- 1Guangdong Mental Health Center, Guangdong Academy of Medical Sciences, Guangdong Provincial People's Hospital, Guangzhou, China
- 2Department of Public Health, Medical College, Qinghai University, Xining, China
- 3The National Clinical Research Center for Mental Disorders and Beijing Key Laboratory of Mental Disorders, Beijing Anding Hospital and the Advanced Innovation Center for Human Brain Protection, Capital Medical University, Beijing, China
- 4Department of Psychiatry, The Melbourne Clinic and St Vincent's Hospital, University of Melbourne, Richmond, VIC, Australia
- 5Department of Business Administration, Hong Kong Shue Yan University, Hong Kong, China
- 6The Jockey Club School of Public Health and Primary Care, Chinese University of Hong Kong, Hong Kong, China
- 7Unit of Psychiatry, Department of Public Health and Medicinal Administration, Institute of Translational Medicine, Faculty of Health Sciences, University of Macau, Macao, China
- 8Centre for Cognitive and Brain Sciences, University of Macau, Macao, China
- 9Institute of Advanced Studies in Humanities and Social Sciences, University of Macau, Macao, China
Objective: Depressive symptoms (depression hereafter) is common in older adults, and closely associated with environmental factors. This study compared the prevalence of depression in older adults living in high-altitude and low-altitude regions, and their association with quality of life (QOL).
Method: A total of 632 older nursing home residents were included, with 425 participants living in low-altitude and 207 participants living in high-altitude regions. Depression and QOL were assessed using standardized instruments.
Results: The prevalence of depression was 26.9% (95% CI: 23.43–30.37%) in the whole sample of older nursing home residents, with 11.1% (95% CI: 8.01–14.05%) in those living in low-altitude and 59.4% (95% CI: 52.68–66.17%) in those living in high-altitude regions. Multiple logistic regression analysis revealed that living in low-altitude region (P < 0.001, OR = 0.07, 95% CI: 0.04–0.12) was associated with lower risk of depression, while perception of poor health status (P < 0.001, OR = 3.86, 95% CI: 1.98–7.54) and having insomnia (P < 0.001, OR = 4.76, 95% CI: 2.99–7.56) were associated with higher risk of depression. QOL was significantly lower in physical (F(1,632) = 35.421, P < 0.001), psychological (F(1,632) = 20.777, P < 0.001), social (F(1,632) = 8.169, P < 0.001) and environmental domains (F(1,632) = 11.861, P < 0.001) in those with depression.
Conclusion: Depression was common in older nursing home residents especially those living in the high-altitude region. Considering the negative impact of depression on QOL and functional outcomes, routine screening and timely treatment of depression should be implemented in this population.
Introduction
Due to biological and psychosocial risk factors such as physical disorders, retirement, bereavement and social isolation, depressive symptoms (depression hereafter) are common in older adults (1, 2), which could lead to a range of negative health outcomes including poor daily functioning, cognitive decline and high risk of suicidality (3–5). The epidemiology of the depression in older adults has been widely studied, with prevalence ranging between 6.35% (6) and 60.3% (7). A meta-analysis revealed that the prevalence of depression was 23.6% among older adults in China (8). The discrepancy in depression prevalence between studies could be partly due to the use of different measures of depression; for example, the Center for Epidemiologic Studies Depression Scale (CES-D) (9), Montgomery–Åsberg Depression Rating Scale (MADRS) (10), Hamilton Rating Scale for Depression (HAMD) (11), and Patients' Health Questionnaire (PHQ-9) (12) were used in different studies.
Environmental factors such as altitude are strongly linked with psychiatric problems (13). For instance, a study conducted in the USA found a positive correlation between increased risk of suicide and high-altitude (14, 15). Living in high-altitude areas is associated with hypoxia (16), lower atmospheric pressure and altered pharmacokinetics of certain psychotropic medications (17), all of which could increase the risk of depression (18). In addition, insufficient health resources, lack of community services, and underdeveloped economic status in many high-altitude areas could be associated with depression (14). However, a common limitation of previous studies of depression in high altitude has been the lack of comparison with those living in low-altitude areas.
