Durante, A., Colaceci, S., Vellone, E., et al. (2019). The Association Between Mutuality, Anxiety, and Depression in Heart Failure Patient-Caregiver Dyads: An Actor-Partner Interdependence Model Analysis. J. Cardiovasc. Nurs. 34, 465–473. doi: 10.1097/JCN.0000000000000599
Expert Committee of Chinese Heart Failure Center. (2018). China Heart Aging Center Certification Standard. Chin. J. Front. Med. Sci. 10, 1–7. doi: 10.12037/YXQY.2018.08-01
Gong, Y., Wang, P., and Zheng, X. M. (2021). Mediating Effect of Mutuality between Family Resilience and Positive Emotion, Positive Copying Style in Patients with Chronic Heart Failure. Pract. J. Cardiac. Cereb. Pneum. Vasc. Dis. 29, 47–52. doi: 10.12114/j.issn.1008-5971.2021.00.277
Halm, M. A., and Bakas, T. (2007). Factors associated with caregiver depressive symptoms, outcomes, and perceived physical health after coronary artery bypass surgery. J. Cardiovasc. Nurs. 22, 508–515. doi: 10.1097/01.JCN.0000297388.21626.6c
Hooker, S. A., Schmiege, S. J., Trivedi, R. B., Amoyal, N. R., and Bekelman, D. B. (2018). Mutuality and heart failure self-care in patients and their informal caregivers. Eur. J. Cardiovasc. Nurs. 17, 102–113. doi: 10.1177/1474515117730184
Kenny, D. A., and Cook, W. (1999). Partner effects in relationship research: Conceptual issues, analytic difficulties, and illustrations. Pers. Relationsh. 6:433448. doi: 10.1111/j.1475-6811.1999.tb00202.x
Kneeshaw, M. F., Considine, R. M., and Jennings, J. (1999). Mutuality and preparedness of family caregivers for elderly women after bypass surgery. Appl. Nurs. Res. 12, 128–135. doi: 10.1016/s0897-1897(99)80034-2
Li, C., Yuan, J., Huang, X., Zhang, S., Hong, Y., and Zhong, J. (2022). Correlation between depression and intimacy in lung cancer patients and their family caregivers. BMC Palliat Care 21:99. doi: 10.1186/s12904-022-00992-7
Liu, J. Y. (2006). A study on the relationship between family caregivers with dementia and the role of caregiving activities, Ph.D. theses. China: Chang Gung University.
Liu, S. Y., Li, H. F., and Duan, L. J. (2020). Correlation analysis of self-management behavior and hope level in patients with chronic heart failure. Chin. Gen. Pract. Nurs. 18, 92–94. doi: 10.12104/j.issn.1674-4748.2020.01.029
Liu, X. C., Tang, M. Q., Chen, K., Hu, L., and Wang, A. Z. (1995). Comparison of SDS and CES-D in the Evaluation of Depression Symptoms in College Students. Chin. J. Ment. Health 9, 19–20+37.
