- 1Sackler Faculty of Medicine, Tel Aviv University, Tel Aviv, Israel
- 2The Chaim Sheba Medical Center, Ramat Gan, Israel
- 3School of Psychological Sciences, Tel Aviv University, Tel Aviv, Israel
- 4Department of Psychology, Bar-Ilan University, Ramat Gan, Israel
Objective: To identify COVID-19 work-related stressors and experiences associated with sleep difficulties in HCW, and to assess the role of depression and traumatic stress in this association.
Methods: A cross-sectional study of HCW using self-report questionnaires, during the first peak of the pandemic in Israel (April 2020), conducted in a large tertiary medical center in Israel. Study population included 189 physicians and nurses working in designated COVID-19 wards and a comparison group of 643 HCW. Mean age of the total sample was 41.7 ± 11.1, 67% were female, 42.1% physicians, with overall mean number of years of professional experience 14.2 ± 20. The exposure was working in COVID-19 wards and related specific stressors and negative experiences. Primary outcome measurement was the Insomnia Severity Index (ISI). Secondary outcomes included the Primary Care-Post Traumatic Stress Disorder Screen (PC-PTSD-5); the Patient Health Questionnaire-9 (PHQ-9) for depression; the anxiety module of the Patient-Reported Outcomes Measurement Information System (PROMIS); Pandemic-Related Stress Factors (PRSF) and witnessing patient suffering and death.
Results: Compared with non-COVID-19 HCW, COVID-19 HCW were more likely to be male (41.3% vs. 30.7%) and younger (36.91 ± 8.81 vs. 43.14 ± 11.35 years). COVID-19 HCW reported higher prevalence of sleep difficulties: 63% vs. 50.7% in the non-COVID group (OR 1.62, 95% CI 1.15–2.29, p = 0.006), mostly difficulty maintaining sleep: 26.5% vs. 18.5% (OR 1.65, 95% CI 1.11–2.44, p = 0.012). Negative COVID-19 work-related experiences, specifically witnessing patient physical suffering and death, partially explained the association. Although past psychological problems and current depression and PTSD were associated with difficulty maintaining sleep, the main association remained robust also after controlling for those conditions in the full model.
Conclusion and Relevance: COVID-19 frontline HCW were more likely to report sleep difficulties, mainly difficulty maintaining sleep, as compared with non-COVID-19 HCW working at the same hospital. Negative patient-care related experiences likely mediated the increased probability for those difficulties. Future research is needed to elucidate the long-term trajectories of sleep difficulties among HCW during large scale outbreaks, and to identify risk factors for their persistence.
Introduction
The COVID-19 pandemic continues to challenge health care workers, as a new COVID variants keep emerging. Working at the frontline of this global pandemic is highly stressful and can significantly impact various aspects of daily life, including sleep quality and quantity (1). Recently, studies from several countries have shown high prevalence of insomnia and of sleep difficulties among hospital medical staff involved in the pandemic, especially among female staff and those with psychological symptoms and with lower educational attainment (2–6).
The association between stressful workplace experiences and poor sleep quality, independent of home-related stress, was previously reported (7). Sleep difficulties were found to be associated with poorer cognitive performance (8, 9), increased numbers of occupational accidents and injuries (10, 11) and car crashes (12, 13). Impaired cognitive and motor skills were found among hospital residents, even with acute, short-standing sleep loss (14). Sleep deprivation was found to negatively impacts surgeons’ technical skills, with obvious implications for patient safety (15), and in the longer term, it was associated with neurological dysfunction and even death (16). In addition, sleep deprivation was found to predict a wide variety of mental disorders (17), including increased risk for stress (18), depression (19), suicidality (20, 21), and also psychotic experiences (22). Furthermore, during stressful events, short sleep was associated with diminished coping with stress (23), increased susceptibility for posttraumatic stress disorder (PTSD) (24–27), as well as for anxiety and hypomania (28).
Although previous research on frontline COVID-19 health care workers (HCW) found high prevalence of sleep difficulties, detailed data on the nature of those difficulties and on associated risk factors are still limited. Furthermore, it is unclear whether sleep difficulties are an independent outcome among COVID-19 HCW or merely a manifestation of other mental health outcomes, such as depression and PTSD. We set to compare the frequency of sleep difficulties among COVID-19 and non-COVID-19 HCW during the first peak of the pandemic in Israel, to identify factors associated with those difficulties, and to investigate whether they occur independent of PTSD and depression. We aim to explore the association between factors related to work at COVID-19 wards and reported sleep difficulties. More specifically, we ask whether negative experiences that are more prevalent among COVID-19 HCW play a role as intermediates in that association.
Materials and Methods
We conducted a single-center, cross-sectional study among physicians and nurses working at the Sheba Medical Center, a large tertiary medical center in central Israel. The study was conducted between April 19–23, 2020. During this period the total number of confirmed COVID-19 cases in Israel peaked from 13,319 (April 19) to 14,511 (April 23).
This study followed the standards and ethics of the American Association for Public Opinion Research reporting guidelines (29) and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines (30). The protocol was approved by the Institutional Review Board of the Sheba Medical Center. Participation in the study was solely voluntary. All participants signed an electronic consent form. The data collected did not include personal identifiers (e.g., name, home address, phone number or email).
Participants
As part of the preparation for the surge in COVID-19 confirmed cases in Israel, specialized COVID-19 care wards were set up and isolated from other care areas in the hospital. Designated teams were allocated for COVID-19 containment wards, as well as two intensive care units, a designated emergency department, five inpatient wards and a psychiatry ward were assembled for the expected COVID-19 patients, totaling almost 400 specialized beds. We aimed at oversampling HCW working in COVID-19 wards (31). A total of 189 HCW from designated COVID-19 departments and 643 non-designated COVID-19 ward HCW (comparison group) responded to the survey, a total of 828 HCW. Sample flow across COVID-19 and non-COVID-19 teams is presented in Supplementary Figure 1.
Study Measures
The participants completed a self-administered anonymous questionnaire digitally through a secured digital platform (Qualtrics). The questionnaire included information on current ward (COVID-19 containment wards or regular wards), sociodemographic characteristics, general and mental health items, and a question about having to go into quarantine (yes/no).
