Complementary Feeding Practices and Parental Pressure to Eat among Spanish Infants and Toddlers: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Questionnaire
2.2.1. Demographic Characteristics
2.2.2. Complementary Feeding Practices
2.2.3. Parental Pressure to Eat
2.3. Data Analysis
3. Results
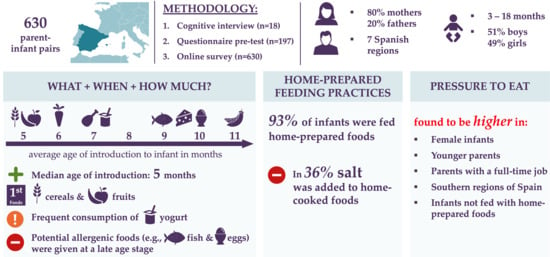
3.1. Demographic Characteristics
3.2. Complementary Feeding Practices
3.2.1. Timing of Introduction
3.2.2. Frequency of Intake
3.2.3. Home-Prepared Feeding Practices
3.3. Pressure to Eat
3.4. Associations between Sample Characteristics, Feeding Practices and Pressure to Eat
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Caprio, S.; Santoro, N.; Weiss, R. Childhood obesity and the associated rise in cardiometabolic complications. Nat. Metab. 2020, 2, 223–232. [Google Scholar] [CrossRef] [PubMed]
- Narzisi, K.; Simons, J. Interventions that prevent or reduce obesity in children from birth to five years of age: A systematic review. J. Child Health Care 2020, 1367493520917863. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pérez-Farinós, N.; Lopez-Sobaler, A.M.; Dal Re, M.A.; Villar, C.; Labrado, E.; Robledo, T.; Ortega, R.M. The ALADINO Study: A National Study of Prevalence of Overweight and Obesity in Spanish Children in 2011. BioMed Res. Int. 2013, 163687. [Google Scholar] [CrossRef]
- Sánchez-Cruz, J.-J.; Jiménez-Moleón, J.J.; Fernández-Quesadad, F.; Sáncheza, M.J. Prevalencia de obesidad infantil y juvenil en España en 2012. Rev. Esp. Cardiol. 2014, 66, 371–376. [Google Scholar] [CrossRef]
- Aranceta-Bartrina, J.; Pérez-Rodrigo, C. La obesidad infantil: Una asignatura pendiente. Rev. Esp. Cardiol. 2018, 71, 888–891. [Google Scholar] [CrossRef]
- Agencia Española de Seguridad Alimentaria y Nutrición (AESAN): Estudio Aladino 2019: Estudio sobre Alimentación, Actividad Física, Desarrollo Infantil y Obesidad en España 2019. Available online: https://www.aesan.gob.es/AECOSAN/docs/documentos/nutricion/observatorio/Informe_Aladino_2019.pdf (accessed on 5 January 2021).
- Spinelli, A.; Buoncristiano, M.; Kovacs, V.A.; Yngve, A.; Spiroski, I.; Obreja, G.; Sant′Angelo, V.F. Prevalence of severe obesity among primary school children in 21 European countries. Obes. Facts 2009, 12, 244–258. [Google Scholar] [CrossRef]
- Schwartz, C.; Scholtens, P.A.M.J.; Lalanne, A.; Weenen, H.; Nicklaus, S. Development healthy eating habits early in life. Review of recent evidence and selected guidelines. Appetite 2011, 57, 796–807. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.; Fall, C. Infant nutrition and later health: A review of current evidence. Nutrients 2012, 4, 859–874. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization (WHO). Infant and Young Child Nutrition: Global Strategy on Infant and Young Child Feeding; World Health Organization, Fifty Fifth World Health Assembly: Geneva, Switzerland, 2002. [Google Scholar]
- D’Auria, E.; Borsani, B.; Pendezza, E.; Bosetti, A.; Paradiso, L.; Zuccotti, G.V.; Verduci, E. Complementary feeding: Pitfalls for health outcomes. Int. J. Environ. Res. Public Health 2020, 17, 7931. [Google Scholar] [CrossRef]
- Nicklaus, S. Children′s acceptance of new foods at weaning. Role of practices of weaning and of food sensory properties. Appetite 2011, 57, 812–815. [Google Scholar] [CrossRef]
- Maier-Nöth, A.; Schaal, B.; Leathwood, P.; Issanchou, S. The lasting influences of early food-related variety experience: A longitudinal study of vegetable acceptance from 5 months to 6 years in two populations. PLoS ONE 2016, 11, e0151356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mennella, J.A.; Beauchamp, G.K. The role of early life experiences in flavor perception and delight. In Obesity Prevention, 1st ed.; Dubé, L., Bechara, A., Dagher, A., Drewnowski, A., Eds.; Elsevier Inc.: Philadelphia, PA, USA, 2010; pp. 203–217. [Google Scholar] [CrossRef]
- Nicklaus, S.; Remy, E. Early origins of overeating: Tracking between early food habits and later eating patterns. Curr. Obes. Rep. 2013, 2, 179–184. [Google Scholar] [CrossRef] [Green Version]