Lossnitzer, N., Feisst, M., Wild, B., Katus, H. A., Schultz, J. H., Frankenstein, L., et al. (2020). Cross-lagged analyses of the bidirectional relationship between depression and markers of chronic heart failure. Depress Anxiety 37, 898–907. doi: 10.1002/da.23041
Lyons, K. S., and Lee, C. S. (2018). The Theory of Dyadic Illness Management. J. Fam. Nurs. 24, 8–28. doi: 10.1177/1074840717745669
Lyons, K. S., Sadowski, T., and Lee, C. S. (2020). The role of concealment and relationship quality on patient hospitalizations, care strain and depressive symptoms in heart failure dyads. Eur. J. Cardiovasc. Nurs. 19, 118–124. doi: 10.1177/1474515119863791
Matsuda, R., Kohno, T., Kohsaka, S., Shiraishi, Y., Katsumata, Y., Hayashida, K., et al. (2021). Psychological disturbances and their association with sleep disturbances in patients admitted for cardiovascular diseases. PLoS One. 16:e0244484. doi: 10.1371/journal.pone.0244484
Pan, Y., Jones, P. S., and Winslow, B. W. (2017). The Relationship Between Mutuality, Filial Piety, and Depression in Family Caregivers in China. J. Transcult. Nurs. 28, 455–463. doi: 10.1177/1043659616657877
Peng, Y. Y., Sun, G. Z., Wang, J., and Gu, Z. J. (2021). Influence of mutuality between patients with chronic heart failure and family caregivers on their positive emotions and positive coping styles. Chin. J. Mod. Nurs. 27, 846–850. doi: 10.3760/cma.j.cn115682-20200922-05474
Schumacher, K. L., Stewart, B. J., and Archbold, P. G. (2007). Mutuality and preparedness moderate the effects of caregiving demand on cancer family caregiver outcomes. Nurs. Res. 56, 425–433. doi: 10.1097/01.NNR.0000299852.75300.03
Shyu, Y. I., Yang, C. T., Huang, C. C., Kuo, H. C., Chen, S. T., and Hsu, W. C. (2010). Influences of mutuality, preparedness, and balance on caregivers of patients with dementia. J. Nurs. Res. 18, 155–163. doi: 10.1097/JNR.0b013e3181ed5845
The Writing Committee of the Report on Cardiovascular Health and Diseases in China. (2020). Interpretation of Report on Cardiovascular Health and Diseases in China 2019. Chin. J. Card Med. 25, 401–410. doi: 10.3969/j.issn.1007-5410.2020.05.001
Vellone, E., Chung, M. L., Alvaro, R., Paturzo, M., and Dellafiore, F. (2018). The Influence of Mutuality on Self-Care in Heart Failure Patients and Caregivers: A Dyadic Analysis. J. Fam. Nurs. 24, 563–584. doi: 10.1177/1074840718809484
Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., et al. (2020). Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation 141:e139–e596. doi: 10.1161/CIR.0000000000000757
Wickham, R. E., and Knee, C. R. (2012). Interdependence theory and the actor-partner interdependence model: Where theory and method converge. Pers. Soc. Psychol. Rev. 16, 375–393. doi: 10.1177/1088868312447897
Wu, X., Liu, S. T., Zhou, S. J., Li, X. X., and Zhang, L. L. (2020). Impact of intimate relationship between colorectal cancer patients and their primary family caregivers on their quality of life: An analysis based on actor-partner interdependence model. Chin. Gen. Prac. 23, 2120–2125. doi: 10.12114/j.issn.1007-9572.2020.00.203
Zhang, J., Liu, P. P., Lv, R., Zhang, D. L., and Yang, Y. J. (2008). Comparing the Different Self-Rating Scales for Anxiety and Depression Evaluation in the Patients With or Without Heart Failure. Chin. Circ. J. 23, 120–122.
Zhang, X. Q., Wang, M. J., Liu, L. L., and Chen, M. X. (2020). Correlations among mutuality, perceived social support and resilience among main caregivers of pancreatic cancer patients after surgery. Chin. J. Mod. Nurs. 26, 1865–1870. doi: 10.3760/cma.j.cn115682-20191205-04456
Keywords: actor-partner interdependence model, chronic heart failure, depression, dyads, mutuality
Citation: Zhou T, Qu J, Sun H, Xue M and Liu Y (2022) Relationship between mutuality and depression in patients with chronic heart failure and caregivers in China: An actor-partner interdependence model analysis. Front. Psychol. 13:928311. doi: 10.3389/fpsyg.2022.928311
Received: 25 April 2022; Accepted: 12 August 2022;
Published: 08 September 2022.
Edited by:
M. Graça Pereira, University of Minho, PortugalCopyright © 2022 Zhou, Qu, Sun, Xue and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yongbing Liu, bingbing19950806@163.com
 Ting Zhou
Ting Zhou Jiling Qu
Jiling Qu Huiping Sun
Huiping Sun Mengxin Xue
Mengxin Xue Yongbing Liu
Yongbing Liu