Hence, we compared the prevalence of depression in older adults living in low-altitude and high-altitude regions, and explore their association with demographic and clinical characteristics, as well as quality of life (QOL), which is a widely used health outcome in both clinical practice and research (19).
Methods
Study Setting and Participants
This cross-sectional comparative study was conducted between September 1st and November 31st, 2019 in China. Participants were recruited from three public nursing homes in Xi'ning, a city in Qinghai province with an average altitude of 2,300 m (high-altitude area), and a large-scale nursing home in Guangzhou, a city in Guangdong province, with an average altitude of 10 m (low-altitude area). Older adults in the selected nursing homes were consecutively invited to participate in this study and those who met the following inclusion criteria were included: (1) age of 60 years or above; (2) Chinese ethnicity and fluent in Chinese languages including Mandarin or Cantonese; (3) have ability to communicate and complete the assessment adequately. Those with obvious cognitive decline such as dementia and intellectual disability based on a review of health records were excluded. The study protocol was approved by the IRB of University of the Macau and written informed consent was obtained from all participants.
Assessment Tools and Evaluation
Basic socio-demographic and clinical characteristics of participants were collected including age, gender, education level, marital status, religion, perceived financial status, medical conditions, and family history of psychiatric disorders. The Chinese version of the self-reported 9-item Patient Health Questionnaire (PHQ-9) was used to evaluate the severity of depression within the past 2 weeks (20, 21). The PHQ-9 is the most commonly used, validated and efficient instrument for screening depression (22), which was developed based on the Diagnostic and Statistical Manual of Mental Disorders-Four Edition (DSM-IV Edition) (23),with satisfactory reliability and validity in Chinese populations including older adults (20). The PHQ-9 consists of nine items, including little interest in doing things, feeling holpless, sleeping disturbance, feeling tired, appetite suiation, feeling bad about self, trouble concentrating on things, moving or speaking slowly, and thought or hurt yourself. Each item is scored from 0 (not at all) to 3 (nearly every day) with a total score between 0 and 27. A higher PHQ-9 total score indicates more severe depression (24), with a total score of ≥5 as “having depression,” and ≥10 as “having moderate to severe depression” (25). Participants' QOL was measured using the World Health Organization Quality of Life brief version (WHOQOL-BREF), which includes 26 items covering four dimensions (physical, psychological, social, and environmental domains). A higher score indicates higher QOL. Following previous studies (26–28), three standardized questions were used to evaluate insomnia symptoms (insomnia hereafter) in the past week (e.g., “Did you have difficulties in initiating sleep?”; “Did you ever have difficulties in maintaining sleep?” and “Did you wake up in the midnight and having difficulties in sleeping again?”), with each question having three options (0 = never, 1 = sometime, and 2 = often). If a participant answered “often” to any of the questions, then he/she was defined as “having insomnia” (28).
Statistical Analysis
The study data were analyzed using SPSS 24.0 for Windows. Comparison of the basic demographic and clinical characteristics between older adults living in high- and low-altitude regions, and comparison between depression and non-depression groups in the whole sample with respect to socio-demographic and clinical characteristics were performed by independent sample t-test, Mann-Whitney U test, and chi-square test, as appropriate. The PHQ-9 total scores between low and high altitude areas were compared using analysis of covariance (ANCOVA), after controlling for confounding effects of variables with significant group differences in univariate analyses. In addition, QOL between depression and non-depression groups in the whole sample was also compared using ANCOVA, after controlling for the potentially confounding effects of variables with significant group differences in univariate analyses. Multiple logistic regression analysis with the “enter” method was performed to determine the independent relationships between depression and socio-demographic and clinical characteristics. Depression was entered as dependent variable, while variables that significantly differed between the depression and non-depression groups in the univariate analyses were independent variables. The level of significance was set at 0.05 (two-tailed).
Result
Of a total of 657 older nursing home residents invited to participate in the study, 632 (425 in low-altitude and 207 in high-altitude regions) met the study criteria and completed the assessments during the study period, giving a participation rate of 96.2%. The prevalence of overall depression (PHQ total score of ≥5) in the whole sample was 26.9% (95% CI: 23.43–30.37%), with 59.4% (95% CI: 52.68–66.17%) in those living in high-altitude and 11.1% (95% CI: 8.01–14.05%) living in low-altitude regions. In contrast, the prevalence of moderate to severe depression (PHQ total score ≥10) was 8.07% (95% CI: 5.94–10.20%) in the whole sample, with 16.91% (95% CI: 11.76–22.06%) living in high-altitude and 3.76% (95% CI: 1.95–5.58%) living in low-altitude areas. The mean total score of PHQ-9 was 3.05 (SD = 3.91).