- Nicklaus, S. The role of food experiences during early childhood in food pleasure learning. Appetite 2016, 104, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Switkowski, K.M.; Gingras, V.; Rifas-Shiman, S.L.; Oken, E. Patterns of Complementary Feeding Behaviors Predict Diet Quality in Early Childhood. Nutrients 2020, 12, 810. [Google Scholar] [CrossRef] [Green Version]
- Pan American Health Organization and World Health Organization (PAHO & WHO). Guiding Principles for Complementary Feeding of the Breastfed; World Health Organization: Washington, DC, USA, 2001. [Google Scholar]
- Agostoni, C.; Decsi, T.; Fewtrell, M.; Goulet, O.; Kolacek, S.; Koletzko, B.; Michaelsen, K.F.; Moreno, L.; Puntis, J.; Rigo, J.; et al. Complementary feeding: A commentary by the ESPGHAN Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2008, 46, 99–110. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellöf, M.; Embleton, N.; Mis, N.F.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary feeding: A position paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on nutrition. J. Pediatr. Gastroenterol. Nutr. 2007, 64, 119–132. [Google Scholar] [CrossRef]
- EFSA Panel on Nutrition, Novel Foods and Food Allergens (NDA); Castenmiller, J.; de Henauw, S.; Hirsch-Ernst, K.I.; Kearney, J.; Knutsen, H.K.; Maciuk, A.; Mangelsdorf, I.; McArdle, H.J.; Naska, A.; et al. Appropriate age range for introduction of complementary feeding into an infant’s diet. EFSA J. 2019, 17, e05780. [Google Scholar] [CrossRef] [Green Version]
- Koletzko, B.; Hirsch, N.L.; Jewell, J.M.; Dos Santos, Q.; Breda, J.; Fewtrell, M.; Weber, M.W. National Recommendations for Infant and Young Child Feeding in the World Health Organization European Region. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 672. [Google Scholar] [CrossRef] [PubMed]
- Alder, E.M.; Williams, F.L.R.; Anderson, A.S.; Forsyth, S.; Florey, C.D.V.; van der Velde, P. What influences the timing of the introduction of solid food to infants? Br. J. Nutr. 2004, 92, 527. [Google Scholar] [CrossRef] [Green Version]
- Costantini, C.; Harris, G.; Reddy, V.; Akehurst, L.; Fasulo, A. Introducing complementary foods to infants: Does age really matter? A look at feeding practices in two European communities: British and Italian. Child Care Pract. 2018, 25, 1–16. [Google Scholar] [CrossRef]
- Foterek, K.; Hilbig, A.; Alexy, U. Breast-feeding and weaning practices in the DONALD Study. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 361–367. [Google Scholar] [CrossRef] [PubMed]
- White, J.M.; Bégin, F.; Kumapley, R.; Murray, C.; Krasevec, J. Complementary feeding practices: Current global and regional estimates. Matern. Child Nutr. 2017, 13, e12505. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Netting, M.J.; Makrides, M. Complementary foods: Guidelines and practices. In Complementary Feeding: Building the Foundations for a Healthy Life; Black, R.E., Makrides, M., Ong, K.K., Eds.; Karger Publishers: Basel, Switzerland, 2017; pp. 1–12. [Google Scholar] [CrossRef] [Green Version]
- Domellöf, M.; Braegger, C.; Campoy, C.; Colomb, V.; Decsi, T.; Fewtrell, M.; Hojsak, I.; Mihatsch, W.; Molgaard, C.; Shamir, R.; et al. Iron requirements of infants and toddlers. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 119–129. [Google Scholar] [CrossRef]
- Asociación Española de Pediatría (AEP). Manual Práctico de Nutrición en Pediatría; AEP Asociación Española de Pediatría: Madrid, Spain, 2007. [Google Scholar]
- Asociación Española de Pediatría (AEP). Recomendaciones de la Asociación Española de Pediatría Sobre la Alimentación Complementaria; Comité de Lactancia Materna y Comité de Nutrición de la Asociación Española de Pediatría, AEP Asociación Española de Pediatría: Madrid, Spain, 2018. [Google Scholar]
- World Health Organization (WHO): Infant and Young Child Feeding. Available online: https://www.who.int/en/news-room/fact-sheets/detail/infant-and-youngchild-feeding (accessed on 5 January 2021).