Sleep difficulties were measured with the validated Hebrew version of the Insomnia Severity Index (ISI) (32, 33). Response options of the ISI questions were collapsed into dichotomous values (yes/no) for each of the three ISI items.
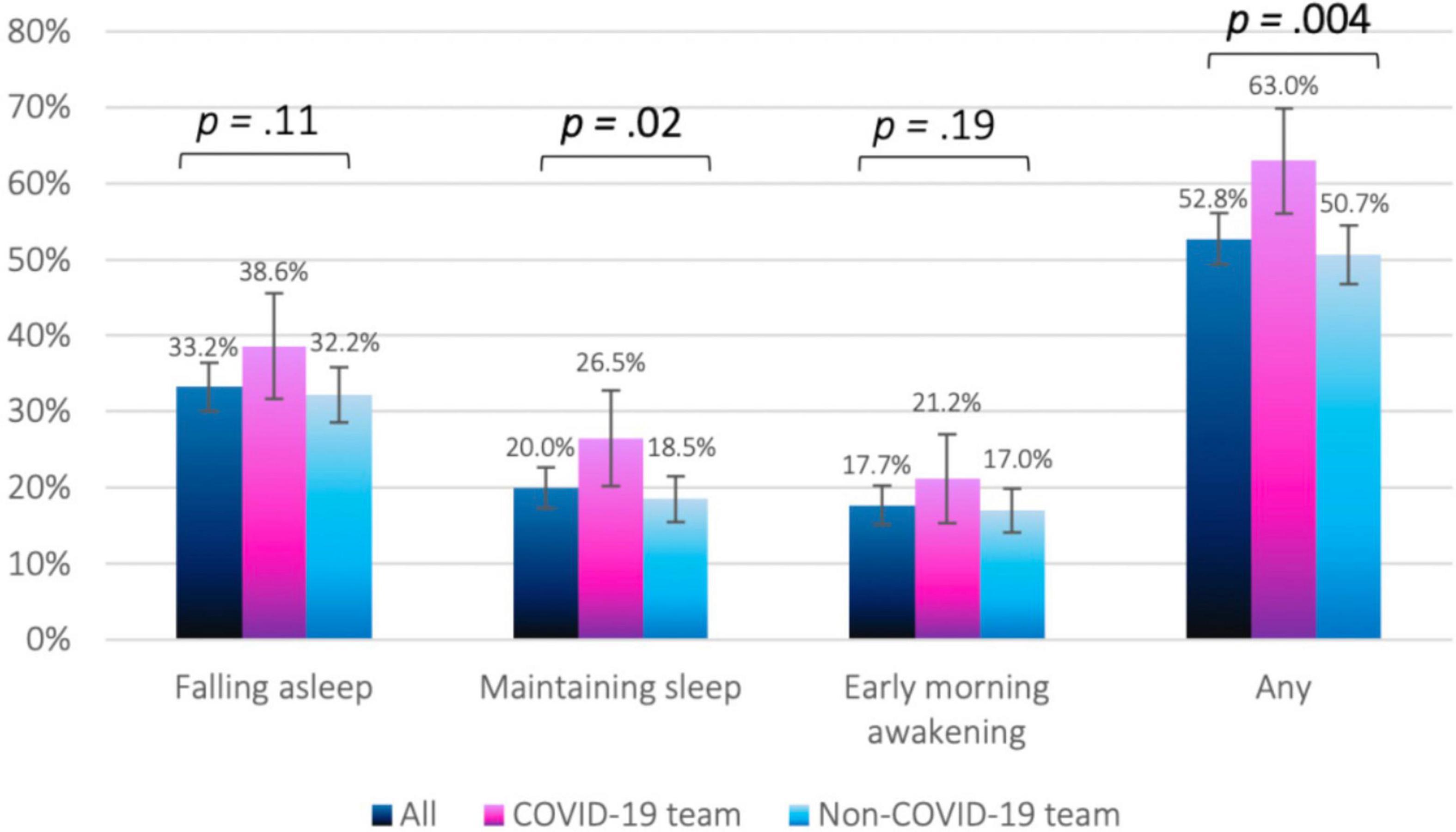
The prevalence of having at least one form of sleep difficulty was significantly higher among COVID-19 vs. non-COVID-19 HCW (63% and 50.7%, respectively, p = 0.004). Specifically, COVID-19 HCW were more likely to experience difficulty maintaining sleep (26.5% and 18.5%, respectively, p = 0.02) as presented in Figure 1.
Traumatic stress during the past month was assessed with the validated Hebrew version of the Primary Care PTSD Screen for DSM-5 (PC-PTSD-5) (34). The PC-PTSD-5 has a score range of 0-5, and we set a cutoff of 3 to define traumatic stress symptoms (35). Participants were asked to respond about their traumatic symptoms specifically in relation to the COVID-19 pandemic.
Depression was assessed with the Hebrew version of the well-validated Patient Health Questionnaire-9 (PHQ-9) (36). The PHQ-9 has a score range of 0–27, and a score of ≥10 was used to identify probable depression in the current study (37).
Anxiety among HCW was assessed by means of the 8-item Hebrew version of the National institution of Mental Health (NIMH) Patient-Reported Outcomes Measurement Information System (PROMIS) anxiety module (38–41). PROMIS has an established coding system validated by the NIMH, with standardized “T” scores ranging between 36.3–82.7 (“PROMIS® Scoring Manuals.,” n.d.). The cutoff point for probable anxiety was set at T ≥62.3, considered as equivalent to the GAD-7 standard cutoff score for moderate anxiety (=10) (40).
Pandemic-related stress factors (PRSF) were measured with an inventory compiled from questions which were proved to be pertinent in research carried out during the SARS and N1H1 pandemics (42–44). A 4-point Likert-type scale was used for scoring the items (from 0 = never to 3 = always). Questions concerning negative experiences included exposure to patients’ physical and mental suffering, the number of patient deaths witnessed over the past month (none, one, more than one) (45), and the self-perceived physical health question from the 12-item Medical Outcomes Study (MOS) Short-Form Health Status Survey (SF-12) (Hebrew version) (poor, fair, good, very good, excellent) (46).