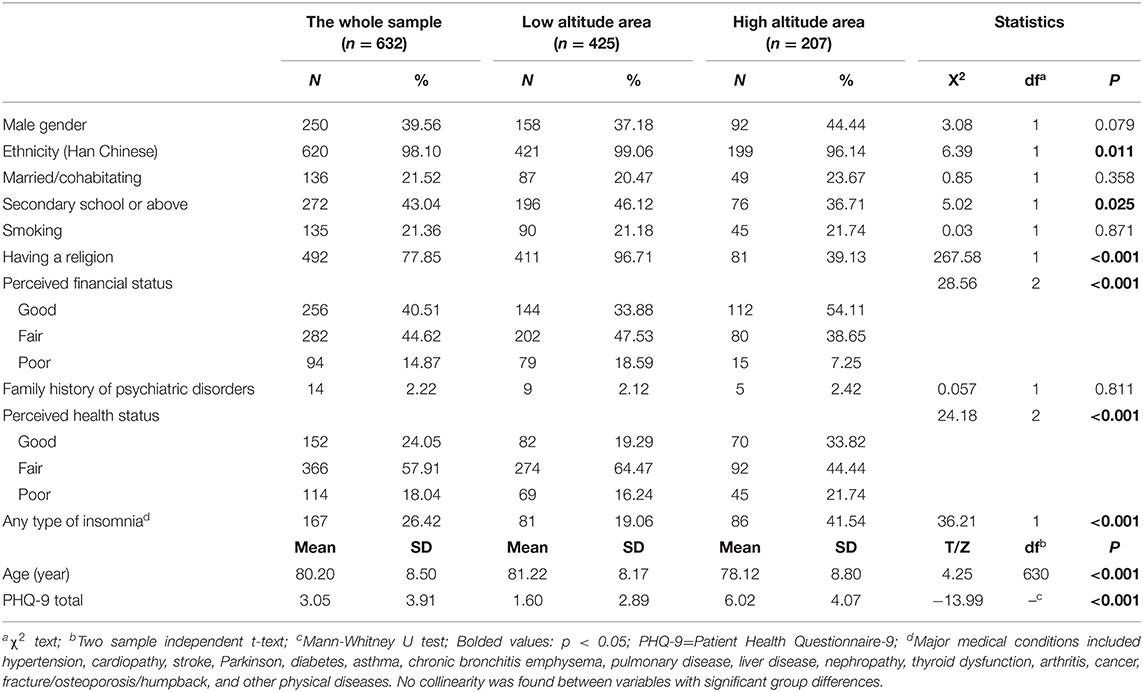
Table 1 shows the demographic and clinical characteristic of the whole sample and also separately by altitude region. There were significant differences between low-altitude and high-altitude regions in terms of age, ethnicity, education level, religion, perceived financial status, perceived health status, number of medical conditions and depressive symptoms. After controlling for these variables with group differences, older adults living in high altitude area reported more severe depression [F(1,632) = 42.849, P < 0.001].
Table 2 presents the comparisons between older adults with depression and those without depression with respect to basic demographic and clinical characteristics, and QOL. Compared to those without depression, participants with depression had lower education level, no religion, poor health status, were living in higher-altitude region and more likely to have major medical conditions. After controlling for covariates, QOL was significantly lower in physical (F(1,632) =35.421, P < 0.001), psychological (F(1,632) = 20.777, P < 0.001), social (F(1,632) = 8.169, P < 0.001) and environmental (F(1,632) = 11.861, P < 0.001) domains in those with depression. Multiple logistic regression analysis revealed that living in low-altitude region (P < 0.001, OR = 0.07, 95% CI: 0.04–0.12) was associated with lower risk of depression, while perceived poor health status (P < 0.001, OR = 3.86, 95% CI: 1.98–7.54) and having insomnia (P < 0.001, OR = 4.76, 95% CI: 2.99–7.56) were associated with higher risk of depression (Table 3).