- Burns, J.; Emerson, J.A.; Amundson, K.; Doocy, S.; Caulfield, L.E.; Klemm, R.D.W. A qualitative analysis of barriers and facilitators to optimal breastfeeding and complementary feeding practices in South Kivu, Democratic Republic of Congo. Food Nutr. Bull. 2016, 37, 119–131. [Google Scholar] [CrossRef] [PubMed]
- Egyir, B.K.; Ramsay, S.A.; Bilderback, B.; Safaii, S.A. Complementary feeding practices of mothers and their perceived impacts on young children: Findings from KEEA district of Ghana. Matern. Child Health J. 2016, 20, 1886–1894. [Google Scholar] [CrossRef] [PubMed]
- Issaka, A.I.; Agho, K.E.; Page, A.N.; Burns, P.L.; Stevens, G.J.; Dibley, M.J. Determinants of suboptimal complementary feeding practices among children aged 6-23 months in seven francophone West African countries. Matern. Child Nutr. 2015, 11, 31–52. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W.; Madise, N.J.; Fotso, J.-C.; Kyobutungi, C.; Mutua, M.K.; Gitau, T.M.; Yatich, N. Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health 2011, 11, 396. [Google Scholar] [CrossRef] [Green Version]
- Vaahtera, M.; Kulmala, T.; Hietanen, A.; Ndekha, M.; Cullinan, T.; Salin, M.L.; Ashorn, P. Breastfeeding and complementary feeding practices in rural Malawi. Acta Paediatr. 2001, 90, 328–332. [Google Scholar] [CrossRef] [PubMed]
- Duong, D.V.; Binns, C.W.; Lee, A.H. Introduction of complementary food to infants within the first six months postpartum in rural Vietnam. Acta Paediatr. 2005, 94, 1714–1720. [Google Scholar] [CrossRef]
- Gardner, H.; Green, K.; Gardner, A. Infant feeding practices of Emirati women in the rapidly developing city of Abu Dhabi, United Arab Emirates. Int. J. Environ. Res. Public Health 2015, 12, 10923–10940. [Google Scholar] [CrossRef] [Green Version]
- Radwan, H. Patterns and determinants of breastfeeding and complementary feeding practices of Emirati Mothers in the United Arab Emirates. BMC Public Health 2013, 13, 171. [Google Scholar] [CrossRef] [Green Version]
- Friel, J.K.; Isaak, C.A.; Hanning, R.; Miller, A. Complementary food consumption of Canadian infants. Open Nutr. J. 2009, 3, 11–16. [Google Scholar] [CrossRef]
- Siega-Riz, A.M.; Deming, D.M.; Reidy, K.C.; Fox, M.K.; Condon, E.; Briefel, R.R. Food consumption patterns of infants and toddlers: Where are we now? J. Am. Diet. Assoc. 2010, 110, S38–S51. [Google Scholar] [CrossRef]
- Helle, C.; Hillesund, E.R.; Øverby, N.C. Timing of complementary feeding and associations with maternal and infant characteristics: A Norwegian cross-sectional study. PLoS ONE 2018, 13, e0199455. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, S.; Ludvigsson, J.; Brekke, H.K. Introduction of complementary foods in Sweden and impact of maternal education on feeding practices. Public Health Nutr. 2017, 20, 1054–1062. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kronborg, H.; Foverskov, E.; Vaeth, M. Predictors for early introduction of solid food among Danish mothers and infants: An observational study. BMC Pediatr. 2014, 14, 243. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lande, B.; Andersen, L.F.; Baerug, A.; Trygg, K.U.; Lund-Larsen, K.; Veierød, M.B.; Bjørneboe, G.E.A. Infant feeding practices and associated factors in the first six months of life: The Norwegian infant nutrition survey. Acta Paediatr. 2003, 92, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Carletti, C.; Pani, P.; Monasta, L.; Knowles, A.; Cattaneo, A. Introduction of complementary foods in a cohort of infants in Northeast Italy: Do parents comply with WHO Recommendations? Nutrients 2017, 9, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dratva, J.; Merten, S.; Ackermann-Liebrich, U. The timing of complementary feeding of infants in Switzerland: Compliance with the Swiss and the WHO guidelines. Acta Paediatr. 2006, 95, 818–825. [Google Scholar] [CrossRef] [PubMed]
- McAndrew, F.; Thompson, J.; Fellows, L.; Large, A.; Speed, M.; Renfrew, M.J. Infant Feeding Survey 2010; The Health and Social Care Information Centre: Leeds, UK, 2012.
- Giovannini, M.; Riva, E.; Banderali, G.; Scaglioni, S.; Veehof, S.; Sala, M.; Radaelli, G.; Agostoni, C. Feeding practices of infants through the first year of life in Italy. Acta Paediatr. 2004, 93, 492–497. [Google Scholar] [CrossRef] [PubMed]
- O′Donovan, S.M.; Murray, D.M.; Hourihane, J.O.; Kenny, L.C.; Irvine, A.D.; Kiely, M. Adherence with early infant feeding and complementary feeding guidelines in the Cork BASELINE Birth Cohort Study. Public Health Nutr. 2015, 18, 2864–2873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lange, C.; Visalli, M.; Jacob, S.; Chabanet, C.; Schlich, P.; Nicklaus, S. Maternal feeding practices during the first year and their impact on infants’ acceptance of complementary food. Food Qual. Prefer. 2013, 29, 89–98. [Google Scholar] [CrossRef]