Statistical Analysis
Descriptive statistics were used to describe the sample. We used chi-square tests to compare sociodemographic characteristics, sleep difficulties, prevalence of specific traumatic stress symptoms, probable depression (PHQ-9 score ≥10), probable PTSD (PC-PTSD-5 score ≥3) and probable anxiety (PROMIS score ≥62.3) between COVID-19 and non-COVID-19 HCW. T-tests were used to compare PHQ-9 and PROMIS anxiety module mean scores between study teams. We recoded ordinal variables with multiple categories (e.g., PRSF items, exposure to patient suffering) as categorical, with 1 and 0 representing high and low categories, respectively. Missing values in the PROMIS Anxiety module and the PHQ-9 questionnaire were imputed by the group mean score (47). Logistic regression was used to compare the likelihood of sleep difficulties among COVID-19 and non-COVID-19 wards. Multiple logistic models were used to assess potential mediators and confounders. Adjusted ORs and 95% CIs were computed, with non-COVID-19 team as the reference group.
Next, we conducted a three-step hierarchical logistic regression, to explore the role of potential confounders and mediators in the association between working at COVID-19 wards and sleep difficulties. Covariates were included based on the following criteria: (1) basic sociodemographic characteristics (age, sex, profession and professional experience); (2) theoretical and empirical framework developed based on research carried out during previous and current pandemics (witnessing patient suffering and death, and past psychological problems); and (3) variables that did not have considerable effect on the association between study group and sleep difficulties (PRSF and financial concerns) were not included in the hierarchical model. As model fitting via logistic regression is sensitive to collinearities among independent variables, we decontaminated the strongly correlated witnessing patient physical suffering and witnessing patient death variables from common variance by regressing them out of each other and including their standardized residuals in the final model (48). This method does not affect model’s predictability, and therefore R2 remains unchanged compared with the non-residualized model but reduces multicollinearity and extracts the unique variance explained by each predictor, resulting in purified more powerful coefficients.
A three-step hierarchical logistic regression was used to test whether probable depression and PTSD, either alone or combined, accounted for the increased likelihood of sleep difficulties among COVID-19 HCW. Alpha was set at 0.05, and all tests were 2-tailed. Statistical analyses were conducted with IBM SPSS V25 software.
Results
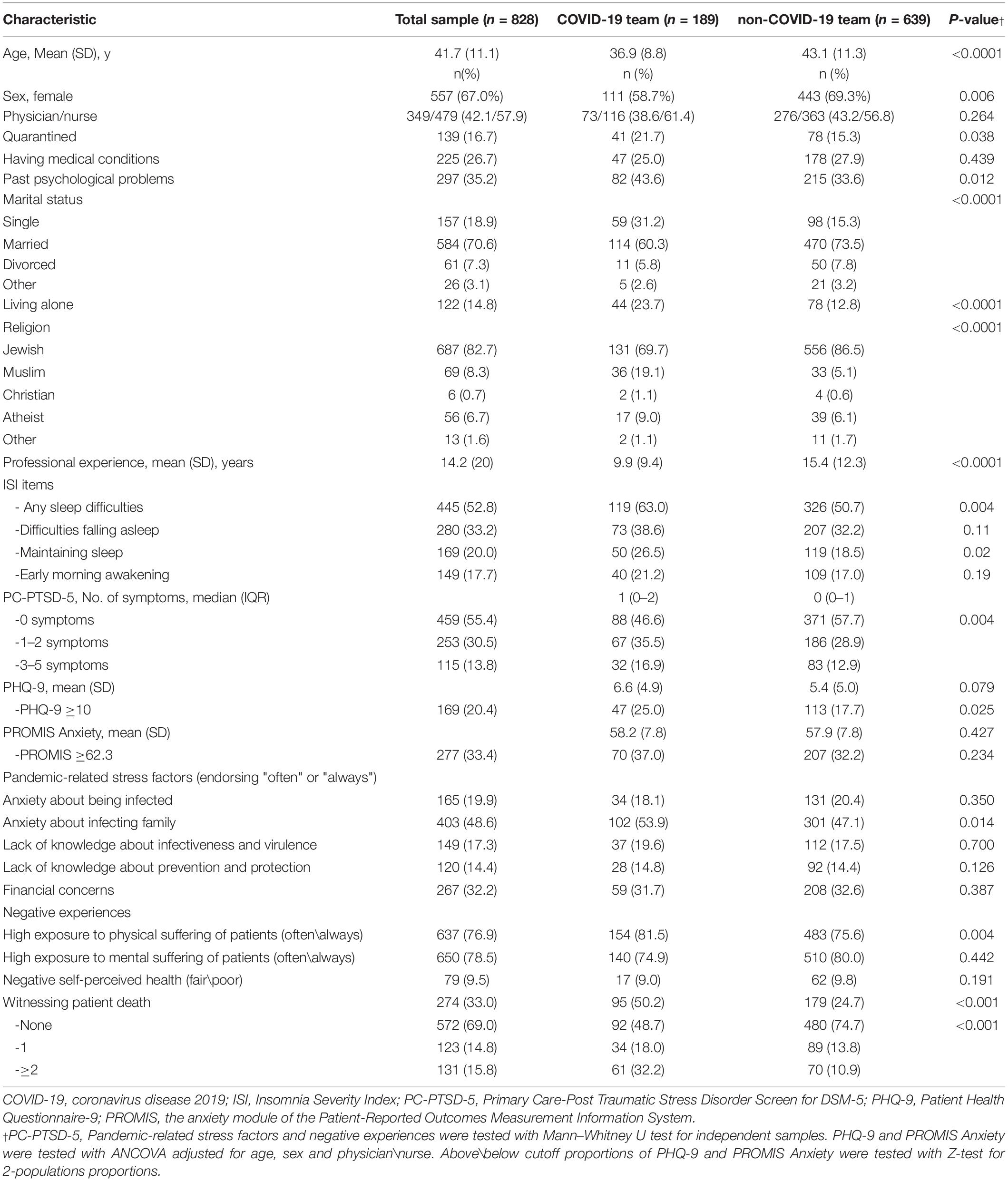
The analytic sample included a total of 828 HCW (42.1% physician, 57.9% nurses), of whom 189 worked in the COVID-19 wards (42.3% of total COVID-19 team members in the hospital) and 639 in the non-COVID-19 wards (20.1% of total non-COVID-19 teams). Detailed description of the study sample are reported elsewhere (49). The main characteristics and work-related experiences of the study groups are presented in Table 1.
