- 1Department of Psychiatry and Psychotherapy, Evangelisches Klinikum Bethel, Universitätsklinikum OWL of Bielefeld University, Bielefeld, Germany
- 2Department of Psychology, Bielefeld University, Bielefeld, Germany
Background: Major depression is one of the leading causes of disability and limited capacity to work. Neuropsychological impairment is a common symptom in acute and remitted major depression and is associated with poor psychosocial functioning. This scoping review aimed to identify research on the role of neuropsychological functioning in outcomes of vocational rehabilitation programs in individuals with depression.
Methods: We report on the conduct of this pre-registered (https://osf.io/5yrnf) scoping review in accordance with PRISMA-ScR guidelines. PubMed and PsychInfo were systematically searched for English or German research articles published between 1990 and September 2021 that studied objective neuropsychological tests as predictors of vocational rehabilitation interventions and included participants with depression.
Results: The systematic literature search yielded no studies that specifically targeted subjects with major depression. However, eight articles published since 2016 were included in the review, analyzing data from five trials that evaluated the effectiveness of supported employment in North America and Europe in severe mental illnesses. An estimated 31% of the total number of participants included (n = 3,533) had major depression. Using a variety of cognitive tests and covariates, seven articles found that neuropsychological functioning – especially global cognition scores, verbal and visual learning and memory – significantly predicted vocational outcomes of rehabilitation programs.
Conclusion: Despite a lack of studies specifically targeting major depressive disorder, the identified literature suggests that higher baseline neuropsychological functioning predicts better vocational outcomes of supported employment programs in individuals with depression. In clinical practice, additional neuropsychological modules during return-to-work interventions might be helpful for vocational outcomes of such programs.
Introduction
Major depressive disorder is on top of the world’s most prevalent mental health problems and is associated with poor health, mortality, disease and increased disability (1, 2). Major Depression, even in remission, also affects working life and is related to unemployment, reduced work productivity, absenteeism and presenteeism (3), accounting for a high economic burden across different countries (4, 5). Moreover, depression is related to an increased risk for early retirement and applying for disability pension (6, 7).
The major symptoms of depression are depressed mood and loss of interest or lack of pleasure, but it also comes along with several cognitive impairments like diminished ability to think, reduced concentration and attention, or indecisiveness (8, 9). Subjectively perceived cognitive deficits have been associated with perceived global disability, workplace performance, and quality of life (10). Meta-analysis have confirmed objective neuropsychological deficits in depressive disorders in the domains of attention, memory and executive function (11). There is evidence that cognitive dysfunction across several neuropsychological domains is already identifiable in the first episode of depression (12). In addition, cognitive impairment was shown to persist even in remitted patients (12, 13) and appeared to be a long lasting residual-symptom (14) that increases the risk of relapse (15).
Neuropsychological deficits are negatively related to various aspects of psychosocial functioning, treatment progress, quality of life and occupational outcomes (16–19). Recent reviews suggest that neuropsychological deficits may be a principal predictor of occupational functioning (17, 20, 21). Specifically, one review found that employment status and work impairment were associated with neuropsychological deficits across several domains, e.g., attention, executive functions and verbal memory in two depressed samples (17). Clark et al. (20) concluded that cognitive dysfunction in various domains may have a direct impact on work productivity, especially on presenteeism in depressed people. Woo et al. (21) found evidence that residual deficits in memory, attention, learning and executive function predict occupational impairment even in people with remitted depression.
To support people with major depression returning to work or reducing work disability (e.g., sickness absence), several rehabilitation approaches have been studied (22). A recent review (22) about vocational rehabilitation interventions for people with depression showed overall possible positive effects of a combination of work-directed and psychological interventions in reducing illness-related absence days compared to care as usual, but no difference was found with regard to the amount of people who worked at follow-up. Given the emerging evidence about the association between cognitive functioning and vocational functioning in acute and remitted major depression, neuropsychological variables may also affect outcomes of vocational rehabilitation interventions. Evidence comes from studies of people with psychotic disorders and supported employment (SE) programs, like the evidence-based Individual Placement and Support model (IPS) that provides rapid job search based on individual preferences and skills, and long-term support at the workplace (23). IPS and other programs using SE like the Program for Assertive Community Treatment (PACT) have been shown to significantly improve vocational outcomes for people with severe mental illnesses (24, 25). Research in schizophrenia suggests that more severe cognitive impairment predicts worse work and SE outcomes, including the number of hours worked, job tenure and wage levels (26–32). For example, higher scores in the subdomains of executive functions (32), visual organization and memory (26), and verbal learning and memory (28) have been identified to significantly predict better rehabilitation outcomes in addition to general cognitive function. Accordingly, additional cognitive training has been examined in people enrolled in SE (33). In samples with psychotic or bipolar disorders receiving SE, there is evidence for the effectiveness of additional cognitive training for gaining competitive employment and other work-related outcomes, further supporting the hypothesis that cognitive functioning influences the success of vocational rehabilitation interventions (34–39). For instance, over 2–3 years, patients in the SE with cognitive training program were more likely to work, held more jobs, worked more weeks and hours, and earned higher wages than patients who received SE alone (38).
In sum, neuropsychological impairment is a common and meaningful symptom in major depressive episodes, and SE interventions that help people with SMI to return to work have been shown to be effective. In addition, a relationship between neuropsychological performance and work outcomes has already been demonstrated for some psychiatric and neurological patient samples [e.g., (40–42)]. However, it is unclear whether and how these known neuropsychological impairments might specifically affect the benefits of return-to-work interventions for individuals with major depression. Addressing these issues might have important healthcare implications, given the high prevalence of major depression and the occupational limitations associated with this disorder. It is unclear if the association between neuropsychology and rehabilitation outcomes also holds for SE participants with psychiatric diagnoses other than psychosis, because persons with schizophrenia show more severe cognitive deficits than for example severely depressive patients (43). Learning more about the relationship between neuropsychological variables and vocational rehabilitation program outcomes in people with major depressive disorder is crucial for the development and adjustment of occupation-related interventions, such as SE, for people with depression. If neuropsychological functioning could be shown to affect outcomes of vocational rehabilitation programs, diagnostic assessments and interventions targeting cognition can be used to enhance work-related outcomes and improve the quality of life of people with major depressive disorder. Following a scoping review approach, we aimed to identify existing research on the association between cognitive functioning and outcomes of vocational rehabilitation interventions in people with depressive disorders. We conducted a scoping review to provide an overview of the scope and nature of research on neuropsychological variables as predictors of the success of return-to-work interventions for people with major depression. Scoping reviews aim to identify and map the existing research on a particular topic that is usually broadly defined. Following a systematic literature search they may identify research gaps, key concepts, theories, or sources of evidence (44). Specifically, we aimed to answer the following research questions:
• What research is available regarding the association between neuropsychological functioning and vocational rehabilitation intervention outcomes in people with depressive disorders, what were study contexts and which main research questions were posed?
• Which rehabilitation interventions have been examined?
• Which neuropsychological domains and tests have been investigated?
• What vocational outcomes have been used and which major results have been found?
Methods
Protocol and registration
The study protocol was prospectively registered with the Open Science Framework on September 9, 2021.1 This scoping review was performed using the Joanna Briggs Institute guidance for the conduct of scoping reviews (44). We report the conduct and results of this scoping review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews (45).
Eligibility criteria
Original research studies published between 1990 and 2021 in English or German language were included that (a) had a quantitative-empirical study design, (b) had examined persons with a depressive disorder and, if applicable, a comparison or healthy control group, (c) examined a vocational rehabilitation intervention, (d) measured, among other characteristics, neuropsychological variables prior to the intervention and (e) statistically correlated outcome criteria with baseline variables following the intervention. Reviews published between 1990 and 2021 in English or German language were included if they examined the association between neuropsychological variables and outcomes of vocational rehabilitation interventions in people with major depressive disorder. Studies were excluded, if they did not include patients with depressive disorders, did not conduct an occupational or work-related intervention, or did not provide information on baseline neuropsychological variables and/or vocational outcome parameters.
Search strategy and study selection
PubMed and PsychInfo were searched for relevant articles using combinations of search terms for the three relevant topics neuropsychological performance AND work-related rehabilitation AND depressive disorders. Specifically, for neuropsychological performance the following search terms were used: [(“cognition”) OR (“cognitive function*”) OR (“cognitive impairment”) OR (“cognitive dysfunction”) OR (“cognitive deficit”) OR (“neurocog*”) OR (“neuropsycholog*”) OR (“memory”) OR (“executive function*”) OR (“verbal learning”) OR (“processing speed”)].
Regarding work-related rehabilitation interventions, the following terms were used: [(“supported employment”) OR (“individual placement and support”) OR (“individual enabling and support”) OR (“vocational rehabilitation”) OR (“work-focused”) OR (“job acquisition”) OR (“job coaching”) OR (“occupational rehabilitation”) OR (“work-related”) OR (“vocational rehabilitation”) OR (“work-directed”) OR (“vocational training”) OR (“prevocational training”) OR (“vocational intervention”)].