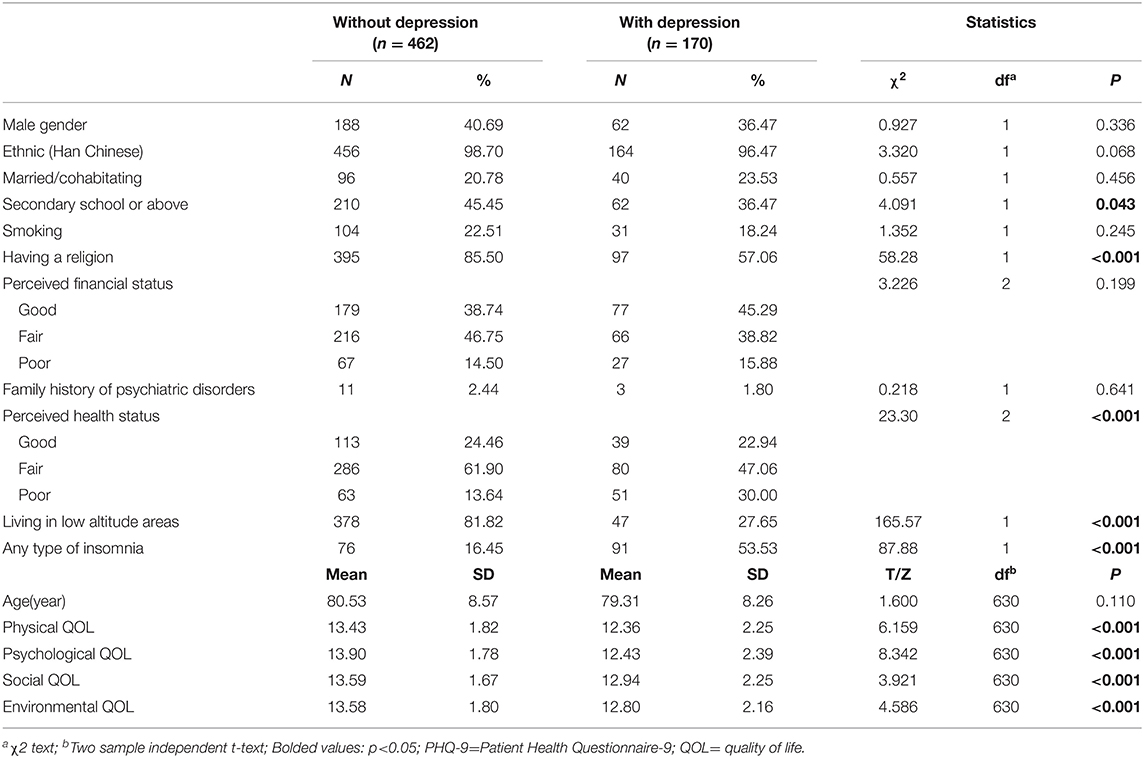
Table 2. Comparison between older adults with and without depression in terms of basic demographic and clinical characteristics in the whole sample.
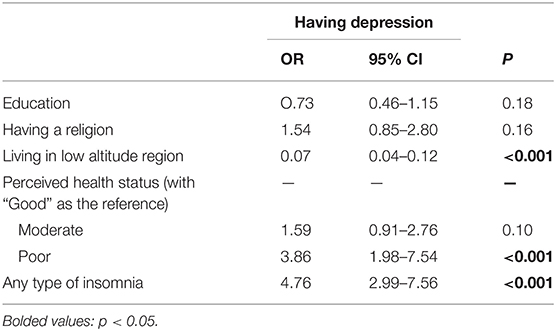
Table 3. Socio-demographic correlates of depression in older adults (by multiple logistic regression analysis).
Discussion
To the best of our knowledge, this was the first study that compared the prevalence of depression in older nursing home residents living in low-altitude and high-altitude regions. Depression was common (26.9%) in older nursing home residents in China, which is similar to the findings in Brazil (23.5%) (29), but higher than those living in nursing homes in Japan (11.9%) (30) and Thailand (18.5%) (31). However, it should be noted that due to different sampling methods, demographic and clinical characteristics, and measures of depression as well as their cutoff values, direct comparisons should be made with caution (8).