COVID-19 HCW were more likely to experience any sleep difficulties (OR 1.62, 95% CI 1.15–2.29, p = 0.006). Difficulty maintaining sleep emerged as the strongest and most significant finding (OR 1.65, 95% CI 1.11–2.44, p = 0.012). These associations persisted in the multivariate models that adjusted for age, sex, and profession (model 1), and for PRSF items (anxiety about being infected, anxiety about infecting family, lack of knowledge about infectiveness and virulence, and lack of knowledge about prevention and protection) (model 2). The effect of financial concerns on the associations was negligible. The association between working in COVID-19 wards and difficulty maintaining sleep was attenuated when negative experiences were added to the model as shown in Table 2.
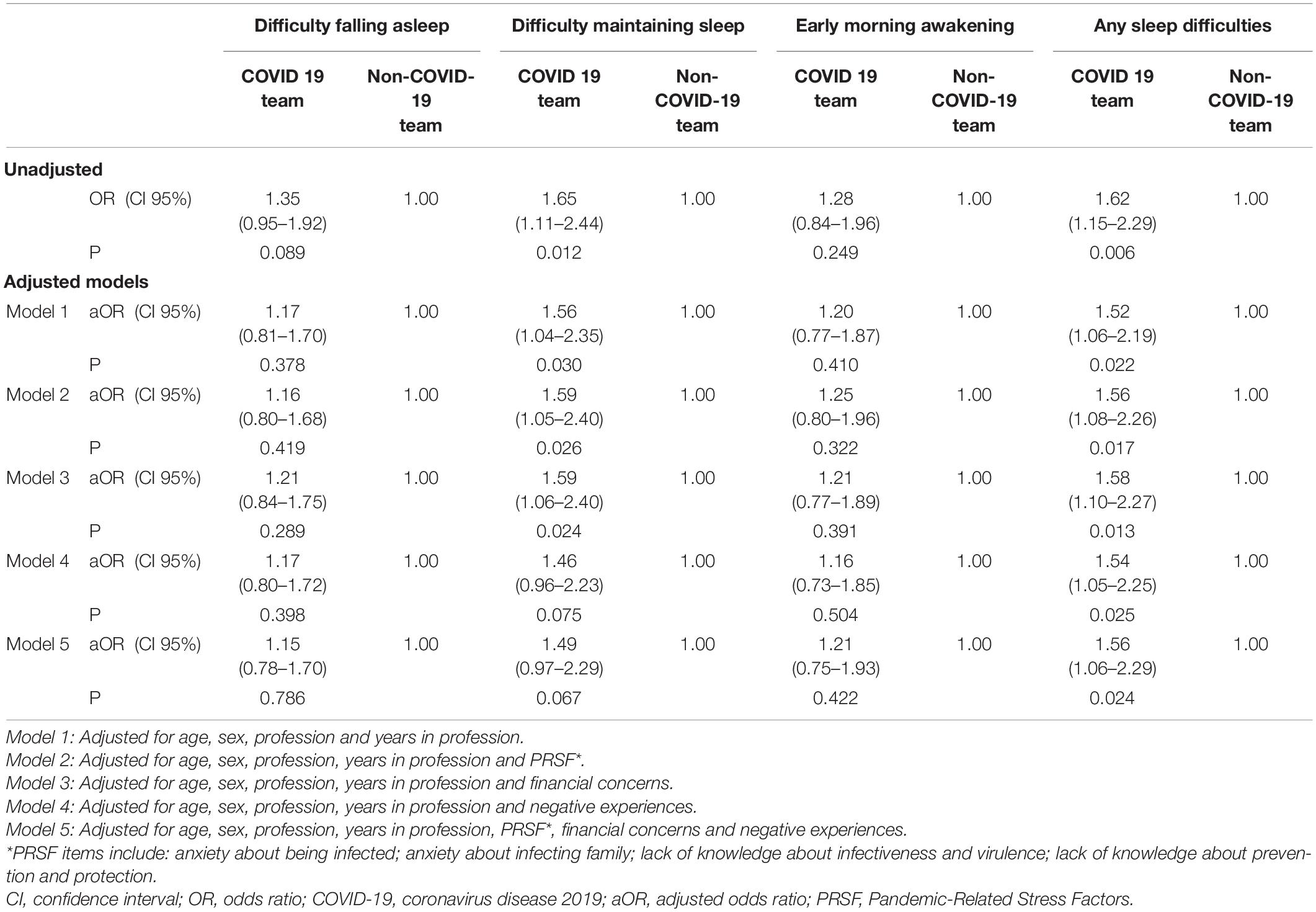
Table 2. Crude and adjusted odds ratios for sleep difficulties among COVID-19 vs. non- COVID-19 teams.
Next, we focused on exploring the association between difficulty maintaining sleep and variables selected according to the aforementioned criteria, using three-step hierarchical logistic regression model, presented in Table 3. We found that the main effect of work in COVID-19 ward on difficulty maintaining sleep was considerably attenuated after adjusting for witnessing patient physical suffering and death were added to the model. Adding self-reported past psychological problems to the model, which was found to be associated with difficulty maintaining sleep, further attenuated the association in the full model (OR 1.35, 95% CI 0.89–2.06, p = 0.162).