Finally, search terms for depressive disorder were: [(“major depression”) OR (“depression”) OR (“depressive disorder”) OR (“major depressive disorder”) OR (“depress*”)].
To find studies that include all three topic areas, AND operators were used between each combination of terms for the topics. The search query was adapted for the respective requirements of each database. For the PubMed search query, terms were searched in [All Fields]. The initial search was conducted on September 10, 2021. In addition, reference lists of the included manuscripts were searched for further relevant studies. During citation searching, we noticed a couple of studies examining neuropsychological variables among several other predictors of vocational rehabilitation outcomes. As scoping reviews may follow an iterative search strategy (44) and to avoid overlooking neuropsychological predictors in this study area, we performed a further PubMed search, using the following search terms: (“predict*”[Title/Abstract]) AND (“IPS”[Title/Abstract] OR “individual placement and support”[Title/Abstract] OR “vocational rehabilitation”[Title/Abstract] OR “supported employment”[Title/Abstract]) AND (“mental illness*” [Title/Abstract] OR “depressive disorder”[Title/Abstract]).
First, two authors (LD and JB) independently screened titles and abstracts of the literature search for eligibility. Full texts of articles that had not been excluded in the first step, were independently reviewed by LD and JB with respect to the research question. Ambiguities were discussed and resolved by joint consensus.
Data charting and data items
Two authors (LD and JB) jointly developed a data charting form that was updated in an iterative process. Data were charted independently and results were discussed. First, variables to describe the study in terms of year of publication, country, study design, and sample characteristics were extracted. With regard to our research question, the following data were abstracted: main research question, neuropsychological domains and tests, other examined predictors, information about the studied vocational intervention, any occupational outcomes, main findings and findings regarding neuropsychological functioning predicting vocational rehabilitation intervention outcomes.
Synthesis of results
First, we grouped basic information of the included articles in terms of authors, publication year, country, sample size, target group, and intervention. In a separate table, we mapped data regarding neuropsychological predictors, with neuropsychological tests used, main research questions, included covariates, follow-up period, and vocational outcomes variables. The results presented in the tables were then summarized narratively. To display the amount of participants with major depression included in the samples, we summarized the total number and percentages of diagnostic groups included in each articles’ sample. If articles did not report on exact diagnostic groups, we aimed to collect information about their sample in other published research papers about the trials. When subsamples were used and information on the exact number of participants with a diagnosis was not available for a specific subsample, we estimated the number of participants with a particular diagnosis by extrapolating the percentage of individuals with that diagnosis in the base sample.
Results
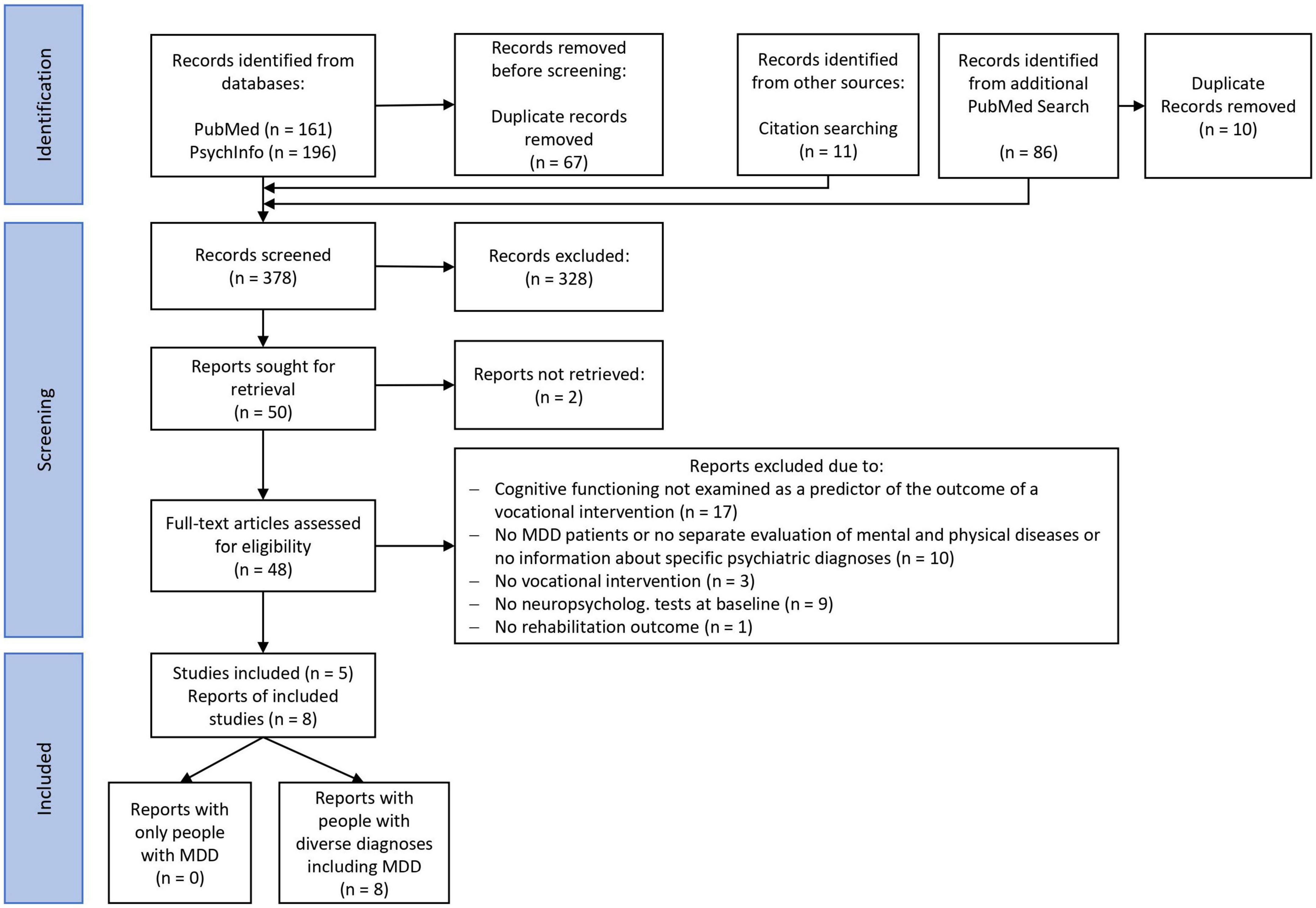
The systematic literature search revealed no studies investigating neuropsychological predictors of vocational rehabilitation interventions specifically for persons with major depression. However, we identified eight articles related to our research question that examined diagnostically mixed samples including major depressive disorder. Due to the exploratory approach of scoping studies, these articles were still included if they examined individuals with depression in addition to participants with other psychiatric diagnoses. Figure 1 shows the search and inclusion process according to the PRISMA flow chart. The eight included reports analyzed data from five studies. Because the articles nevertheless focused on different aspects regarding neuropsychological predictors of work outcomes, we decided to consider all articles separately, even when they were based on the same sample.
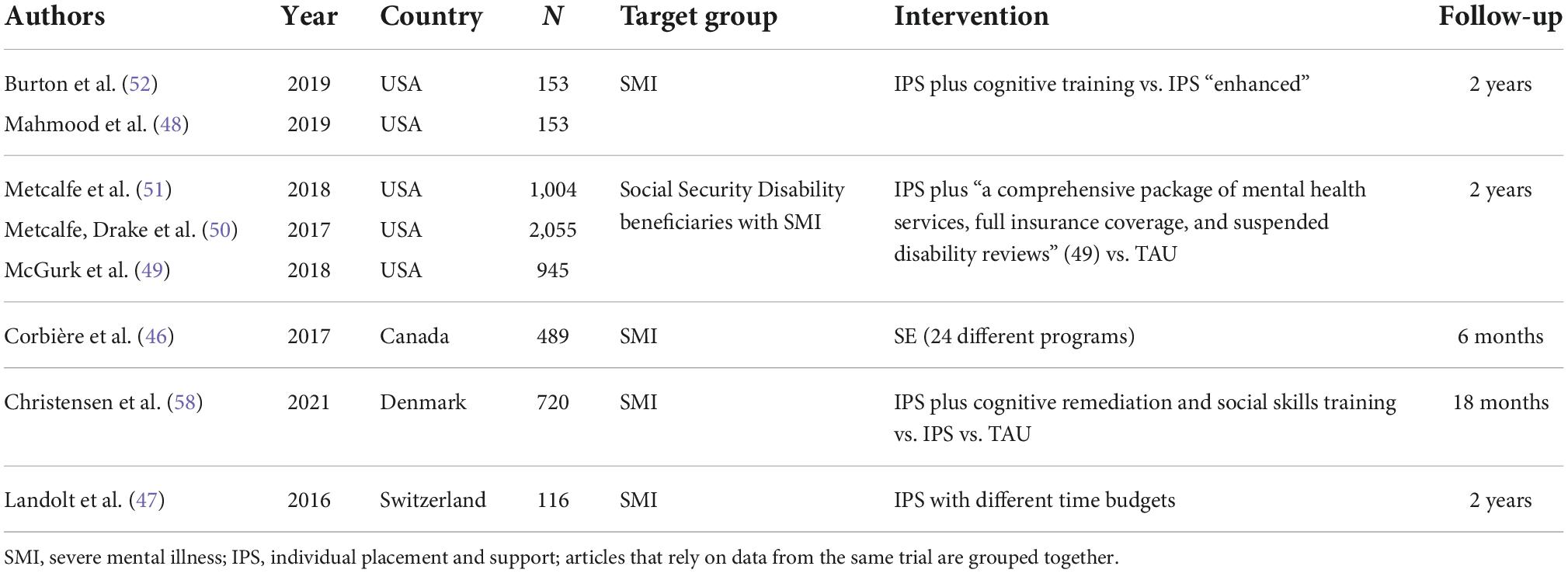
All eight reports were original research articles published in peer-reviewed psychiatric and mental health (46–51), or neuropsychological (52) journals, including one brief report (47). Table 1 describes the included research articles in terms of publication year, country in which the sample was recruited, total analyzed sample size, target group, and vocational intervention. Although research published since 1990 was eligible for inclusion, all included articles were published between 2016 and 2021. Data have been collected in the context of five studies (53–57) evaluating SE or IPS interventions in people with SMI who were currently unemployed and looking for a job. Three studies (54–56) were conducted in North America (n = 2 USA, n = 1 Canada), while two (53, 57) were conducted in European countries (n = 1 Switzerland, n = 1 Denmark). Of the five studies, one was a longitudinal observational study without a control group (56), and four were randomized controlled trials evaluating different IPS interventions. The studied interventions varied substantially in terms of additional support provided besides the work-focused SE or IPS programs.