- Schwartz, C.; Madrelle, J.; Vereijken, C.M.J.L.; Weenen, H.; Nicklaus, S.; Hetherington, M.M. Complementary feeding and “donner les bases du goût” (providing the foundation of taste). A qualitative approach to understand weaning practices, attitudes and experiences by French mothers. Appetite 2013, 71, 321–331. [Google Scholar] [CrossRef]
- Tarrant, R.C.; Younger, K.M.; Sheridan-Pereira, M.; White, M.J.; Kearney, J.M. Factors associated with weaning practices in term infants: A prospective observational study in Ireland. Br. J. Nutr. 2010, 104, 1544–1554. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rebhan, B.; Kohlhuber, M.; Schwegler, U.; Koletzko, B.V.; Fromme, H. Infant feeding practices and associated factors through the first 9 months of life in Bavaria, Germany. J. Pediatr. Gastroenterol. Nutr. 2009, 49, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Van Grieken, A.; Van Der Velde, L.A.; Vlasblom, E.; Beltman, M.; L′Hoir, M.P.; Boere-Boonekamp, M.M.; Raat, H. Factors associated with early introduction of complementary feeding and consumption of non-recommended foods among Dutch infants: The BeeBOFT study. BMC Public Health 2019, 19, 388. [Google Scholar] [CrossRef] [Green Version]
- Serra-Majem, L.; Ribas Barba, L.; Pérez-Rodrigo, C.; Roman Viñas, B.; Aranceta Bartrina, J. Hábitos alimentarios y consumo de alimentos en la población infantil y juvenil española (1998–2000): Variables socioeconómicas y geográficas. Med. Clín. 2003, 121, 126–131. [Google Scholar] [CrossRef]
- Díez-Gañán, L.; Galán Labaca, I.; Domínguez, C.M.L.; Gandarillas Grande, A.; Zorrilla Torras, B.; Cebrián, F.A. Ingesta de alimentos, energía y nutrientes en la población de 5 a 12 años de la Comunidad de Madrid: Resultados de la Encuesta de Nutrición Infantil 2001–2002. Rev. Esp. Salud Publica 2007, 81, 543–558. [Google Scholar] [CrossRef] [Green Version]
- Latorre-Millán, M.; Rupérez, A.I.; González-Gil, E.M.; Santaliestra-Pasías, A.; Vázquez-Cobela, R.; Gil Campos, M.; Aguilera, C.M.; Gil, Á.; Moreno, L.A.; Leis, R.; et al. Dietary Patterns and Their Association with Body Composition and Cardiometabolic Markers in Children and Adolescents: Genobox Cohort. Nutrients 2020, 12, 3424. [Google Scholar] [CrossRef]
- Dalmau, J.; Moráis, A.; Martínez, V.; Peña-Quintana, L.; Varea, V.; Martínez, M.J.; Soler, B. Evaluación de la alimentación y consumo de nutrientes en menores de 3 años. Estudio piloto ALSALMA. An. Pediatr. 2014, 81, 22–31. [Google Scholar] [CrossRef] [PubMed]
- Dalmau, J.; Peña-Quintana, L.; Moráis, A.; Martínez, V.; Varea, V.; Martínez, M.J.; Soler, B. Análisis cuantitativo de la ingesta de nutrientes en niños menores de 3 años. Estudio ALSALMA. An. Pediatr. 2015, 82, 255–266. [Google Scholar] [CrossRef]
- Agencia Española de Consumo, Seguridad Alimentaria y Nutrición (AECOSAN). ENALIA: Encuesta Nacional de Consumo de Alimentos en Población Infantil y Adolescente 2012–2015; Ministerio de Sanidad, Servicios Sociales e Igualdad: Madrid, Spain, 2017.
- López-Sobaler, A.M.; Aparicio, A.; González-Rodríguez, L.G.; Cuadrado-Soto, E.; Rubio, J.; Marcos, V.; Sanchidrián, R.; Santos, S.; Pérez-Farinós, N.; Re, M.Á.D.; et al. Adequacy of usual vitamin and mineral intake in Spanish children and adolescents: ENALIA study. Nutrients 2017, 9, 131. [Google Scholar] [CrossRef] [Green Version]
- Madrigal, C.; Soto-Méndez, M.J.; Leis, R.; Hernández-Ruiz, Á.; Valero, T.; Villoslada, F.L.; De Victoria, E.M.; Moreno, J.M.; Ortega, R.M.; Ruiz-López, M.D.; et al. Dietary Intake, Nutritional Adequacy and Food Sources of Total Fat and Fatty Acids, and Relationships with Personal and Family Factors in Spanish Children Aged One to < 10 Years: Results of the EsNuPI Study. Nutrients 2020, 12, 2467. [Google Scholar] [CrossRef]
- Thompson, A.L.; Mendez, M.A.; Borja, J.B.; Adair, L.S.; Zimmer, C.R.; Bentley, M.E. Development and validation of the infant feeding style questionnaire. Appetite 2009, 53, 210–221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ventura, A.K.; Birch, L.L. Does parenting affect children′s eating and weight status? Int. J. Behav. Nutr. Phys. Act. 2008, 5, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sacco, L.M.; Bentley, M.E.; Carby-Shields, K.; Borja, J.B.; Goldman, B.D. Assessment of infant feeding styles among low-income African-American mothers: Comparing reported and observed behaviors. Appetite 2007, 49, 131–140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiSantis, K.I.; Hodges, E.A.; Johnson, S.L.; Fisher, J.O. The role of responsive feeding in overweight during infancy and toddlerhood: A systematic review. Int. J. Obes. 2011, 35, 480–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ellis, J.M.; Galloway, A.T.; Webb, R.M.; Martz, D.M.; Farrow, C.V. Recollections of pressure to eat during childhood, but not picky eating, predict young adult eating behavior. Appetite 2016, 97, 58–63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodgers, R.F.; Paxton, S.J.; Massey, R.; Campbell, K.J.; Wertheim, E.H.; Skouteris, H.; Gibbons, K. Maternal feeding practices predict weight gain and obesogenic eating behaviors in young children: A prospective study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 24. [Google Scholar] [CrossRef] [Green Version]