The prevalence of depression in older adults living in high-altitude (59.4%) was almost five times higher compared to those living in low-altitude regions (11.1%) in this study, which is consistent with the findings (52.3%) of a previous study conducted in Yushu, another city in Qinghai province (32, 33). The significant difference in depression prevalence between high- and low-altitude regions remained even after controlling for covariates. This could be due to socioeconomic reasons. Generally, the high-altitude region in Qinghai province is one of the most economically under-developed regions in China (34). Poor social welfare, low pension after retirement, and insufficient primary health services in the community are factors associated with an increase the risk of depression in older adults (32, 35). In contrast, Guangzhou (situated in the low-altitude region) is one of the most economically developed areas, with the best social and health service systems in China (34, 36). Second, environmental factors in high-altitude areas, such as hypoxia and lower atmospheric pressure can commonly lead to sleep problems like high apnea/hypopnea index, increased frequency of arousals and changed sleep structure (37–39). In addition, long-term hypoxia in high-altitude areas could influence neural activity through certain neurotransmitters such as dopamine and serotonin in the monoamine system, which in turn could increase the risk of psychiatric problems (32). These factors are also associated with higher risk of depression (40, 41).
In this study apart from living in high-attitude region, perceived poor health status and insomnia were independently associated with higher risk of depression, which is consistent with previous findings (42, 43). Older adults with poor health status particularly severe medical disorders often suffer from physical and psychological problems such as low energy, low appetite, frustration, which may lead to depression. The association between insomnia and depression is bidirectional. On the one hand, common sleep problems including insomnia associated with hypoxia in high-altitude areas can increase the likelihood of depression. On the other hand, depression can also lead to sleep disturbances (43, 44).
Older adults with depression frequently experienced physical distress, impaired functional ability, cognitive decline and higher risk of suicidality (3–5). QOL is deemed to be related to the interaction between protective factors (e.g., better social support) and distressing factors (e.g., poor mental and physical status) (45), hence depressed older adults are likely to have a lower QOL, which is consistent with the our study that QOL was significantly lower in physical, psychological, social and environmental domains in those with depression, although the group differences in QOL ratings were not large.
The strengths of this study were the inclusion of study participants from both high- and low- altitude regions as well as the use of QOL measures. However, several limitations should be noted. First, due to the cross-sectional study design, the causality between depression and other variables could not be examined. Second, as only one public nursing home in low-altitude (Guangzhou) and three public nursing homes in high-altitude regions (Qinghai) were included, the findings could not be generalized to those living in other settings. Finally, older adults with severe cognitive impairment were excluded, which could lead to selection bias to an uncertain extent.
In conclusion, depression was common in older nursing home residents particularly those living in high-altitude region. Considering the negative impact of depression on QOL and functional outcomes, routine screening and timely treatment of depression should be implemented in this subpopulation. In view of the rapid urbanization in China, traditional family structures have gradually changed. Many young family members do not live with their parents/grandparents (46, 47), which results in increasing number of older adults being placed in nursing homes. Therefore, increased mental health care resources should be allocated by the central and local governments to the nursing homes and relevant community mental health services in high-altitude regions to address the needs of this growing sub-population.
Data Availability Statement
The IRB of University of Macau that approved the study prohibits the authors from making the research data set publicly available. Readers and all interested researchers may contact Dr. Yu-Tao Xiang (Email address: xyutly@gmail.com) for details. Dr. Yu-Tao Xiang could apply to the IRB of University of Macau for the release of the data.
Ethics Statement
The study protocol was approved by the IRB of University of the Macau and written informed consent was obtained from all participants.
Author Contributions
Y-TX: study design. FW, SL, QZ, XC, and DZ: collection, analyses, and interpretation of data. FW and Y-TX: drafting of the manuscript. CN: critical revision of the manuscript. All the authors approved the final version for publication.
Funding
The study was supported by the Special Fund for Science and Technology of Guangdong Provincial People's Hospital (Grant no. 2017zh02), the National Science and Technology Major Project for investigational new drug (Grant no. 2018ZX09201-014), the Beijing Municipal Science & Technology Commission (Grant no. Z181100001518005), and the University of Macau (Grant no. MYRG2019-00066-FHS).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank all the subjects and staff involved in this study.