According to the method sections of the articles, a total of n = 3,533 participants were included in the five studies. Sample sizes differed widely ranging from n = 116 (47) to n = 2,055 (50). Metcalfe et al. (51) and McGurk et al. (49) both analyzed sub-samples (intervention group) of a study with a total n = 2,055 that Metcalfe, Drake et al. (50) used for their analyses. All articles reported that the target group were people with SMI, but one study (54) only included people with SMI who received social security disability benefits. Figure 2 shows the total samples sizes and the percentage of people with major depression in each articles’ sample. Because Metcalfe, Drake et al. (50) and Metcalfe et al. (51) did not specify the amount of people with major depression, data from the same sample reported by McGurk et al. (49) were extrapolated to estimate the total number of participants with major depression and bipolar disorder in all studies (see 2.5 synthesis of results). According to this calculation, the total number of participants diagnosed with major depressive disorder across all five studies was approximately n = 1,103 (31%). The proportion of participants with major depressive disorder varied between 11% (58) and 43% (47). The most prevalent other primary diagnoses were psychotic disorders (total n = 1,373; 38%) and bipolar disorders (estimated total n = 852; 24%). The articles created diagnostic subgroups based on the primary diagnosis (e.g., major depressive disorder) or primary diagnostic group (e.g., affective disorders). As the articles did not report all their results separately for major depression and other diagnoses, the compiled findings on neuropsychological predictors of vocational interventions presented below include data from individuals with a primary diagnosis of major depression as well as from individuals with other primary SMI diagnoses. In one part of the results section, however, we summarize some analyses of differences between diagnostic groups on neuropsychological measures and vocational outcomes from individual studies.
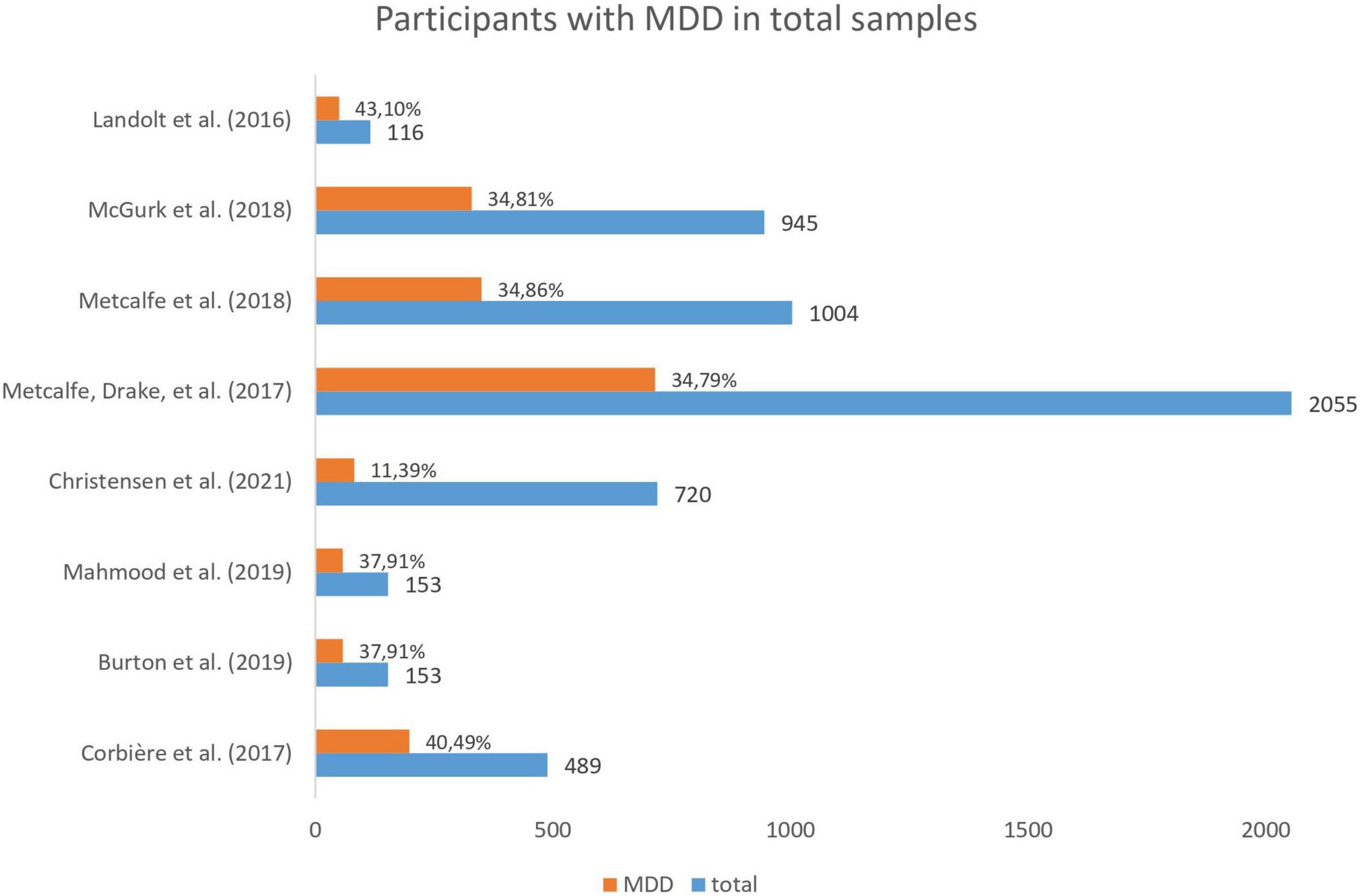
Figure 2. Total number of participants and percentage of people with major depressive disorder (MDD) included in each article.