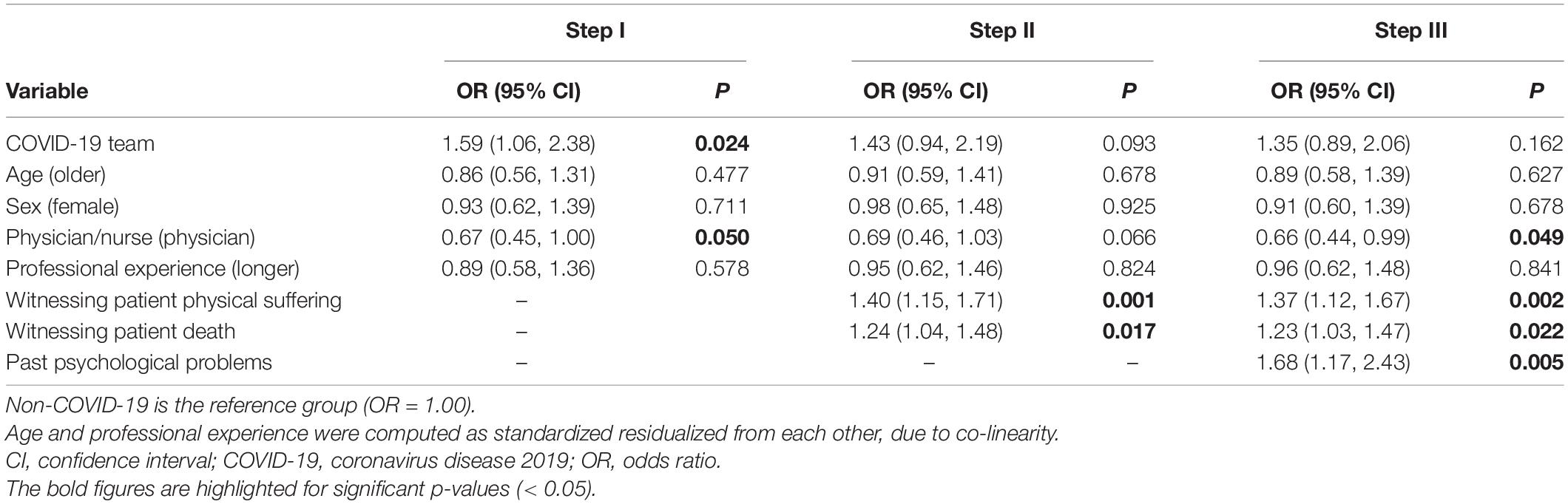
Table 3. Factors associated with likelihood of difficulty maintaining sleep in COVID-19 and non-COVID-19 teams.
Lastly, although difficulty maintaining sleep was associated with both probable depression and PTSD (OR 3.36 and 3.12, respectively), those conditions did not account for the increased likelihood of difficulty maintaining sleep among COVID-19 HCW as shown in Table 4.
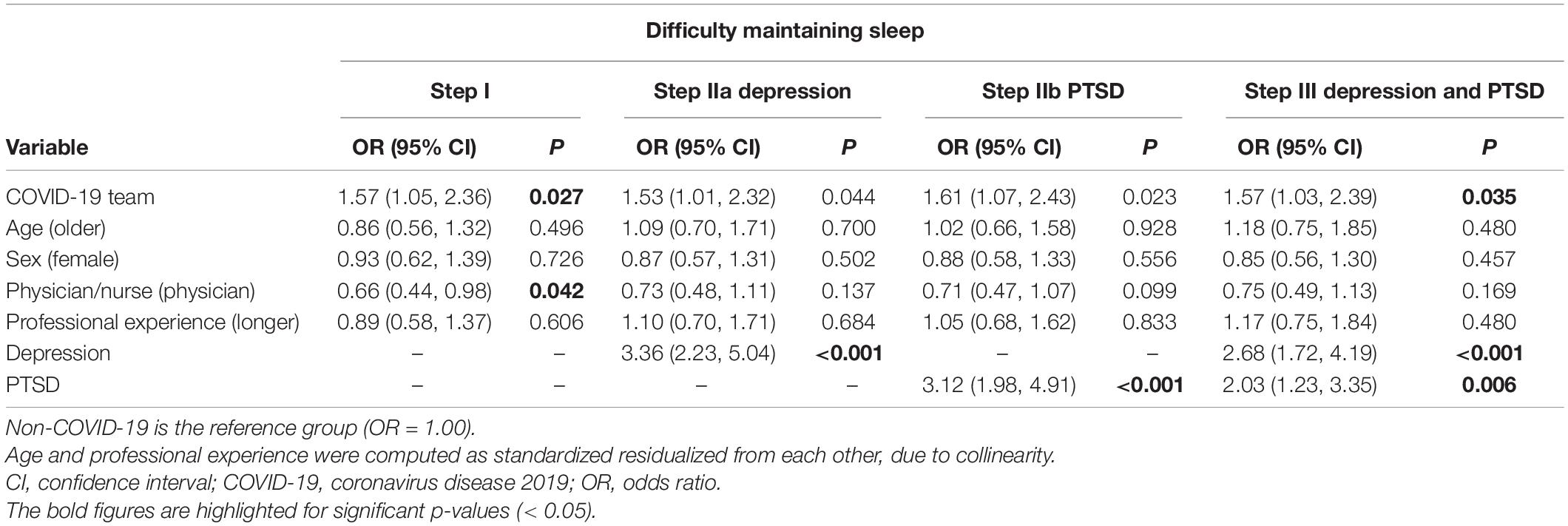
Table 4. The association between difficulty maintaining sleep and PTSD and depression in COVID-19 and non-COVID-19 healthcare workers.
Discussion
The main finding that emerged from our data was that COVID-19 HCW experienced higher prevalence of sleep difficulties, specifically difficulty maintaining sleep, compared with non-COVID-19 HCW in a large tertiary medical center in central Israel, during the first peak of COVID-19 pandemic. Although sleep difficulties among frontline HCW were previously reported in the current and previous pandemics (2, 3, 50–57), there are no published data on the role of mediating factors that might explain the association between work in COVID-19 wards and sleep difficulties.
We found that negative experiences, most notably witnessing physical suffering by the patient and patient death, accounted partially for the association between working in COVID-19 ward and difficulty maintaining sleep. The role of those two negative experiences as intermediates persisted also after adjusting for the potential confounding effect of past psychological problems. The mediation effect was unique for those negative experiences and was not found for other variables related to the pandemic, such as PRSF and financial concerns. It is plausible that witnessing patient suffering and death induced distressing dreams (nightmares), which interrupted REM sleep (58). Interestingly, the association between working in COVID-19 ward and difficulty maintaining sleep in our sample could not be attributed to current probable depression or PTSD, despite the fact that sleep difficulties are common symptoms in both disorders.