References
1. Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand. (2004) 109:21–7. doi: 10.1111/j.1600-0047.2004.00325.x
2. Yaka E, Keskinoglu P, Ucku R, Yener GG, Tunca Z. Prevalence and risk factors of depression among community dwelling elderly. Arch Gerontol Geriatr. (2014) 59:150–4. doi: 10.1016/j.archger.2014.03.014
3. Holtfreter K, Reisig MD, Turanovic JJ. Depression and infrequent participation in social activities among older adults: the moderating role of high-quality familial ties. Aging Ment Health. (2017) 21:379–88. doi: 10.1080/13607863.2015.1099036
4. Wu C-S, Yu S-H, Lee C-Y, Tseng H-Y, Chiu Y-F, Hsiung CA. Prevalence of and risk factors for minor and major depression among community-dwelling older adults in Taiwan. Int Psychogeriatr. (2017) 29:1113–21. doi: 10.1017/S1041610217000199
5. Waugh A. Depression and older people. Nurs Older People. (2006) 18:27–30. doi: 10.7748/nop.18.8.27.s17
6. Chen J, Zhang L, Gao L. Depressive symptom and its influence factor in urban old adults in Wuhan. Chin J Gerontol. (2007) 27:275–6. doi: 10.3969/j.issn.1005-9202.2007.03.032
7. Jia L, Zhuang H, Wang X, Liu F, Chen B, Lin Y. Depression status of the elderly and its relationship with quality of life in community of Fuzhou city. Chin J Geriatr. (2011) 30:970–3. doi: 10.3760/cma.j.issn.0254-9026.2011.11.024
8. Li D, Zhang DJ, Shao JJ, Qi XD, Tian L. A meta-analysis of the prevalence of depressive symptoms in Chinese older adults. Arch Gerontol Geriatr. (2014) 58:1–9. doi: 10.1016/j.archger.2013.07.016
9. Lewinsohn PM, Seeley JR, Roberts RE, Allen NB. Center for epidemiologic studies depression scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging. (1997) 12:277. doi: 10.1037/0882-7974.12.2.277
10. Yohannes AM, Baldwin RC, Connolly MJ. Depression and anxiety in elderly outpatients with chronic obstructive pulmonary disease: prevalence, and validation of the BASDEC screening questionnaire. Int J Geriatr Psychiatry. (2000) 15:1090–6.
11. Lyness JM, King DA, Cox C, Yoediono Z, Caine ED. The importance of subsyndromal depression in older primary care patients: prevalence and associated functional disability. J Am Geriatr Soc. (1999) 47:647–52. doi: 10.1111/j.1532-5415.1999.tb01584.x
12. Kocalevent R-D, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
13. Kious BA-O, Bakian AA-O, Zhao J, Mickey BA-O, Guille CA-O, Renshaw P, et al. Altitude and risk of depression and anxiety: findings from the intern health study. Int Rev Psychiatry. (2019) 31:637–45. doi: 10.1080/09540261.2019.1586324
14. Ishikawa M, Yamanaka G, Nakajima S, Suwa K, Matsuda A, Nakaoka T, et al. Association between high altitude and depression in the Himalayas and the Andes. Nihon Ronen Igakkai Zasshi. (2013) 50:330–4. doi: 10.3143/geriatrics.50.330
15. Reno E, Brown TL, Betz ME, Allen MH, Hoffecker L, Reitinger J, et al. Suicide and high altitude: an integrative review. High Alt Med Biol. (2018) 19:99–108. doi: 10.1089/ham.2016.0131
16. Ishikawa M, Yamanaka G, Yamamoto N, Nakaoka T, Okumiya K, Matsubayashi K, et al. Depression and altitude: cross-sectional community-based study among elderly high-altitude residents in the himalayan regions. Cult Med Psychiatry. (2016) 40:1–11. doi: 10.1007/s11013-015-9462-7
17. Arancibia A, Paulos C, Chavez J, Ritschel WA. Pharmacokinetics of lithium in healthy volunteers after exposure to high altitude. Int J Clin Pharmacol Ther. (2003) 41:200–6. doi: 10.5414/CPP41200
18. Kious BM, Fau KD, Renshaw PF, Renshaw PF. Living high and feeling low: altitude, suicide, and depression. Harv Rev Psychiatry. (2018) 26:43–56. doi: 10.1097/HRP.0000000000000158
19. Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E, et al. A systematic review of quality of life research in medicine and health sciences. Qual Life Res. (2019) 28:2641–50. doi: 10.1007/s11136-019-02214-9
20. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
21. Leung DYP, Mak YW, Leung SF, Chiang VCL, Loke AY. Measurement invariances of the PHQ-9 across gender and age groups in Chinese adolescents. Asia Pac Psychiatry. (2020) 12:e12381. doi: 10.1111/appy.12381
22. Levis B, Benedetti A, Thombs BD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
23. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Text Revision (DMS-IV-TR). Washington, DC: American Psychiatric Association (2000).