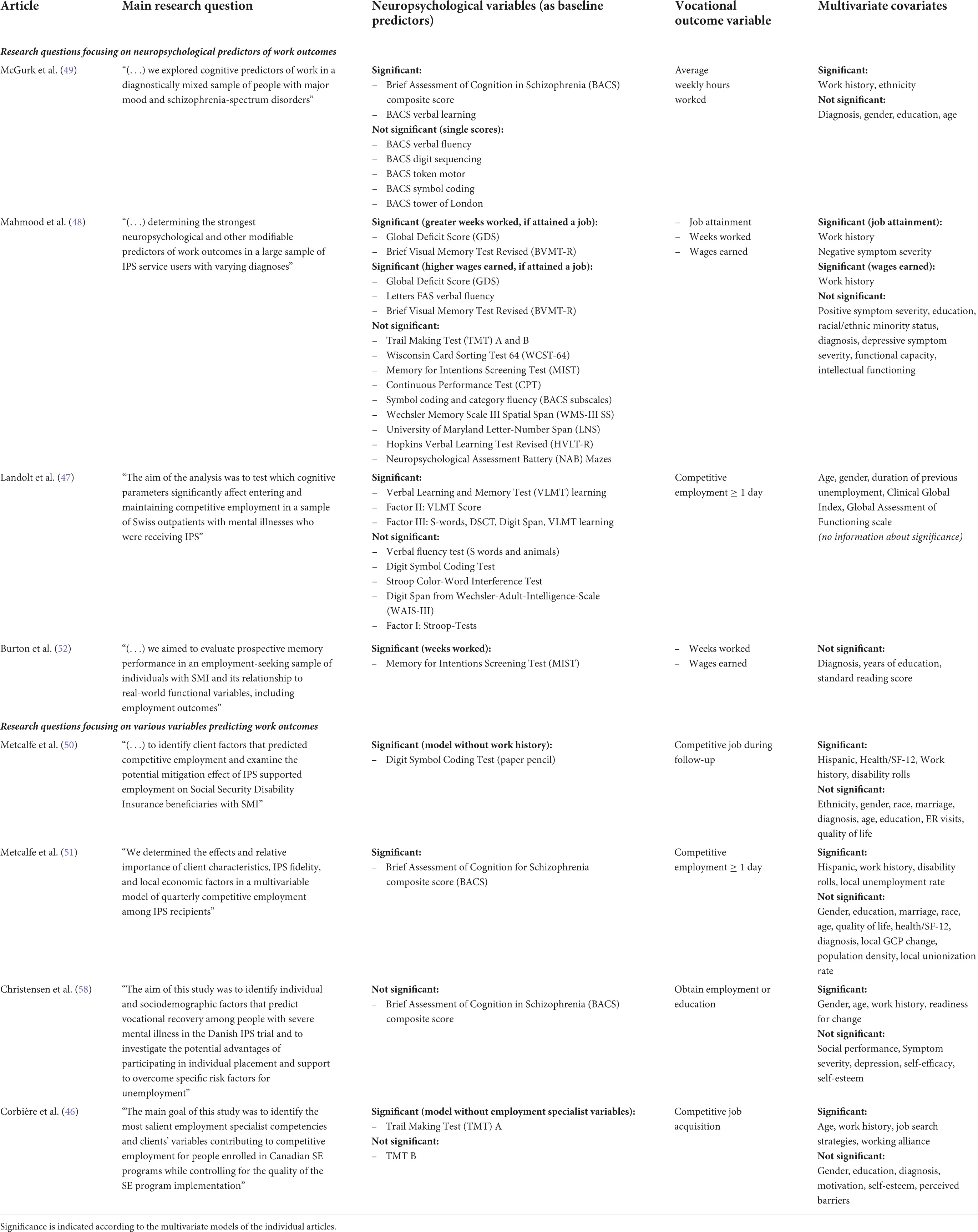
Table 2 provides an overview of the main research questions, neuropsychological measures, vocational outcome variables, and covariates of the articles included.
Research questions and neuropsychological tests
With respect to the role of neuropsychological predictors in the research questions, two types of articles were identified. Main research questions of four articles (47–49, 52) explicitly focused on neuropsychological variables while the main research questions of the other four articles (46, 50, 51, 58) focused on various client or context variables predicting work outcomes of vocational rehabilitation programs, including neuropsychological predictors. In general, articles assessed a wide range of neuropsychological tests and cognitive domains. Articles used only one neuropsychological test (50) or various tests or test batteries (see Table 2). The most frequently used test (n = 4) was the Brief Assessment of Cognition in Schizophrenia (BACS), which contains the six measures list learning, digit sequencing task, token motor task, category instances and controlled word association tests, symbol coding test, and Tower of London (59). Two articles (51, 58) only analyzed the BACS composite score which is calculated across scores of all six measures, while one article (48) only used two subscale scores (symbol coding and category fluency) and one article evaluated both the composite and all six individual test scores (49).
Results at bivariate level
All articles evaluated the role of cognitive functioning for predicting outcomes of vocational rehabilitation interventions in models with multiple predictor variables. Five articles (47–49, 51, 58) additionally reported bivariate associations between cognitive functioning and work outcomes. In all of them, some neuropsychological variables [BACS composite score, BACS-symbol coding, letter-number-span, Wisconsin card sorting test, digit span, and Verbal Learning and Memory Test (VLMT)] were significantly associated with work outcomes of the SE intervention. Additionally, Metcalfe, Drake et al. (50) reported that participants who were employed during follow-up performed significantly better on the baseline Digit Symbol Test than participants who were unemployed at follow-up.
Results at multivariate level
Of eight articles included, seven found a significant predictive effect of any neuropsychological measure in multivariate models predicting work outcomes of the vocational rehabilitation program (46–52). Considering that some articles relied on the same samples, this implies that four out of five studies showed that higher baseline neuropsychological test scores predicted better outcomes of SE interventions. Individual test scores, as well as global cognition scores were analyzed.
Global cognition scores
Five articles used composite scores of individual neuropsychological tests to predict SE outcomes in models with multiple predictors, of which four observed significant results. Mahmood et al. (48) calculated a “global deficit score” (GDS) averaging cognitive impairment across all 13 individual measures and found that GDS significantly predicted average hours worked and total wages earned in participants who attained a job. Landolt et al. (47) conducted an exploratory factors analysis and found that the most general factor (digit symbol and digit span tests, verbal learning score, verbal fluency test) significantly predicted job attainment and maintaining a job. McGurk et al. (49) found that the BACS composite score significantly predicted average hours worked. Metcalfe et al. (51) and Christensen et al. (58) both evaluated if the BACS composite score predicted job attainment during the follow-up period, but only Metcalfe et al. (51) found it to be a significant predictor.
Individual tests
Among the individual tests assessed, mainly measures of verbal and visual learning and/or memory significantly predicted SE outcomes. In one article, the Brief Visual Memory Test Revised (BVMT-R) significantly predicted average weeks worked and wages earned (48). Furthermore, the VLMT utilized by Landolt et al. (47) was significantly associated with job attainment. Regarding the BACS subtests, McGurk et al. (49) showed that only verbal learning remained significant in a model including all predictors. Burton et al. (52) only studied one cognitive dimension, namely prospective memory measured by the Memory for Intentions Screening Test (MIST) and found it to be a significant predictor of weeks worked during 2 years of SE. However, the analysis of the same sample by Mahmood et al. (48) including many other predictors did not show a significant effect of the MIST score. Likewise, another verbal learning test (HVLT-R) (48) and short-term memory tests (digit span/spatial span) (47, 48) did not reach significance in other articles.
Besides verbal and visual learning and memory, verbal fluency was predictive of wages earned (48) and processing speed measured by the Digit Symbol Coding Test (50) or the Trail Making Test (TMT) A (46) was significantly associated with job attainment. However, when employment specialist variables were entered into the model, the TMT A score was not significant anymore in the article by Corbière et al. (46) and the Digit Symbol Coding Test only reached borderline significance when work history was entered into the model (50). At the bivariate level, the BACS-symbol-coding subtest has been significantly associated with the amount of work during follow-up (48, 49). However, in other articles, a digit symbol coding test (47) and verbal fluency tests (47, 49), were not found to be significant predictors of vocational outcomes of SE among other significant neuropsychological variables.
In general, the included articles suggest that tests measuring complex executive functions, like Tower of London (49), or Stroop test (47), were not among the significant single domains. Likewise, the TMT A and B which were intended to measure processing speed and executive functions, respectively, were not found to be significant predictors in another article (48).
Covariates
The majority of articles included a measure of work history in their multivariate models (n = 7/8) (46–51, 58). The articles defined work history differently, with:
• four articles reporting a dichotomous measure, namely any paid work during the past 2 years (yes/no) (49–51), or at least 2 months of work within the last 5 years before baseline (yes/no) (58),
• and three articles reporting a continuous measure, namely time (months or years) of unemployment before study entry (46–48).
Work history significantly predicted work outcomes of SE at multivariate level in all these articles, with the restriction that Landolt et al. (47) did not report on the significance of covariates. Neuropsychological variables significantly added predictive power to models that also included work history in four of seven articles according to the alpha levels that the authors applied (47–49, 51). Metcalfe, Drake et al. (50) concluded that the Digit Symbol Coding test reached borderline significance when work history was included in the model.
With regard to demographic variables like age, gender, or ethnicity that many articles assessed, the results were inconclusive. No interaction effects with neuropsychological variables were investigated, except for diagnostic group.
Diagnostic group
In sum, all results reported were not exclusive for depressive participants and include data from mixed SMI samples with patients with major depressive disorder and other, mainly psychotic, diagnoses. This prevents us from reporting neuropsychological findings on SE outcomes as specifically related to people with major depression. However, some included articles analyzed diagnostic differences in their results, which are summarized here. Persons with psychotic disorders performed worse on some prospective memory subscales (52) and the BACS (49), and had a greater overall cognitive impairment score (48) than persons with affective disorders. However, diagnostic group (n = 3 affective disorders vs. psychotic disorders; n = 4 major depression vs. bipolar disorder vs. psychotic disorders) had no significant effect on SE outcomes in either article that entered it into the multivariate models (46, 48–52). Thus, some authors concluded that their results are valid independent of diagnosis (48, 49, 52). Only McGurk et al. (49) entered the interaction between neuropsychological predictors and diagnosis (affective disorder vs. psychotic disorder) into their predictive model. Because the interaction did not reach significance or improve model fit, the authors concluded that their neuropsychological measures predicted SE outcomes equally well in patients with affective disorders and patients with psychotic disorders.