- Thompson, A.L.; Adair, L.S.; Bentley, M.E. Pressuring and restrictive feeding styles influence infant feeding and size among a low-income African-American sample. Obesity 2013, 21, 562–571. [Google Scholar] [CrossRef] [Green Version]
- Bernal, M.J.; Román, S.; Klerks, M.; Iniesta, M.D.; Haro, J.F.; Bodenstab, S.; Sánchez-Siles, L.M. Elaboración de un instrumento para evaluar las prácticas de alimentación infantil en los primeros 18 meses de vida en España. Estudio HIDANS. [XVII Congreso de la Sociedad Española de Investigación en Nutrición y Alimentación en Pediatría (SEINAP), 6 y 7 de octubre de 2017]. Rev. Esp. Pediatr. 2017, 73, 261–263. [Google Scholar]
- Román, S.; Sánchez-Siles, L.M. Parents′ choice criteria for infant food brands: A scale development and validation. Food Qual. Prefer. 2018, 64, 1–10. [Google Scholar] [CrossRef]
- Baughcum, A.E.; Powers, S.W.; Johnson, S.B.; Chamberlin, L.A.; Deeks, C.M.; Jain, A.; Whitaker, R.C. Maternal feeding practices and beliefs and their relationships to overweight in early childhood. J. Dev. Behav. Pediatr. 2001, 22, 391–408. [Google Scholar] [CrossRef]
- Birch, L.L.; Fisher, J.O.; Grimm-Thomas, K.; Markey, C.N.; Sawyer, R.; Johnson, S.L. Confirmatory factor analysis of the Child Feeding Questionnaire: A measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite 2001, 36, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Llewellyn, C.H.; van Jaarsveld, C.H.M.; Johnson, L.; Carnell, S.; Wardle, J. Development and factor structure of the Baby Eating Behaviour Questionnaire in the Gemini birth cohort. Appetite 2011, 57, 388–396. [Google Scholar] [CrossRef]
- van den Boom, S.A.M.; Kimber, A.C.; Morgan, J.B. Weaning practices in children up to 19 months of age in Madrid. Acta Paediatr. 1995, 84, 853–858. [Google Scholar] [CrossRef]
- Beatty, P.; Willis, G.B. Research synthesis: The practice of cognitive interviewing. Public Opin. Q. 2007, 71, 287–311. [Google Scholar] [CrossRef] [Green Version]
- Dickin, K.L.; Larios, F.B.S.; Parra, P.A. Cognitive interviewing to enhance comprehension and accuracy of responses to a spanish-language nutrition program evaluation tool. J. Nutr. Educ. Behav. 2015, 47, 465–471. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). WHO Child Growth Standards: Length/Height-for-Age, Weight for-Age, Weight-for-Length, Weight-for-Height and Body Mass Index-for-Age: Methods and Development; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Bagozzi, R.P.; Yi, Y. On the evaluation of structural equation models. J. Acad. Mark. Sci. 1988, 16, 74–94. [Google Scholar] [CrossRef]
- Betoko, A.; Charles, M.A.; Hankard, R.; Forhan, A.; Bonet, M.; Saurel-Cubizolles, M.-J.J.; Heude, B.; De Lauzon-Guillain, B. Infant feeding patterns over the first year of life: Influence of family characteristics. Eur. J. Clin. Nutr. 2013, 67, 631–637. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fein, S.B.; Labiner-Wolfe, J.; Scanlon, K.S.; Grummer-Strawn, L.M. Selected complementary feeding practices and their association with maternal education. Pediatrics 2008, 122, S91–S97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matvienko-Sikar, K.; Kelly, C.; Sinnott, C.; McSharry, J.; Houghton, C.; Heary, C.; Toomey, E.; Byrne, M.; Kearney, P.M. Parental experiences and perceptions of infant complementary feeding: A qualitative evidence synthesis. Obes. Rev. 2018, 19, 501–517. [Google Scholar] [CrossRef] [PubMed]
- Khandpur, N.; Blaine, R.E.; Fisher, J.O.; Davison, K.K. Fathers′ child feeding practices: A review of the evidence. Appetite 2014, 78, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Litchford, A.; Roskos, M.R.S.; Wengreen, H. Influence of fathers on the feeding practices and behaviors of children: A systematic review. Appetite 2020, 147, 104558. [Google Scholar] [CrossRef]
- Köksal, E.; Yalçın, S.S.; Pekcan, G.; Özbaş, S.; Tezel, B.; Köse, M.R. Complementary feeding practices of children aged 12–23 Months in Turkey. Cent. Eur. J. Public Health 2015, 23, 149–154. [Google Scholar] [CrossRef] [Green Version]
- Maier, A.; Chabanet, C.; Schaal, B.; Leathwood, P.; Issanchou, S. Food-related sensory experience from birth through weaning: Contrasted patterns in two nearby Europeans regions. Appetite 2007, 49, 429–440. [Google Scholar] [CrossRef]
- European Food Safety Authority (EFSA). Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J. 2013, 11, 1–103. [Google Scholar] [CrossRef] [Green Version]
- Lennox, A.; Sommerville, J.; Ong, K.; Henderson, H.; Allen, R. Diet and Nutrition Survey of Infants and Young Children, 2011; Department of Health and Food Standards Agency: London, UK, 2013.