A plausible contributor to the increase in sleep difficulties among frontline HCW during the pandemic is workplace violence, shown in other studies to have increased during the pandemic (59–61).
The main strength of our study is that both study group and comparison group (COVID-19 team and non-COVID-19 team, respectably) were sampled from the same underlying cohort of physicians and nurses, sharing occupational, organizational and hospital leadership features. Additional strengths of our study include: (1) the ‘real-time’ nature of our data, as it were collected during the first peak of the pandemic in Israel, and not retrospectively, thus reducing the likelihood of recall bias; (2) availability of objective information on study group allocation; (3) study outcomes were measured by means of well-validated instruments; and (4) a very low proportion of missing data.
Our findings have several potential implications for the frontline workforce during a pandemic. First, screening for sleep difficulties among COVID-19 HCW, especially those exposed to negative experiences, could prompt targeted early intervention, especially in light of reported beneficial impact of fatigue training for improving personnel and patient safety, and reducing stress and burnout among HCW (62). Second, achieving trauma-induced sleep disorder normalization was shown to reduced risk of PTSD (63, 64), frequently reported among COVID-19 HCW (41, 65, 66). Additionally, integrating occupational mental health programs at healthcare settings, was shown to help alleviating pandemic-related sleep difficulties (67).
Limitations
Our study has several limitations. First, conclusion about directionality is limited by the cross-sectional study design. However, it is unlikely that assignment of HCW to COVID-19 wards was conditioned on history of sleep difficulties. Second, the higher prevalence of sleep difficulties among the COVID-19 HCW might be partially explained by the higher workload in COVID-19 wards, especially considering the reduced work volume in the non-COVID-19 wards during that time. Third, the study was conducted in a single medical center in Israel during the first wave of the pandemic, and therefore the generalizability of our findings might be limited. Fourth, non-responders had slightly different sociodemographic characteristics. Fifth, data were collected by means of self-report questionnaires rather than clinical interviews.
Conclusion
We found that COVID-19 frontline HCW were more likely to report sleep difficulties, mainly difficulty maintaining sleep, as compared with HCW working in regular wards at the same hospital, and that negative patient-care related experiences likely mediated the increased likelihood for those difficulties. Future research is needed to elucidate the long-term trajectories of sleep difficulties among HCW caring for COVID-19 patients, and to identify antecedents and risk factors for persistence of those difficulties.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author Contributions
RC, MM, RG, NH-P, DG, IP: conceiving and designing the study. MM, NH-P, and IP: data collection. NH-P: statistical analyses. RC, RG, NH-P, IH-O, RK, RC, YK, DG, and IP: data interpretation. RC and RG: writing the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
Supported by grants from Foundation Dora and the Binational Science Foundation (Grant No. 2017369).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2022.838825/full#supplementary-material
Supplementary Figure 1 | Flow diagram for study participants.
References
1. Chirico F, Ferrari G, Nucera G, Szarpak Ł, Ilesanmi O. Prevalence of anxiety, depression, burnout syndrome, and mental health disorders among healthcare workers during the COVID-19 pandemic: a rapid umbrella review of systematic reviews. J Health Soc Sci. (2021) 6:209–20.
2. Zhang C, Yang L, Liu S, Ma S, Wang Y, Cai Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
3. Wu K, Wei X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med Sci Monit Basic Res. (2020) 26:e924085. doi: 10.12659/MSMBR.924085
4. Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Global Health. (2020) 16:92. doi: 10.1186/s12992-020-00620-0
5. Stewart NH, Koza A, Dhaon S, Shoushtari C, Martinez M, Arora VM. Sleep disturbances in frontline health care workers during the COVID-19 pandemic: social media survey study. J Med Internet Res. (2021) 23:e27331. doi: 10.2196/27331
6. Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. (2021) 17:299–313. doi: 10.5664/jcsm.8930
7. Burgard SA, Ailshire JA. Putting work to bed: stressful experiences on the job and sleep quality. J Health Soc Behav. (2009) 50:476–92. doi: 10.1177/002214650905000407
8. Wardle-Pinkston S, Slavish DC, Taylor DJ. Insomnia and cognitive performance: a systematic review and meta-analysis. Sleep Med Rev. (2019) 48:101205. doi: 10.1016/j.smrv.2019.07.008
9. Lee H-J, Kim L, Suh K-Y. Cognitive deterioration and changes of P300 during total sleep deprivation. Psychiatry Clin Neurosci. (2003) 57:490–6. doi: 10.1046/j.1440-1819.2003.01153.x
10. Uehli K, Mehta AJ, Miedinger D, Hug K, Schindler C, Holsboer-Trachsler E, et al. Sleep problems and work injuries: a systematic review and meta-analysis. Sleep Med Rev. (2014) 18:61–73. doi: 10.1016/j.smrv.2013.01.004
11. Swanson LM, Arnedt JT, Rosekind MR, Belenky G, Balkin TJ, Drake C. Sleep disorders and work performance: findings from the 2008 National sleep foundation sleep in America poll. J Sleep Res. (2011) 20:487–94. doi: 10.1111/j.1365-2869.2010.00890.x
12. Terán-Santos J, Jiménez-Gómez A, Cordero-Guevara J. The association between sleep apnea and the risk of traffic accidents. cooperative group burgos-santander. N Engl J Med. (1999) 340:847–51. doi: 10.1056/NEJM199903183401104