Work-related outcomes
The most common work outcome was competitive job attainment during the follow-up period (n = 6) (46–48, 50, 51, 58), with one article (58) also including education aiming for competitive employment. Job attainment was defined as working in a competitive job at least for one day during the follow-up (47, 50, 51) or it was not further specified (46, 48, 58). Three (47, 50, 51) out of six articles found neuropsychological variables to be a significant predictor of job attainment. Regarding weeks worked (48, 52) and average weekly hours worked (49) over the study period, all three articles observed significant effects of neuropsychological variables, and regarding wages earned one (48) article found a significant effect of cognitive tests, while the other (52) did not.
Follow-up period
The most common follow-up period was 2 years (n = 6), while 6 months (46) and 18 months (58) follow-up were only reported by one article each. To evaluate if the effect of cognitive predictors changed over time, McGurk et al. (49) added a time (quarters of 2-year period) by cognitive scores interaction into their predictive model, but the interaction was not significant and did not improve model fit.
Control conditions
Among the eight included papers, only two study designs included a control group that did not receive any work-related intervention (treatment as usual; TAU) which were analyzed by two research articles included (50, 58). The interaction between study condition and cognitive variables was not significant in Metcalfe, Drake et al. (50). However, Christensen et al. (58) reported that cognitive functioning significantly predicted vocational recovery only in the IPS group compared with TAU and IPS plus cognitive and social skills training. The formal test of interaction effects, however, did not reveal a significant interaction as defined by the authors (p < 0.001). Landolt et al. (47) reported that the duration of SE (25, 40, or 55 h) did not influence the relationship between cognitive functioning and finding a job.
Discussion
The aim of this scoping review was to identify and map research on the role of neuropsychological predictors of outcomes of vocational rehabilitation programs in people with major depressive disorder. The systematic literature search suggests that studies focusing exclusively on patients with major depression are missing when it comes to examining the impact of neuropsychological deficits on how individuals benefit from such programs. Moreover, research on samples with different diagnoses examining cognitive predictors that include patients with major depression is limited to only five study samples included with an estimated total of 1,103 (31%) depressive participants. In addition, we identified only four articles that focused on neuropsychology in their main research questions, and the included articles varied widely in terms of interventions, follow-up periods, diagnostic groups, outcome measures, neuropsychological tests, and covariates. However, SE and IPS, respectively, were the only rehabilitation approaches examined, suggesting that current research on cognitive predictors including persons with major depression mainly focuses on first place-then train (60) interventions. In sum, most articles found that neuropsychological measures significantly predicted work outcomes of SE interventions with global cognition scores, learning and memory tests, as well as processing speed and verbal fluency being relevant predictors. In several articles, neuropsychological variables were even significant when the important predictor work history was controlled for (46–49, 51), but due to the small number of studies and different study designs, more research targeting participants with major depressive disorder is needed to draw definite conclusions.
Major depressive disorder diagnosis
The limited research focusing on depression is surprising, given that major depression is one of the most common mental disorders and among the leading causes for disability and early retirement (1). Many employees also experience negative effects of the depressive disorder on work participation and functioning, such as productivity loss or sickness absence. Although there is long-standing evidence of cognitive impairment and its association with psychosocial functioning in major depression (11, 16, 61), research on cognitive functioning in vocational rehabilitation programs that includes patients with major depression at all appears to have increased only recently, as all studies included in this review have been published only since 2016. This fits with the results of two reviews that could only include few studies on neuropsychological predictors of occupational functioning and the association of neuropsychology with employment (16, 17). In general, a recent review suggests that studies on vocational outcomes of IPS mainly include participants with schizophrenia and that existing studies might lack power to detect effects on people with major depression (62). To address diagnostic differences, IPS has recently been adapted for individuals with affective disorders to include “motivational, cognitive, and time use strategies” in addition to SE (63), but neuropsychological predictors have not yet been included.
However, diagnosis was not a significant predictor of work outcomes in any article and some authors concluded that their results apply independent of psychiatric diagnosis (48, 52). Only one article included the interaction between neuropsychology and diagnosis, but it supported the conclusion that neuropsychological measures are equally predictive of work outcomes of SE in persons with affective disorders as they are in persons with schizophrenia (49). This is noteworthy because it underlines how important neuropsychological aspects might be for returning to work also for patients with major depression, even if they showed less severe deficits in neuropsychological tests than persons with schizophrenia (48, 49, 52). Is has to be noted that several included studies did not distinguish between bipolar disorder and major depression, or major depression subtypes although they seem to show different patterns of cognitive impairment (64–67). In sum, research aiming at identifying diagnostic differences in neuropsychology predicting vocational outcomes of rehabilitation interventions is missing and more articles are needed to examine whether global cognition or certain domains predict outcomes differently for major depression and other diagnoses and in participants with different levels of impairment.
Neuropsychological predictors of work outcomes
Because several studies aimed to identify the most relevant predictors of work outcomes, cognitive functioning was included in multivariate analysis alongside various other predictors of the success of the SE programs, like work history (46–51, 58), employment specialist competencies (46), or environmental factors (51). There was both evidence that cognitive functioning was a robust predictor even with these factors included and, on the other hand, that cognitive factors were no longer significant when other variables are included in the model (46, 58). The inconsistent results may be due to differences in measurement of predictors and outcomes, for instance the use of categorical or continuous measures of work history. It has been previously noted that a more precise coverage of important and complex constructs might contribute to a better understanding of IPS success (51).
The neuropsychological tests used covered a wide range of functional domains, but the instruments and the number of tests differed between articles. Given that some articles used the same samples, four out of five studies found a significant effect in their multivariate models predicting work outcomes of SE. Global test scores were significant predictors, as well as verbal learning and verbal and visual memory scores, which matches results of previous IPS studies on schizophrenia (68). The significance of global scores is in line with the finding that no specific pattern of cognitive deficits in depression has been identified yet and most studies show broad cognitive functions to be impaired (61). It also can be explained by the broad cognitive abilities that are required at the workplace and probably very different jobs that participants were searching. In general, modern jobs may more often require cognitive rather than physical abilities. Given that the actual impairment in cognitive functions differed between diagnoses and between studies, significant subdomains might reflect which cognitive abilities were especially relevant for participants’ jobs, such as verbal and visual abilities. However, the included studies on SE did not report which jobs their participants have had before, or which jobs they were aiming for. Including this in future research might allow to evaluate how cognitive functioning matches the cognitive requirements at the workplace, if it has an impact on vocational rehabilitation program outcomes, and how this is influenced by SE (29, 69).
The significant results regarding cognitive predictors of rehabilitation success suggest that even with individual vocational and psychosocial services, higher baseline cognitive functioning predicts better work-related outcomes. This is in line with studies showing that improvement in cognitive functioning can contribute to more positive outcomes of rehabilitation interventions (70, 71). Furthermore, cognitive remediation has the potential to improve work outcomes of rehabilitation interventions (38). Our results suggest that additional neuropsychological modules in such interventions may also be beneficial for people with depressive disorders. However, because only two articles included control groups without any intervention, the interaction between cognitive functioning and vocational interventions remains unclear. One model attempted to explain this interaction and the authors proposed that SE may compensate for some cognitive deficits (30). Our results support the suggestion that SE at least does not fully compensate for cognitive deficits in samples including patients with major depressive disorder. The question of whether specific subdomains may be compensated by SE and by what mechanisms is important for future research (47).
With regard to subdomains, it is noteworthy that executive functions did not significantly predict rehabilitation outcomes, although they have been associated with psychosocial functioning in depression before (72). As noted above, it is possible that SE compensated for deficits in executive functions (31), but according to the model by McGurk et al. (30) SE would compensate for basic cognitive functions such as attention rather than more complex functions. In addition, Porter et al. (66) noted several methodological issues to be considered when comparing significant with non-significant test results, such as the psychometric properties of the tests used (e.g., reliability or ceiling effects). Moreover, many tasks that are supposed to measure a certain cognitive domain often require many different cognitive functions (66). In the included articles, test scores that were used to measure a certain subdomain, such as processing speed (TMT-A; digit symbol coding test) or executive functioning (TMT-B), were used in other articles as a measure of global cognitive functioning, so in sum we cannot draw definite conclusions regarding most relevant subdomains.
Especially for individuals with major depressive disorder, future studies may consider including alternative definitions of cognitive impairment, because objective test results often do not match subjective impairment (73–76). Current studies suggest that the intraindividual differences between current deficits and premorbid cognitive functioning may be more relevant to subjective functional impairment at work than normative comparisons (77), because people are likely to have jobs that match their premorbid cognitive abilities and therefore are sensitive to deficits that would normatively be regarded unimpaired. Douglas et al. (64) showed that the amount of people defined as cognitively impaired increased significantly when correcting for premorbid IQ in inpatients with major depressive disorder. Individuals who have previously worked in an occupation with high cognitive demands may be more likely to subjectively perceive differences from their premorbid cognitive abilities and may not feel ready to return to work until they have not reached their premorbid levels, even if their test scores are normatively in the average range. In addition, even small cognitive deficits may still be relevant at the workplace for this group (17). Furthermore, performance on standardized tasks does not necessarily reflect real-life impairment in the workplace, because cognitive deficits increase in patients with major depression during experiences of failure (78) or emotionally negative distractions (79), which is more likely the case in the workplace. Moreover, there are several other illness related variables that are associated with cognitive impairment in major depression, such as rumination (80), attentional bias (81), and motivation (82, 83) which could be examined in terms of their interaction with neuropsychology and IPS outcomes.