24. Maroufizadeh S, Omani-Samani R, Almasi-Hashiani A, Amini P, Sepidarkish M. The reliability and validity of the Patient Health Questionnaire-9 (PHQ-9) and PHQ-2 in patients with infertility. Reprod Health. (2019) 16:137. doi: 10.1186/s12978-019-0802-x
25. Kroenke K, Spitzer RL, Williams JB, Löwe B. The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen Hosp Psychiatry. (2010) 32:345–59. doi: 10.1016/j.genhosppsych.2010.03.006
26. Nogueira B, Li L, Meng LR, Ungvari GS, Forester BP, Chiu HFK, et al. Prevalence of Sleep disturbances and their associations with demographic and clinical characteristics and quality of life in older adults in macao. Perspect Psychiatr Care. (2018) 54:46–53. doi: 10.1111/ppc.12199
27. Zheng W, Luo XN, Li HY, Ke XY, Dai Q, Zhang CJ, et al. Prevalence of insomnia symptoms and their associated factors in patients treated in outpatient clinics of four general hospitals in Guangzhou, China. BMC Psychiatry. (2018) 18:232. doi: 10.1186/s12888-018-1808-6
28. Liu X, Zhou H. Sleep duration, insomnia and behavioral problems among Chinese adolescents. Psychiatry Res. (2002) 111:75–85. doi: 10.1016/S0165-1781(02)00131-2
29. Corrêa VP, Confortin SC, d'Orsi E, de Sá-Junior AR, de Oliveira C, Schneider IJC. Depressive symptoms as an independent risk factor for mortality. Braz J Psychiatry. (2020). doi: 10.1590/1516-4446-2019-0749
30. Haseda MA-O, Kondo NA-O, Ashida TA-OX, Tani YA-O, Takagi D, Kondo K. Community social capital, built environment, and income-based inequality in depressive symptoms among older people in japan: an ecological study from the JAGES project. J Epidemiol. (2018) 28:108–16. doi: 10.2188/jea.JE20160216
31. Charoensakulchai SA-O, Usawachoke S, Kongbangpor W, Thanavirun P, Mitsiriswat A, Pinijnai O, et al. Prevalence and associated factors influencing depression in older adults living in rural Thailand: a cross-sectional study. Geriatr Gerontol Int. (2019) 19:1248–53. doi: 10.1111/ggi.13804
32. Wang J, Zhou Y, Liang Y, Liu Z. A large sample survey of tibetan people on the qinghai-tibet plateau: current situation of depression and risk factors. Int J Environ Res Public Health. (2019) 17:289. doi: 10.3390/ijerph17010289
33. Liu S, Chow IHI, Lu LA-O, Ren YM, Yang HL, Jian SY, et al. Comparison of sleep disturbances between older nursing home residents in high- and low-altitude areas. J Geriatr Psychiatry Neurol. (2019) 33:1–7. doi: 10.1177/0891988719892335
34. China's Provincial GDP Rankings. China's Provincial GDP Rankings (2020). Available online at: https://blogcsdnnet/weixin_42137700/article/details/113512318?utm_medium=distributepc_relevant_bbs_downnone-task-blog-baidujs-1nonecase&depth_1-utm_source=distributepc_relevant_bbs_downnone-task-blog-baidujs-1nonecase (accessed February 1, 2021).