- Patro-Gołąb, B.; Zalewski, B.M.; Kołodziej, M.; Kouwenhoven, S.; Poston, L.; Godfrey, K.M.; Koletzko, B.; Van Goudoever, J.B.; Szajewska, H. Nutritional interventions or exposures in infants and children aged up to 3 years and their effects on subsequent risk of overweight, obesity and body fat: A systematic review of systematic reviews. Obes. Rev. 2016, 17, 1245–1257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mennella, J.A. Ontogeny of taste preferences: Basic biology and implications for health. Am. J. Clin. Nutr. 2014, 99, 704–711. [Google Scholar] [CrossRef] [Green Version]
- Burdette, H.L.; Whitaker, R.C.; Hall, W.C.; Daniels, S.R. Maternal infant-feeding style and children′s adiposity at 5 years of age. Arch. Pediatr. Adolesc. Med. 2006, 160, 513–520. [Google Scholar] [CrossRef] [Green Version]
- Brown, A.; Lee, M. Maternal child-feeding style during the weaning period: Association with infant weight and maternal eating style. Eat. Behav. 2011, 12, 108–111. [Google Scholar] [CrossRef] [Green Version]
- Gross, R.S.; Mendelsohn, A.L.; Fierman, A.H.; Messito, M.J. Maternal controlling feeding styles during early infancy. Clin. Pediatr. 2011, 50, 1125–1133. [Google Scholar] [CrossRef]
- Holub, S.C.; Dolan, E.A. Mothers′ beliefs about infant size: Associations with attitudes and infant feeding practices. J. Appl. Dev. Psychol. 2012, 33, 158–164. [Google Scholar] [CrossRef]
- De Souza Rezende, P.; de Moraes, D.E.B.; Mais, L.A.; Warkentin, S.; Taddei, J.A.D.A.C. Maternal pressure to eat: Associations with maternal and child characteristics among 2-to 8-year-olds in Brazil. Appetite 2019, 133, 40–46. [Google Scholar] [CrossRef]
- Farrow, C.; Blissett, J. Does maternal control during feeding moderate early infant weight gain? Pediatrics 2006, 118, e293–e298. [Google Scholar] [CrossRef] [Green Version]
- Galloway, A.T.; Fiorito, L.M.; Francis, L.A.; Birch, L.L. “Finish your soup”: Counterproductive effects of pressuring children to eat on intake and affect. Appetite 2006, 46, 318–323. [Google Scholar] [CrossRef] [Green Version]
- Fildes, A.; van Jaarsveld, C.H.M.; Llewellyn, C.; Wardle, J.; Fisher, A. Parental control over feeding in infancy. Influence of infant weight, appetite and feeding method. Appetite 2015, 91, 101–106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ministerio de Sanidad de España: Porcentaje de Personas con Obesidad, por Sexo Según Comunidad Autónoma. Available online: https://www.mscbs.gob.es/estadEstudios/sanidadDatos/tablas/tabla10.htm (accessed on 20 December 2020).
- McPhie, S.; Skouteris, H.; Fuller-Tyszkiewicz, M.; McCabe, M.; Ricciardelli, L.A.; Milgrom, J.; Baur, L.A.; Dell’Aquila, D. Maternal predictors of preschool child-eating behaviours, food intake and body mass index: A prospective study. Early Child Dev. Care 2012, 182, 999–1014. [Google Scholar] [CrossRef]
- Blissett, J.; Meyer, C.; Haycraft, E. Maternal and paternal controlling feeding practices with male and female children. Appetite 2006, 47, 212–219. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, H.; Keller, K.L. Children who are pressured to eat at home consume fewer high-fat foods in laboratory test meals. J. Acad. Nutr. Diet. 2012, 112, 271–275. [Google Scholar] [CrossRef] [Green Version]
- Webber, L.; Cooke, L.; Hill, C.; Wardle, J. Child adiposity and maternal feeding practices: A longitudinal analysis. Am. J. Clin. Nutr. 2010, 92, 1423–1428. [Google Scholar] [CrossRef]
- Brown, A.; Lee, M. Breastfeeding is associated with a maternal feeding style low in control from birth. PLoS ONE 2013, 8, 1–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Synnott, K.; Bogue, J.; Edwards, C.A.; Scott, J.A.; Higgins, S.; Norin, E.; Frias, D.; Amarri, S.; Adam, R. Parental perceptions of feeding practices in five European countries: An exploratory study. Eur. J. Clin. Nutr. 2007, 61, 946–956. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Duke, R.E.; Bryson, S.; Hammer, L.D.; Agras, W.S. The relationship between parental factors at infancy and parent-reported control over children’s eating at age 7. Appetite 2004, 43, 247–252. [Google Scholar] [CrossRef] [PubMed]
- Li, R.; Scanlon, K.S.; May, A.; Rose, C.; Birch, L. Bottle-feeding practices during early infancy and eating behaviors at 6 years of age. Pediatrics 2014, 134, S70–S77. [Google Scholar] [CrossRef] [Green Version]