Considering that the effect of cognition on employment status was only significant in half of the included articles that examined it, the outcome measure used by most SE studies, which is job attainment, may need to be broadened. A review suggests that cognitive deficits in major depressive disorder most importantly influence presentism rather than absenteeism (20) which has not been examined as an outcome variable in the included articles. Moreover, it has been suggested that cognitive functioning most importantly influences work behaviors or job tenure rather than work status (68, 84). If SE can support participants to return to work despite cognitive deficits, work productivity, job tenure, and the type of work also need to be considered especially in patients with major depression in order not to overlook functional impairment at the workplace. More diverse outcome variables would be even more relevant, when studies would include participants who already have a job and are on long-term sick leave due to their mental illness. All included studies targeted participants who were looking for a job, and interventions supporting participants returning to their job after a long sickness absence while considering cognitive functioning, appear to be missing.
Study differences
Even though the included studies all applied SE and analyzed predictors of its success, there were substantial differences in terms of the interventions, follow-up periods, diagnostic groups, outcome measures, neuropsychological tests, and included covariates. This shows that there are a variety of applications and approaches (including a measure of cognitive functioning), but it also makes it difficult to compare results and draw conclusions from the small number of studies. Moreover, the samples came from four different countries, and the results need to be considered in terms of the labor market and social security services of each country. Another point to consider is that articles used different alpha levels to indicate significant results due to multiple testing or large sample sizes, which affects the interpretation of significant vs. non-significant results in this review.
Limitations
Although we performed a systematic literature search using a wide range of different keywords and added a second, even broader search, our searching approach was limited to PubMed and PsychInfo and to the reference lists of included articles. Given the small number of resulting study samples, an additional search of other databases, such as Academic Search Premiere or Google Scholar, could have contributed to an even broader scope of this review. In addition, we did not search for gray literature. Another limitation concerns study selection, such that a few studies that fit the inclusion criteria did not further specify their sample’s diagnoses so that it was unclear if people with major depressive disorder were included at all (84–86). For instance, we decided not to include a study by Gold et al. (84), because the small subsample of participants with affective disorders was described as having “most often bipolar disorder.” Thus, the final number of participants with major depressive disorder remains unclear, and it could as well have been argued to include the study. Even in the included articles, precise information on the numbers of participants with depression was sometimes not available because affective disorders were grouped together (50, 51). Therefore, we could only estimate the total number of participants with major depressive disorder using data from the same baseline sample by McGurk et al. (49). Since the articles were based on samples with very different sample sizes and percentages of participants with major depressive disorder, no firm conclusions can be drawn from their results regarding the population of people with depression. A last point to keep in mind is that we decided to include several articles based on the same samples to reflect the full breadth of current research on our topic. In interpreting the study results, the findings of five articles drawn from only two samples should not be overestimated, even though one of these samples was particularly large.
Conclusion
This scoping review identified eight articles (from five samples) that examined the role of objectively measured cognitive functioning in vocational rehabilitation intervention outcomes and included participants with major depressive disorder. The included articles examined cognitive predictors in the context of recent IPS or SE trials, respectively, in North America and Europe with varying add-on interventions, research questions, outcomes, and covariates. Although major depression in particular or diagnostic differences were not focused, the articles suggest that higher cognitive functioning predicts better work related outcomes, similar to findings in schizophrenia. Thus, additional neuropsychological modules during vocational programs might further improve work-related outcomes for people with depression. However, as most studies did not include control participants who did not receive an intervention, the interplay between cognitive performance and the vocational rehabilitation intervention regarding work success remains unclear. Future research may also consider to include depression related covariates and broader outcomes, and examine their interactions with neuropsychological measures. Evidence that global measures of cognition, as well as certain subdomains have a significant impact on certain vocational outcomes also requires further investigation in individuals with major depressive disorder. More focus could be given to individual workplaces and their interactions with differently defined subjective and objective cognitive deficits and varying rehabilitation outcomes.
Data availability statement
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
JB and LD conceptualized the review, searched and screened articles, and extracted data from the included articles. PS was involved in the literature search and screening process. JB prepared the initial draft of the manuscript, which was revised by LD. MD and TB participated in the interpretation of the results and critically reviewed the manuscript draft. All authors read and approved the final version of the manuscript.
Funding
We acknowledge the financial support of the German Research Foundation (DFG) and the Open Access Publication Fund of Bielefeld University for the article processing charge.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Wittchen HU, Jacobi F, Rehm J, Gustavsson A, Svensson M, Jönsson B, et al. The size and burden of mental disorders and other disorders of the brain in europe 2010. Eur Neuropsychopharmacol. (2011) 21:655–79. doi: 10.1016/j.euroneuro.2011.07.018
2. Gbd 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 Diseases and Injuries, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet. (2016) 388:1545–602. doi: 10.1016/s0140-6736(16)31678-6
3. Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity? J Occupat Environ Med. (2008) 50:401–10. doi: 10.1097/JOM.0b013e31816bae50
4. Evans-Lacko S, Knapp M. Global patterns of workplace productivity for people with depression: Absenteeism and presenteeism costs across eight diverse countries. Soc Psychiatry Psychiatr Epidemiol. (2016) 51:1525–37. doi: 10.1007/s00127-016-1278-4
5. Greenberg PE, Fournier AA, Sisitsky T, Simes M, Berman R, Koenigsberg SH, et al. The economic burden of adults with major depressive disorder in the united states (2010 and 2018). PharmacoEconomics. (2021) 39:653–65. doi: 10.1007/s40273-021-01019-4
6. Wedegaertner F, Arnhold-Kerri S, Sittaro NA, Bleich S, Geyer S, Lee WE. Depression- and anxiety-related sick leave and the risk of permanent disability and mortality in the working population in germany: A cohort study. BMC Public Health. (2013) 13:145. doi: 10.1186/1471-2458-13-145
7. Amiri S, Behnezhad S. Depression and risk of disability pension: A systematic review and meta-analysis. Int J Psychiatry Med. (2019):91217419837412. doi: 10.1177/0091217419837412
8. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Virginia: American Psychiatric Association (2013).
9. World Health Organization. Icd-11: International Classification of Diseases (11th Revision). Geneva: World Health Organization (2019).
10. McIntyre RS, Soczynska JZ, Woldeyohannes HO, Alsuwaidan MT, Cha DS, Carvalho AF, et al. The impact of cognitive impairment on perceived workforce performance: Results from the international mood disorders collaborative project. Compr Psychiatry. (2015) 56:279–82. doi: 10.1016/j.comppsych.2014.08.051
11. Rock PL, Roiser JP, Riedel WJ, Blackwell AD. Cognitive impairment in depression: A systematic review and meta-analysis. Psychol Med. (2014) 44:2029–40. doi: 10.1017/s0033291713002535
12. Ahern E, Semkovska M. Cognitive functioning in the first-episode of major depressive disorder: A systematic review and meta-analysis. Neuropsychology. (2017) 31:52–72. doi: 10.1037/neu0000319
13. Semkovska M, Quinlivan L, O’Grady T, Johnson R, Collins A, O’Connor J, et al. Cognitive function following a major depressive episode: A systematic review and meta-analysis. Lancet Psychiatry. (2019) 6:851–61. doi: 10.1016/s2215-0366(19)30291-3
14. Conradi HJ, Ormel J, de Jonge P. Presence of individual (Residual) symptoms during depressive episodes and periods of remission: A 3-Year Prospective Study. Psychol Med. (2011) 41:1165–74. doi: 10.1017/s0033291710001911
15. Israel JA. The impact of residual symptoms in major depression. Pharmaceuticals. (2010) 3:2426–40. doi: 10.3390/ph3082426
16. Cambridge OR, Knight MJ, Mills N, Baune BT. The clinical relationship between cognitive impairment and psychosocial functioning in major depressive disorder: A systematic review. Psychiatry Res. (2018) 269:157–71. doi: 10.1016/j.psychres.2018.08.033
17. Evans VC, Iverson GL, Yatham LN, Lam RW. The relationship between neurocognitive and psychosocial functioning in major depressive disorder: A systematic review. J Clin Psychiatry. (2014) 75:1359–70. doi: 10.4088/JCP.13r08939
18. Knight MJ, Lyrtzis E, Baune BT. The association of cognitive deficits with mental and physical quality of life in major depressive disorder. Compr Psychiatry. (2020) 97:152147. doi: 10.1016/j.comppsych.2019.152147
19. Papakostas GI. Cognitive symptoms in patients with major depressive disorder and their implications for clinical practice. J Clin Psychiatry. (2014) 75:8–14. doi: 10.4088/JCP.13r08710
20. Clark M, DiBenedetti D, Perez V. Cognitive dysfunction and work productivity in major depressive disorder. Exp Rev Pharmacoeconom Outcomes Res. (2016) 16:455–63. doi: 10.1080/14737167.2016.1195688
21. Woo YS, Rosenblat JD, Kakar R, Bahk WM, McIntyre RS. Cognitive deficits as a mediator of poor occupational function in remitted major depressive disorder patients. Clin Psychopharmacol Neurosci. (2016) 14:1–16. doi: 10.9758/cpn.2016.14.1.1
22. Nieuwenhuijsen K, Verbeek JH, Neumeyer-Gromen A, Verhoeven AC, Bültmann U, Faber B. Interventions to improve return to work in depressed people. Cochrane Database Syst Rev. (2020) 10:Cd006237. doi: 10.1002/14651858.CD006237.pub4