13. Connor J, Whitlock G, Norton R, Jackson R. The role of driver sleepiness in car crashes: a systematic review of epidemiological studies. Accid Anal Prev. (2001) 33:31–41. doi: 10.1016/s0001-4575(00)00013-0
14. Mansukhani MP, Kolla BP, Surani S, Varon J, Ramar K. Sleep deprivation in resident physicians, work hour limitations, and related outcomes: a systematic review of the literature. Postgrad Med. (2012) 124:241–9. doi: 10.3810/pgm.2012.07.2583
15. Whelehan DF, McCarrick CA, Ridgway PF. A systematic review of sleep deprivation and technical skill in surgery. Surgeon. (2020) 18:375–84. doi: 10.1016/j.surge.2020.01.004
16. Lewis LD. The interconnected causes and consequences of sleep in the brain. Science. (2021) 374:564–8. doi: 10.1126/science.abi8375
17. Hertenstein E, Feige B, Gmeiner T, Kienzler C, Spiegelhalder K, Johann A, et al. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
18. Grandner MA, Patel NP, Gehrman PR, Perlis ML, Pack AI. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. Sleep Med Rev. (2010) 14:239–47. doi: 10.1016/j.smrv.2009.08.001
19. Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: a meta-analysis of prospective studies. Depress Anxiety. (2015) 32:664–70. doi: 10.1002/da.22386
20. Pigeon WR, Pinquart M, Conner K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J Clin Psychiatry. (2012) 73:e1160–7. doi: 10.4088/JCP.11r07586
21. Bernert RA, Kim JS, Iwata NG, Perlis ML. Sleep disturbances as an evidence-based suicide risk factor. Curr Psychiatry Rep. (2015) 17:554. doi: 10.1007/s11920-015-0554-4
22. Freeman D, Sheaves B, Goodwin GM, Yu LM, Nickless A, Harrison PJ, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. (2017) 4:749–58. doi: 10.1016/S2215-0366(17)30328-0
23. Sexton-Radek K. Stress triggers of long, short, and variable sleep patterns. Percept Mot Skills. (1998) 87:225–6. doi: 10.2466/pms.1998.87.1.225
24. Colvonen PJ, Straus LD, Acheson D, Gehrman P. A review of the relationship between emotional learning and memory, sleep, and PTSD. Curr Psychiatry Rep. (2019) 21:2. doi: 10.1007/s11920-019-0987-2
25. Thormar SB, Gersons BPR, Juen B, Djakababa MN, Karlsson T, Olff M. The impact of disaster work on community volunteers: The role of peri-traumatic distress, level of personal affectedness, sleep quality and resource loss, on post-traumatic stress disorder symptoms and subjective health. J Anxiety Disord. (2014) 28:971–7. doi: 10.1016/j.janxdis.2014.10.006
26. Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. (2013) 36:1009–18. doi: 10.5665/sleep.2798
27. Miller KE, Brownlow JA, Gehrman PR. Sleep in PTSD: treatment approaches and outcomes. Curr Opin Psychol. (2020) 34:12–7. doi: 10.1016/j.copsyc.2019.08.017
28. Monk TH, Buysse DJ, Welsh DK, Kennedy KS, Rose LR. A sleep diary and questionnaire study of naturally short sleepers. J Sleep Res. (2001) 10:173–9. doi: 10.1046/j.1365-2869.2001.00254.x
29. The American Association for Public Opinion Research[AAPOR].Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th ed. (2016).
30. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. (2007) 335:806–8.
31. Leshem E, Klein Y, Haviv Y, Berkenstadt H, Pessach IM. Enhancing intensive care capacity: COVID-19 experience from a tertiary center in Israel. Intensive Care Med. (2020) 46:1640–1. doi: 10.1007/s00134-020-06097-0
32. Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/s1389-9457(00)00065-4
33. Morin CM, Belleville G, Bélanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
34. Spoont MR, Williams JW, Kehle-Forbes S, Nieuwsma JA, Mann-Wrobel MC, Gross R. Does this patient have posttraumatic stress disorder?: rational clinical examination systematic review. JAMA. (2015) 314:501–10. doi: 10.1001/jama.2015.7877
35. Prins A, Bovin MJ, Smolenski DJ, Marx BP, Kimerling R, Jenkins-Guarnieri MA, et al. The primary care PTSD Screen for DSM-5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med. (2016) 31:1206–11. doi: 10.1007/s11606-016-3703-5
36. Geulayov G, Jungerman T, Moses S, Friedman N, Miron R, Gross R. Validation of the hebrew version of the PHQ-9, a screening instrument for depression in primary care. Isr J Psychiatry. (2009) 46:45.
37. Levis B, Benedetti A, Thombs BD. DEPRESsion screening data (DEPRESSD) collaboration. accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476. doi: 10.1136/bmj.l1476
38. Yardeni MAM, Abebe Campino G, Bursztyn B, Shamir A, Mekori-Domachevsky E, Toren A, et al. A three-tier process for screening depression and anxiety among children and adolescents with cancer. Psychooncology. (2020) 29:2019–27. doi: 10.1002/pon.5494
39. National Institutes of Health. PROMIS: Dynamic Tools to Measure Health Outcomes from the Patient Perspective. Maryland: National Institutes of Health (2017).
40. Bevans M, Ross A, Cella D. Patient-reported outcomes measurement information system (PROMIS): Efficient, standardized tools to measure self-reported health and quality of life. Nurs Outlook. (2014) 62:339–45. doi: 10.1016/j.outlook.2014.05.009
41. Mosheva M, Hertz-Palmor N, Dorman Ilan S, Matalon N, Pessach IM, Afek A, et al. Anxiety, pandemic-related stress and resilience among physicians during the COVID-19 pandemic. Depress Anxiety. (2020) 37:965–71. doi: 10.1002/da.23085
42. Leung GM, Lam TH, Ho LM, Ho SY, Chan BH, Wong IO, et al. The impact of community psychological responses on outbreak control for severe acute respiratory syndrome in Hong Kong. J Epidemiol Community Health. (2003) 57:857–63. doi: 10.1136/jech.57.11.857
43. Imai H, Matsuishi K, Ito A, Mouri K, Kitamura N, Akimoto K, et al. Factors associated with motivation and hesitation to work among health professionals during a public crisis: a cross sectional study of hospital workers in Japan during the pandemic (H1N1) 2009. BMC Public Health. (2010) 10:672. doi: 10.1186/1471-2458-10-672
44. Tan BYQ, Chew NWS, Lee GKH, Jing M, Goh Y, Yeo LLL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med (2020) 173:317–20.