- Timby, N.; Hernell, O.; Lönnerdal, B.; Domellöf, M. Parental feeding control in relation to feeding mode and growth pattern during early infancy. Acta Paediatr. 2014, 103, 1072–1077. [Google Scholar] [CrossRef] [PubMed]
- Warkentin, S.; Mais, L.A.; De Oliveira, M.D.R.D.; Carnell, S.; de Aguiar CarrazedoTaddei, J.A. Relationships between parent feeding behaviors and parent and child characteristics in Brazilian preschoolers: A cross-sectional study. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Dinkevich, E.; Leid, L.; Pryor, K.; Wei, Y.; Huberman, H.; Carnell, S. Mothers’ feeding behaviors in infancy: Do they predict child weight trajectories? Obesity 2015, 23, 2470–2476. [Google Scholar] [CrossRef] [Green Version]
- Gonçalves, S.; Lima, V.; Machado, B.C.; Machado, P. Maternal–child feeding practices and associations with maternal and child characteristics. Nutr. Today 2017, 52, 232–239. [Google Scholar] [CrossRef]
- Gross, R.S.; Fierman, A.H.; Mendelsohn, A.L.; Chiasson, M.A.; Rosenberg, T.J.; Scheinmann, R.; Messito, M.J. Maternal perceptions of infant hunger, satiety, and pressuring feeding styles in an urban Latina WIC population. Acad. Pediatr. 2010, 10, 29–35. [Google Scholar] [CrossRef]
- Loth, K.A.; MacLehose, R.F.; Fulkerson, J.A.; Crow, S.; Neumark-Sztainer, D. Eat this, not that! Parental demographic correlates of food-related parenting practices. Appetite 2013, 60, 140–147. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Real, H.; Oliveira, A.; Severo, M.; Moreira, P.; Lopes, C. Combination and adaptation of two tools to assess parental feeding practices in pre-school children. Eat. Behav. 2014, 15, 383–387. [Google Scholar] [CrossRef]
- Russell, C.G.; Haszard, J.J.; Taylor, R.W.; Heath, A.L.M.; Taylor, B.; Campbell, K.J. Parental feeding practices associated with children’s eating and weight: What are parents of toddlers and preschool children doing? Appetite 2018, 128, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Hughes, S.O.; Frankel, L.A.; Beltran, A.; Hodges, E.; Hoerr, S.; Lumeng, J.; Tovar, A.; Kremers, S. Food parenting measurement issues: Working group consensus report. Child. Obes. 2013, 9, S95–S102. [Google Scholar] [CrossRef] [Green Version]
- Stifter, C.A.; Moding, K.J. Understanding and measuring parent use of food to soothe infant and toddler distress: A longitudinal study from 6 to 18 months of age. Appetite 2015, 95, 188–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| n or Mean ± SD | Percentage (%) | |
|---|---|---|
| Characteristics of infants and toddlers | ||
| Age (months) | 11.8 ± 3.6 | |
| 3–6 months | 56 | 8.9 |
| 7–11 months | 230 | 36.5 |
| 12–18 months | 344 | 54.6 |
| Gender | ||
| Boy | 323 | 51.3 |
| Girl | 307 | 48.7 |
| Birth weight (g) | 3222 ± 493 | |
| Position between brothers/sisters | ||
| First | 39 | 6.2 |
| Second | 207 | 32.9 |
| Third | 32 | 5.1 |
| Fourth | 5 | 0.8 |
| No brothers and/or sisters | 347 | 55.1 |
| Daycare attendance | ||
| Yes | 245 | 38.9 |
| No | 385 | 61.1 |
| More than three days a week lunch at daycare | ||
| Yes | 172 | 27.3 |
| No | 73 | 11.6 |
| Characteristics of parents | ||
| Age (years) | 34.6 ± 4.2 | |
| Gender | ||
| Female | 501 | 79.5 |
| Male | 129 | 20.5 |
| Region | ||
| North-East | 121 | 19.2 |
| East | 90 | 14.3 |
| South | 124 | 19.7 |
| Center | 168 | 26.7 |
| North-West | 63 | 10.0 |
| North | 55 | 8.7 |
| Canary Islands | 9 | 1.4 |
| City size | ||
| Medium/big city | 398 | 63.2 |
| Small city/village/countryside | 232 | 36.8 |
| Education | ||
| Primary school | 15 | 2.4 |
| Secondary school | 146 | 23.2 |
| University bachelor/master/PhD | 469 | 74.4 |
| Job intensity | ||
| Full-time | 378 | 60.0 |
| Part-time/per hours | 107 | 17.0 |
| Unknown/not working | 145 | 23.0 |
| Total monthly income (€) | ||
| <1000 | 43 | 6.9 |
| >1000 | 491 | 77.9 |
| Do not know/no answer | 96 | 15.2 |
| Marital status | ||
| Divorced/single | 35 | 5.6 |
| Married/living with a partner | 595 | 94.4 |
| Food Categories Per Age | n | Every Day | 5–6 Days | 3–4 Days | 1–2 Days | Rarely |
|---|---|---|---|---|---|---|
| Cereals | 577 | |||||
| 3–6 months | 51 | 14 (27%) | 9 (18%) | 6 (12%) | 2 (4%) | 20 (39%) |
| 7–11 months | 206 | 94 (46%) | 21 (10%) | 16 (8%) | 12 (6%) | 63 (30%) |
| 12–18 months | 320 | 157 (49%) | 33 (10%) | 22 (7%) | 16 (5%) | 92 (29%) |
| Fruits | 574 | |||||