23. Becker DR, Drake RE. A Working Life for People with Severe Mental Illness. Oxford: Oxford University Press (2003).
24. Suijkerbuijk YB, Schaafsma FG, van Mechelen JC, Ojajärvi A, Corbière M, Anema JR. Interventions for obtaining and maintaining employment in adults with severe mental illness, a network meta-analysis. Cochrane Database Syst Rev. (2017) 9:Cd011867. doi: 10.1002/14651858.CD011867.pub2
25. Becker RE, Meisler N, Stormer G, Brondino MJ. Employment outcomes for clients with severe mental illness in a pact model replication. Psychiatric Serv. (1999) 50:104–6. doi: 10.1176/ps.50.1.104
26. Allott KA, Cotton SM, Chinnery GL, Baksheev GN, Massey J, Sun P, et al. The relative contribution of neurocognition and social cognition to 6-month vocational outcomes following individual placement and support in first-episode psychosis. Schizophr Res. (2013) 150:136–43. doi: 10.1016/j.schres.2013.07.047
27. Bell MD, Bryson G. Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophr Bull. (2001) 27:269–79. doi: 10.1093/oxfordjournals.schbul.a006873
28. Karambelas GJ, Cotton SM, Farhall J, Killackey E, Allott KA. Contribution of neurocognition to 18-month employment outcomes in first-episode psychosis. Early Interv Psychiatry. (2019) 13:453–60. doi: 10.1111/eip.12504
29. McGurk SR, Mueser KT. Cognitive and clinical predictors of work outcomes in clients with schizophrenia receiving supported employment services: 4-Year Follow-Up. Adm Policy Ment Health. (2006) 33:598–606. doi: 10.1007/s10488-006-0070-2
30. McGurk SR, Mueser KT. Cognitive functioning, symptoms, and work in supported employment: A review and heuristic model. Schizophr Res. (2004) 70:147–73. doi: 10.1016/j.schres.2004.01.009
31. McGurk SR, Mueser KT. Cognitive functioning and employment in severe mental illness. J Nerv Ment Dis. (2003) 191:789–98. doi: 10.1097/01.nmd.0000100921.31489.5a
32. Tsang HW, Leung AY, Chung RC, Bell M, Cheung WM. Review on vocational predictors: A systematic review of predictors of vocational outcomes among individuals with schizophrenia: An Update since 1998. Aust N Z J Psychiatry. (2010) 44:495–504. doi: 10.3109/00048671003785716
33. Wexler BE, Bell MD. Cognitive remediation and vocational rehabilitation for schizophrenia. Schizophr Bull. (2005) 31:931–41. doi: 10.1093/schbul/sbi038
34. Bell MD, Bryson GJ, Greig TC, Fiszdon JM, Wexler BE. Neurocognitive enhancement therapy with work therapy: Productivity outcomes at 6- and 12-month follow-ups. J Rehabil Res Dev. (2005) 42:829–38. doi: 10.1682/jrrd.2005.03.0061
35. Bell MD, Zito W, Greig T, Wexler BE. Neurocognitive enhancement therapy with vocational services: Work outcomes at two-year follow-up. Schizophr Res. (2008) 105:18–29. doi: 10.1016/j.schres.2008.06.026
36. Lindenmayer JP, McGurk SR, Mueser KT, Khan A, Wance D, Hoffman L, et al. A randomized controlled trial of cognitive remediation among inpatients with persistent mental illness. Psychiatr Serv. (2008) 59:241–7. doi: 10.1176/ps.2008.59.3.241
37. McGurk SR, Mueser KT, Pascaris A. Cognitive training and supported employment for persons with severe mental illness: One-Year results from a randomized controlled trial. Schizophr Bull. (2005) 31:898–909. doi: 10.1093/schbul/sbi037
38. McGurk SR, Mueser KT, Feldman K, Wolfe R, Pascaris A. Cognitive training for supported employment: 2-3 year outcomes of a randomized controlled trial. Am J Psychiatry. (2007) 164:437–41. doi: 10.1176/ajp.2007.164.3.437
39. Rodríguez Pulido F, Caballero Estebaranz N, González Dávila E, Melián Cartaya MJ. Cognitive remediation to improve the vocational outcomes of people with severe mental illness. Neuropsychol Rehabil. (2021) 31:293–315. doi: 10.1080/09602011.2019.1692671
40. Tse S, Chan S, Ng KL, Yatham LN. Meta-Analysis of predictors of favorable employment outcomes among individuals with bipolar disorder. Bipolar Disord. (2014) 16:217–29. doi: 10.1111/bdi.12148
41. Grauwmeijer E, Heijenbrok-Kal MH, Haitsma IK, Ribbers GMA. Prospective study on employment outcome 3 years after moderate to severe traumatic brain injury. Arch Phys Med Rehabil. (2012) 93:993–9. doi: 10.1016/j.apmr.2012.01.018
42. Lillefjell M, Krokstad S, Espnes GA. Factors predicting work ability following multidisciplinary rehabilitation for chronic musculoskeletal pain. J Occupat Rehabil. (2006) 16:543–55. doi: 10.1007/s10926-005-9011-2
43. Barch DM. Neuropsychological abnormalities in schizophrenia and major mood disorders: Similarities and Differences. Curr Psychiatry Rep. (2009) 11:313–9. doi: 10.1007/s11920-009-0045-6
44. Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synth. (2020) 18:2119–26. doi: 10.11124/jbies-20-00167
45. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. Prisma extension for scoping reviews (Prisma-Scr): Checklist and Explanation. Ann Internal Med. (2018) 169:467–73. doi: 10.7326/m18-0850
46. Corbière M, Lecomte T, Reinharz D, Kirsh B, Goering P, Menear M, et al. Predictors of acquisition of competitive employment for people enrolled in supported employment programs. J Nerv Ment Dis. (2017) 205:275–82. doi: 10.1097/nmd.0000000000000612
47. Landolt K, Brantschen E, Nordt C, Bärtsch B, Kawohl W, Rössler W. Association of supported employment with cognitive functioning and employment outcomes. Psychiatric Serv. (2016) 67:1257–61. doi: 10.1176/appi.ps.201500183
48. Mahmood Z, Keller AV, Burton CZ, Vella L, Matt GE, McGurk SR, et al. Modifiable predictors of supported employment outcomes among people with severe mental illness. Psychiatric Serv. (2019) 70:782–92. doi: 10.1176/appi.ps.201800562
49. McGurk SR, Drake RE, Xie H, Riley J, Milfort R, Hale TW, et al. Cognitive predictors of work among social security disability insurance beneficiaries with psychiatric disorders enrolled in ips supported employment. Schizophr Bull. (2018) 44:32–7. doi: 10.1093/schbul/sbx115
50. Metcalfe JD, Drake RE, Bond GR. Predicting employment in the mental health treatment study: Do Client Factors Matter? Adm Policy Ment Health. (2017) 44:345–53. doi: 10.1007/s10488-016-0774-x
51. Metcalfe JD, Riley J, McGurk S, Hale T, Drake RE, Bond GR. Comparing predictors of employment in individual placement and support: A longitudinal analysis. Psychiatry Res. (2018) 264:85–90. doi: 10.1016/j.psychres.2018.03.050
52. Burton CZ, Vella L, Twamley EW. Prospective memory, level of disability, and return to work in severe mental illness. Clin Neuropsychol. (2019) 33:594–605. doi: 10.1080/13854046.2018.1436725
53. Rössler W, Ujeyl M, Kawohl W, Nordt C, Lasalvia A, Haker H, et al. Predictors of employment for people with mental illness: Results of a multicenter randomized trial on the effectiveness of placement budgets for supported employment. Front Psychiatry. (2019) 10:518. doi: 10.3389/fpsyt.2019.00518
54. Drake RE, Frey W, Bond GR, Goldman HH, Salkever D, Miller A, et al. Assisting Social security disability insurance beneficiaries with schizophrenia, bipolar disorder, or major depression in returning to work. Am J Psychiatry. (2013) 170:1433–41. doi: 10.1176/appi.ajp.2013.13020214
55. Twamley EW, Thomas KR, Burton CZ, Vella L, Jeste DV, Heaton RK, et al. Compensatory cognitive training for people with severe mental illnesses in supported employment: A randomized controlled trial. Schizophr Res. (2019) 203:41–8. doi: 10.1016/j.schres.2017.08.005
56. Corbière M, Lanctôt N, Lecomte T, Latimer E, Goering P, Kirsh B, et al. A Pan-Canadian evaluation of supported employment programs dedicated to people with severe mental disorders. Commun Ment Health J. (2010) 46:44–55. doi: 10.1007/s10597-009-9207-6