35. Rashid A, Mohd R. Poor social support as a risk factor for antenatal depressive symptoms among women attending public antennal clinics in Penang, Malaysia. Reprod Health. (2017) 14:144. doi: 10.1186/s12978-017-0404-4
36. Chen H, Liu Y, Li Z, Xue D. Urbanization, economic development and health: evidence from China's labor-force dynamic survey. Int J Equity Health. (2017) 16:207. doi: 10.1186/s12939-017-0705-9
37. Guan W, Ga Q, Li R, Bai ZZ, Wuren T, Wang J, et al. Sleep disturbances in long-term immigrants with chronic mountain sickness: a comparison with healthy immigrants at high altitude. Respir Physiol Neurobiol. (2015) 206:4–10. doi: 10.1016/j.resp.2014.11.007
38. Bloch KE, Buenzli JC, Latshang TD, Ulrich S. Sleep at high altitude: guesses and facts. J Appl Physiol. (2015) 119:1466–80. doi: 10.1152/japplphysiol.00448.2015
39. Sakamoto R, Okumiya K, Norboo T, Tsering N, Yamaguchi T, Nose M, et al. Sleep quality among elderly high-altitude dwellers in Ladakh. Psychiatry Res. (2017) 249:51–7. doi: 10.1016/j.psychres.2016.12.043
40. Matte DL, Pizzichini MM, Hoepers AT, Diaz AP, Karloh M, Dias M, et al. Prevalence of depression in COPD: a systematic review and meta-analysis of controlled studies. Respir Med. (2016) 117:154–61. doi: 10.1016/j.rmed.2016.06.006
41. Mukandala G, Tynan R, Lanigan S, O'Connor JJ. The effects of hypoxia and inflammation on synaptic signaling in the CNS. Brain Sci. (2016) 6:6. doi: 10.3390/brainsci6010006
42. Li L, Wu C, Gan Y, Qu X, Lu Z. Insomnia and the risk of depression: a meta-analysis of prospective cohort studies. BMC Psychiatry. (2016) 16:375. doi: 10.1186/s12888-016-1075-3
43. Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. (2019) 23:2324–32. doi: 10.1111/jcmm.14170
44. Mason BL, Davidov A, Minhajuddin A, Trivedi MH. Focusing on insomnia symptoms to better understand depression: A STAR*D report. J Affect Disord. (2020) 260:183–6. doi: 10.1016/j.jad.2019.08.094
45. Hatoum HT, Kong SX, Kania CM, Wong JM, Mendelson WB. Insomnia, health-related quality of life and healthcare resource consumption. Pharmacoeconomics. (1998) 14:629–37. doi: 10.2165/00019053-199814060-00004
46. Dong X, Wong BO, Yang C, Zhang F, Xu F, Zhao L, et al. Factors associated with willingness to enter care homes for the elderly and pre-elderly in west of China. Medicine. (2020) 99:e23140. doi: 10.1097/MD.0000000000023140
Keywords: older adults, depression, quality of life, high-altitude area, nursing homes
Citation: Wang F, Liu S, Zhang Q, Ng CH, Cui X, Zhang D and Xiang Y-T (2021) Prevalence of Depression in Older Nursing Home Residents in High and Low Altitude Regions: A Comparative Study. Front. Psychiatry 12:669234. doi: 10.3389/fpsyt.2021.669234
Received: 18 February 2021; Accepted: 07 May 2021;
Published: 22 June 2021.
Edited by:
Christos Theleritis, National and Kapodistrian University of Athens, GreeceReviewed by:
Evangelos C. Fradelos, University of Thessaly, GreeceYiyang Yuan, University of Massachusetts Medical School, United States
Copyright © 2021 Wang, Liu, Zhang, Ng, Cui, Zhang and Xiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu-Tao Xiang, xyutly@gmail.com
†These authors have contributed equally to this work
 Fei Wang
Fei Wang Shou Liu
Shou Liu Qinge Zhang3†
Qinge Zhang3† Chee H. Ng
Chee H. Ng Dexing Zhang
Dexing Zhang Yu-Tao Xiang
Yu-Tao Xiang