| 3–6 months | 36 | 25 (69%) | 9 (25%) | 2 (6%) | 0 (0%) | 0 (0%) |
| 7–11 months | 211 | 167 (79%) | 30 (14%) | 10 (5%) | 4 (2%) | 0 (0%) |
| 12–18 months | 327 | 246 (75%) | 65 (20%) | 13 (4%) | 3 (1%) | 0 (0%) |
| Vegetables | 545 | |||||
| 3–6 months | 25 | 16 (64%) | 7 (28%) | 2 (8%) | 0 (0%) | 0 (0%) |
| 7–11 months | 199 | 150 (75%) | 31 (16%) | 13 (7%) | 5 (2%) | 0 (0%) |
| 12–18 months | 321 | 216 (67%) | 68 (21%) | 25 (8%) | 10 (3%) | 2 (1%) |
| Yogurt | 468 | |||||
| 3–6 months | 15 | 4 (27%) | 6 (40%) | 2 (13%) | 3 (20%) | 0 (0%) |
| 7–11 months | 159 | 68 (43%) | 46 (29%) | 27 (17%) | 12 (7%) | 6 (4%) |
| 12–18 months | 294 | 174 (59%) | 62 (21%) | 40 (14%) | 13 (4%) | 5 (2%) |
| Meat | 490 | |||||
| 3–6 months | 13 | 4 (31%) | 4 (31%) | 4 (31%) | 1 (8%) | 0 (0%) |
| 7–11 months | 179 | 50 (28%) | 43 (24%) | 64 (36%) | 19 (10%) | 3 (2%) |
| 12–18 months | 298 | 46 (15%) | 82 (28%) | 133 (45%) | 36 (12%) | 1 (0%) |
| Cheese | 252 | |||||
| 3–6 months | 3 | 0 (0%) | 1 (33%) | 1 (33%) | 0 (0%) | 1 (33%) |
| 7–11 months | 35 | 1 (3%) | 4 (11%) | 10 (29%) | 13 (37%) | 7 (20%) |
| 12–18 months | 214 | 14 (6%) | 41 (19%) | 53 (25%) | 70 (33%) | 36 (17%) |
| Fish | 422 | |||||
| 3–6 months | 5 | 0 (0%) | 2 (40%) | 3 (60%) | 0 (0%) | 0 (0%) |
| 7–11 months | 121 | 6 (5%) | 19 (16%) | 53 (44%) | 37 (31%) | 6 (5%) |
| 12–18 months | 296 | 15 (5%) | 58 (20%) | 134 (45%) | 85 (29%) | 4 (1%) |
| Eggs | 323 | |||||
| 3–6 months | 4 | 0 (0%) | 1 (25%) | 1 (25%) | 1 (25%) | 1 (25%) |
| 7–11 months | 61 | 0 (0%) | 2 (3%) | 6 (10%) | 39 (64%) | 14 (23%) |
| 12–18 months | 258 | 1 (0%) | 6 (2%) | 33 (13%) | 183 (71%) | 35 (14%) |
| Legumes | 300 | |||||
| 3–6 months | 4 | 0 (0%) | 0 (0%) | 1 (25%) | 1 (25%) | 2 (50%) |
| 7–11 months | 51 | 1 (2%) | 6 (12%) | 10 (20%) | 27 (53%) | 7 (14%) |
| 12–18 months | 245 | 1 (1%) | 15 (6%) | 56 (23%) | 138 (56%) | 35 (14%) |
| Age Group | Home-Prepared Food, n (%) | Never Home-Prepared Food, n (%) |
|---|---|---|
| 3–6 months | 43 (77%) | 13 (23%) |
| 7–11 months | 216 (94%) | 14 (6%) |
| 12–18 months | 327 (95%) | 17 (5%) |
| Total | 586 (93%) | 44 (7%) |
| Pressure to Eat Scale and Its Items 1 | Mean ± SD |
|---|---|
| My child should always eat all of the food | 3.45 ± 1.13 |
| I try my best to make sure my child eats enough | 4.01 ± 0.88 |
| My child would eat much less if I do not pay attention to the feeding | 2.93 ± 1.20 |
| Variable | Characteristics | Mean ± SD | F-Value | p-Value | |
|---|---|---|---|---|---|
| Pressure to eat | Gender infant | Girl | 3.54 ± 0.84 | F1,628 = 5.67 | 0.02 |
| Boy | 3.39 ± 0.81 | ||||
| Parent’s age | ≤30 years | 3.61 ± 0.78 | F1,628 = 3.68 | 0.05 | |
| >30 years | 3.44 ± 0.83 | ||||
| Job intensity | Full-time | 3.50 ± 0.79 | F1,483 = 8.55 | <0.01 | |
| Part-time/per hours | 3.25 ± 0.76 | ||||
| Region | North | 3.20 ± 0.81 | F6,623 = 2.81 | 0.01 | |
| North-East | 3.47 ± 0.78 | ||||
| East | 3.56 ± 0.81 | ||||
| South | 3.57 ± 0.82 | ||||
| Center | 3.51 ± 0.77 | ||||
| North-West | 3.26 ± 0.95 | ||||
| Canary Islands | 2.96 ± 1.20 |
| Variable | Food Category | Child Does Not Eat This Food Mean ± SD | Child Eats This Food Mean ± SD | F-Value | p-Value |
|---|---|---|---|---|---|
| Pressure to eat | Fruit | 3.88 ± 0.69 | 3.44 ± 0.83 | F1,578 = 4.22 | 0.04 |
| Vegetables | 3.74 ± 0.72 | 3.43 ± 0.84 | F1,578 = 4.78 | 0.03 | |
| Meat | 3.64 ± 0.80 | 3.42 ± 0.83 | F1,578 = 5.37 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Klerks, M.; Roman, S.; Bernal, M.J.; Haro-Vicente, J.F.; Sanchez-Siles, L.M. Complementary Feeding Practices and Parental Pressure to Eat among Spanish Infants and Toddlers: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 1982. https://doi.org/10.3390/ijerph18041982
Klerks M, Roman S, Bernal MJ, Haro-Vicente JF, Sanchez-Siles LM. Complementary Feeding Practices and Parental Pressure to Eat among Spanish Infants and Toddlers: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2021; 18(4):1982. https://doi.org/10.3390/ijerph18041982
Chicago/Turabian StyleKlerks, Michelle, Sergio Roman, Maria Jose Bernal, Juan Francisco Haro-Vicente, and Luis Manuel Sanchez-Siles. 2021. "Complementary Feeding Practices and Parental Pressure to Eat among Spanish Infants and Toddlers: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 18, no. 4: 1982. https://doi.org/10.3390/ijerph18041982