57. Christensen TN, Wallstrøm IG, Stenager E, Bojesen AB, Gluud C, Nordentoft M, et al. Effects of individual placement and support supplemented with cognitive remediation and work-focused social skills training for people with severe mental illness: A randomized clinical trial. JAMA Psychiatry. (2019) 76:1232–40. doi: 10.1001/jamapsychiatry.2019.2291
58. Christensen TN, Wallstrøm IG, Bojesen AB, Nordentoft M, Eplov LF. Predictors of work and education among people with severe mental illness who participated in the danish individual placement and support study: Findings from a randomized clinical trial. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1669–77. doi: 10.1007/s00127-021-02107-8
59. Keefe RS, Goldberg TE, Harvey PD, Gold JM, Poe MP, Coughenour L. The brief assessment of cognition in schizophrenia: reliability, sensitivity, and comparison with a standard neurocognitive battery. Schizophr Res. (2004) 68:283–97. doi: 10.1016/j.schres.2003.09.011
60. Corrigan PW, McCracken SG. Place first, then train: an alternative to the medical model of psychiatric rehabilitation. Soc Work. (2005) 50:31–9. doi: 10.1093/sw/50.1.31
61. McIntyre RS, Cha DS, Soczynska JK, Woldeyohannes HO, Gallaugher LA, Kudlow P, et al. Cognitive deficits and functional outcomes in major depressive disorder: determinants, substrates, and treatment interventions. Depress Anxiety. (2013) 30:515–27. doi: 10.1002/da.22063
62. Hellström L, Pedersen P, Christensen TN, Wallstroem IG, Bojesen AB, Stenager E, et al. Vocational outcomes of the individual placement and support model in subgroups of diagnoses, substance abuse, and forensic conditions: A systematic review and analysis of pooled original data. J Occupat Rehabil. (2021) 31:699–710. doi: 10.1007/s10926-021-09960-z
63. Bejerholm U, Larsson ME, Johanson S. Supported employment adapted for people with affective disorders-a randomized controlled trial. J Affect Disord. (2017) 207:212–20. doi: 10.1016/j.jad.2016.08.028
64. Douglas KM, Gallagher P, Robinson LJ, Carter JD, McIntosh VV, Frampton CM, et al. Prevalence of cognitive impairment in major depression and bipolar disorder. Bipolar Disord. (2018) 20:260–74. doi: 10.1111/bdi.12602
65. Porter RJ, Bourke C, Gallagher P. Neuropsychological impairment in major depression: Its nature, origin and clinical significance. Aust N Z J Psychiatry. (2007) 41:115–28. doi: 10.1080/00048670601109881
66. Porter RJ, Robinson LJ, Malhi GS, Gallagher P. The neurocognitive profile of mood disorders – a review of the evidence and methodological issues. Bipolar Disord. (2015) 17(Suppl 2):21–40. doi: 10.1111/bdi.12342
67. Beblo T, Sinnamon G, Baune BT. Specifying the neuropsychology of affective disorders: Clinical, demographic and neurobiological factors. Neuropsychol Rev. (2011) 21:337–59. doi: 10.1007/s11065-011-9171-0
68. Evans JD, Bond GR, Meyer PS, Kim HW, Lysaker PH, Gibson PJ, et al. Cognitive and clinical predictors of success in vocational rehabilitation in schizophrenia. Schizophr Res. (2004) 70:331–42. doi: 10.1016/j.schres.2004.01.011
69. Caruana E, Cotton S, Killackey E, Allott K. The relationship between cognition, job complexity, and employment duration in first-episode psychosis. Psychiatr Rehabil J. (2015) 38:210–7. doi: 10.1037/prj0000129
70. Ikebuchi E, Sato S, Yamaguchi S, Shimodaira M, Taneda A, Hatsuse N, et al. Does improvement of cognitive functioning by cognitive remediation therapy effect work outcomes in severe mental illness? A secondary analysis of a randomized controlled trial. Psychiatry Clin Neurosci. (2017) 71:301–8. doi: 10.1111/pcn.12486
71. Johansen T, Øyeflaten I, Eriksen HR, Lyby PS, Dittrich WH, Holsen I, et al. Sustained attention and working memory predict the number of days on health-related benefits in the year following occupational rehabilitation. J Occupat Rehabil. (2021) 31:592–603. doi: 10.1007/s10926-020-09944-5
72. Knight MJ, Air T, Baune BT. The role of cognitive impairment in psychosocial functioning in remitted depression. J Affect Disord. (2018) 235:129–34. doi: 10.1016/j.jad.2018.04.051
73. Mohn C, Rund BR. Neurocognitive profile in major depressive disorders: relationship to symptom level and subjective memory complaints. BMC Psychiatry. (2016) 16:108. doi: 10.1186/s12888-016-0815-8
74. Lahr D, Beblo T, Hartje W. Cognitive performance and subjective complaints before and after remission of major depression. Cogn Neuropsychiatry. (2007) 12:25–45. doi: 10.1080/13546800600714791
75. Petersen JZ, Porter RJ, Miskowiak KW. Clinical characteristics associated with the discrepancy between subjective and objective cognitive impairment in depression. J Affect Disord. (2019) 246:763–74. doi: 10.1016/j.jad.2018.12.105
76. Dehn LB, Beblo T. Are they just exaggerating? differences between subjective and objective cognitive performance in patients with depression: mounting evidence and open questions. J Affect Disord. (2019) 248:198–9. doi: 10.1016/j.jad.2018.05.082
77. Tran T, Milanovic M, Holshausen K, Bowie CR. What is normal cognition in depression? Prevalence and functional correlates of normative versus idiographic cognitive impairment. Neuropsychology. (2021) 35:33–41. doi: 10.1037/neu0000717
78. Douglas KM, Porter RJ, Frampton CM, Gallagher P, Young AH. Abnormal response to failure in unmedicated major depression. J Affect Disord. (2009) 119:92–9. doi: 10.1016/j.jad.2009.02.018
79. Beblo T, Mensebach C, Wingenfeld K, Schlosser N, Rullkoetter N, Schaffrath C, et al. The impact of neutral and emotionally negative distraction on memory performance and its relation to memory complaints in major depression. Psychiatry Res. (2010) 178:106–11. doi: 10.1016/j.psychres.2009.04.012
80. Donaldson C, Lam D, Mathews A. Rumination and attention in major depression. Behav Res Ther. (2007) 45:2664–78. doi: 10.1016/j.brat.2007.07.002
81. Peckham AD, McHugh RK, Otto MW. A Meta-Analysis of the magnitude of biased attention in depression. Depress Anxiety. (2010) 27:1135–42. doi: 10.1002/da.20755
82. Scheurich A, Fellgiebel A, Schermuly I, Bauer S, Wölfges R, Müller MJ. Experimental evidence for a motivational origin of cognitive impairment in major depression. Psychol Med. (2008) 38:237–46. doi: 10.1017/s0033291707002206
83. Grahek I, Shenhav A, Musslick S, Krebs RM, Koster EHW. Motivation and cognitive control in depression. Neurosci Biobehav Rev. (2019) 102:371–81. doi: 10.1016/j.neubiorev.2019.04.011
84. Gold JM, Goldberg RW, McNary SW, Dixon LB, Lehman AF. Cognitive correlates of job tenure among patients with severe mental illness. Am J Psychiatry. (2002) 159:1395–402. doi: 10.1176/appi.ajp.159.8.1395
85. Johansen T, Jensen C, Eriksen HR, Lyby PS, Dittrich WH, Holsen IN, et al. Occupational rehabilitation is associated with improvements in cognitive functioning. Front Psychol. (2019) 10:2233. doi: 10.3389/fpsyg.2019.02233
Keywords: supported employment (SE), cognitive function, depression, work, neuropsychology
Citation: Bergdolt J, Sellin P, Driessen M, Beblo T and Dehn LB (2022) Neuropsychological predictors of vocational rehabilitation outcomes in individuals with major depression: A scoping review. Front. Psychiatry 13:942161. doi: 10.3389/fpsyt.2022.942161
Received: 12 May 2022; Accepted: 21 October 2022;
Published: 09 November 2022.
Edited by:
Emre Umucu, Michigan State University, United StatesReviewed by:
Jessica Marie Brooks, Columbia University, United StatesTeresa Grenawalt, The University of Alabama, United States
Copyright © 2022 Bergdolt, Sellin, Driessen, Beblo and Dehn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lorenz B. Dehn, lorenz.dehn@evkb.de
 Juliane Bergdolt1
Juliane Bergdolt1 Thomas Beblo
Thomas Beblo Lorenz B. Dehn
Lorenz B. Dehn