45. Laor-Maayany R, Goldzweig G, Hasson-Ohayon I, Bar-Sela G, Engler-Gross A, Braun M. Compassion fatigue among oncologists: the role of grief, sense of failure, and exposure to suffering and death. Support Care Cancer. (2020) 28:2025–31. doi: 10.1007/s00520-019-05009-3
46. Amir M, Lewin-Epstein N, Becker G, Buskila D. Psychometric properties of the SF-12 (Hebrew version) in a primary care population in Israel. Med Care. (2002) 40:918–28. doi: 10.1097/00005650-200210000-00009
48. Garson GD. Multilevel Modeling: Applications in STATA®, IBM® SPSS®, SAS®, R, & HLMTM. Thousand Oaks, CA: SAGE (2020).
49. Mosheva M, Gross R, Hertz-Palmor N, Hasson-Ohayon I, Kaplan R, Cleper R, et al. The association between witnessing patient death and mental health outcomes in frontline COVID-19 healthcare workers. Depress Anxiety. (2021) 38:468–79. doi: 10.1002/da.23140
50. Jahrami H, BaHammam AS, AlGahtani H, Ebrahim A, Faris M, AlEid K, et al. The examination of sleep quality for frontline healthcare workers during the outbreak of COVID-19. Sleep Breath. (2020): 25, 503–511. doi: 10.1007/s11325-020-02135-9
51. Qi J, Xu J, Li B-Z, Huang JS, Yang Y, Zhang ZT, et al. The evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. (2020) 72:1–4. doi: 10.1016/j.sleep.2020.05.023
52. Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup Med. (2020) 70:364–9. doi: 10.1093/occmed/kqaa074
53. Li X, Yu H, Bian G, Hu Z, Liu X, Zhou Q, et al. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain Behav Immun. (2020) 87:140–1. doi: 10.1016/j.bbi.2020.05.008
54. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
55. Preti E, Di Mattei V, Perego G, Ferrari F, Mazzetti M, Taranto P, et al. The psychological impact of epidemic and pandemic outbreaks on healthcare workers: rapid review of the evidence. Curr Psychiatry Rep. (2020) 22:43. doi: 10.1007/s11920-020-01166-z
56. Shi L, Lu Z-A, Que J-Y, Huang XL, Liu L, Ran MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in china during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053. doi: 10.1001/jamanetworkopen.2020.14053
57. Su T-P, Lien T-C, Yang C-Y, Su YL, Wang JH, Tsai SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
58. Tang W, Lu Y, Yang Y, Xu J. An epidemiologic study of self-reported sleep problems in a large sample of adolescent earthquake survivors: the effects of age, gender, exposure, and psychopathology. J Psychosom Res. (2018) 113:22–9. doi: 10.1016/j.jpsychores.2018.07.006
59. Devi S. COVID-19 exacerbates violence against health workers. Lancet. (2020) 396:658. doi: 10.1016/S0140-6736(20)31858-4
60. Dye TD, Alcantara L, Siddiqi S, Barbosu M, Sharma S, Panko T, et al. Risk of COVID-19-related bullying, harassment and stigma among healthcare workers: an analytical cross-sectional global study. BMJ Open. (2020) 10:e046620. doi: 10.1136/bmjopen-2020-046620
61. Magnavita N, Di Stasio E, Capitanelli I, Lops EA, Chirico F, Garbarino S. Sleep problems and workplace violence: a systematic review and meta-analysis. Front Neurosci. (2019) 13:997. doi: 10.3389/fnins.2019.00997
62. Barger LK, Runyon MS, Renn ML, Moore CG, Weiss PM, Condle JP, et al. Effect of fatigue training on safety, fatigue, and sleep in emergency medical services personnel and other shift workers: a systematic review and meta-analysis. Prehosp Emerg Care. (2018) 22:58–68. doi: 10.1080/10903127.2017.1362087
63. Germain A, McKeon AB, Campbell RL. Sleep in PTSD: Conceptual model and novel directions in brain-based research and interventions. Curr Opin Psychol. (2017) 14:84–9. doi: 10.1016/j.copsyc.2016.12.004
64. Germain A. Sleep disturbances as the hallmark of PTSD: where are we now? Am J Psychiatry. (2013) 170:372–82. doi: 10.1176/appi.ajp.2012.12040432
65. Carmassi C, Foghi C, Dell’Oste V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers facing the three coronavirus outbreaks: what can we expect after the COVID-19 pandemic. Psychiatry Res. (2020) 292:113312. doi: 10.1016/j.psychres.2020.113312
66. Johnson SU, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS One. (2020) 15:e0241032. doi: 10.1371/journal.pone.0241032
Keywords: sleep, sleep difficulties, COVID-19, health care workers (HCW), COVID-19 outbreak, sleep disorders, health care staff, stress
Citation: Cleper R, Hertz-Palmor N, Mosheva M, Hasson-Ohayon I, Kaplan R, Kreiss Y, Afek A, Pessach IM, Gothelf D and Gross R (2022) Sleep Difficulties Among COVID-19 Frontline Healthcare Workers. Front. Psychiatry 13:838825. doi: 10.3389/fpsyt.2022.838825
Received: 18 December 2021; Accepted: 28 March 2022;
Published: 29 April 2022.
Edited by:
Heon-Jeong Lee, Korea University, South KoreaReviewed by:
Francesco Chirico, Catholic University of the Sacred Heart, Rome, ItalyAthanasia Pataka, Aristotle University of Thessaloniki, Greece
Copyright © 2022 Cleper, Hertz-Palmor, Mosheva, Hasson-Ohayon, Kaplan, Kreiss, Afek, Pessach, Gothelf and Gross. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Raz Gross, Raz.Gross@sheba.health.gov.il
 Rony Cleper
Rony Cleper Nimrod Hertz-Palmor
Nimrod Hertz-Palmor Mariela Mosheva
Mariela Mosheva Ilanit Hasson-Ohayon
Ilanit Hasson-Ohayon Rachel Kaplan2
Rachel Kaplan2 Doron Gothelf
Doron Gothelf Raz Gross
Raz Gross