Challenges and Perspectives for Biosensing of Bioaerosol Containing Pathogenic Microorganisms
Abstract
:1. Introduction
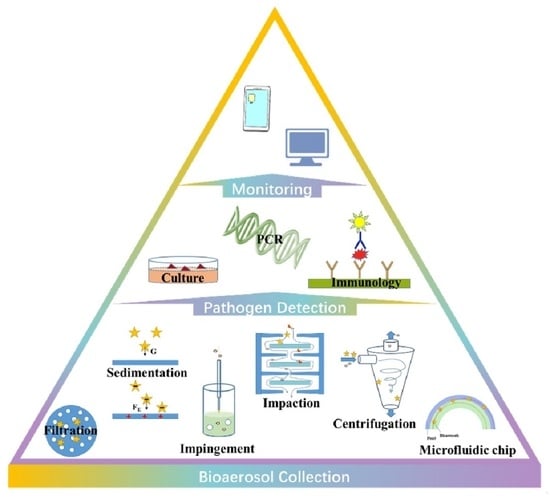
2. Bioaerosol Collection
2.1. Sedimentation
2.2. Filtration
2.3. Centrifugation
2.4. Impaction
2.5. Impingement
2.6. Microfluidics
3. Pathogen Detection
3.1. Microbial Culture
3.2. Molecular Biological Detection
3.3. Immunological Detection
3.4. Others
4. Conclusions and Future Trends
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Kabir, E.; Azzouz, A.; Raza, N.; Bhardwaj, S.K.; Kim, K.-H.; Tabatabaei, M.; Kukkar, D. Recent Advances in Monitoring, Sampling, and Sensing Techniques for Bioaerosols in the Atmosphere. ACS Sens. 2020, 5, 1254–1267. [Google Scholar] [CrossRef] [PubMed]
- Haig, C.; Mackay, W.; Walker, J.; Williams, C. Bioaerosol sampling: Sampling mechanisms, bioefficiency and field studies. J. Hosp. Infect. 2016, 93, 242–255. [Google Scholar] [CrossRef]
- Pan, M.; Lednicky, J.; Wu, C. Collection, particle sizing and detection of airborne viruses. J. Appl. Microbiol. 2019, 127, 1596–1611. [Google Scholar] [CrossRef] [Green Version]
- Ghosh, B.; Lal, H.; Srivastava, A. Review of bioaerosols in indoor environment with special reference to sampling, analysis and control mechanisms. Environ. Int. 2015, 85, 254–272. [Google Scholar] [CrossRef]
- Xie, W.; Li, Y.; Bai, W.; Hou, J.; Ma, T.; Zeng, X.; Zhang, L.; An, T. The source and transport of bioaerosols in the air: A review. Front. Environ. Sci. Eng. 2021, 15, 1–19. [Google Scholar] [CrossRef]
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed on 9 December 2020).
- Tong, T.R. Airborne Severe Acute Respiratory Syndrome Coronavirus and Its Implications. J. Infect. Dis. 2005, 191, 1401–1402. [Google Scholar] [CrossRef] [Green Version]
- Booth, T.F.; Kournikakis, B.; Bastien, N.; Ho, J.; Kobasa, D.; Stadnyk, L.; Li, Y.; Spence, M.; Paton, S.; Henry, B.; et al. Detection of Airborne Severe Acute Respiratory Syndrome (SARS) Coronavirus and Environmental Contamination in SARS Outbreak Units. J. Infect. Dis. 2005, 191, 1472–1477. [Google Scholar] [CrossRef]
- Kim, H.R.; An, S.; Hwang, J. High air flow-rate electrostatic sampler for the rapid monitoring of airborne coronavirus and influenza viruses. J. Hazard. Mater. 2021, 412, 125219. [Google Scholar] [CrossRef] [PubMed]
- Piri, A.; Kim, H.R.; Park, D.H.; Hwang, J. Increased survivability of coronavirus and H1N1 influenza virus under electrostatic aerosol-to-hydrosol sampling. J. Hazard. Mater. 2021, 413, 125417. [Google Scholar] [CrossRef]
- Da Silva, P.G.; Nascimento, M.S.J.; Soares, R.R.G.; Sousa, S.I.V.; Mesquita, J.R. Airborne spread of infectious SARS-CoV-2: Moving forward using lessons from SARS-CoV and MERS-CoV. Sci. Total Environ. 2021, 764, 142802. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.C.; Mui, K.; Wong, L.; Chu, H. Ventilation of general hospital wards for mitigating infection risks of three kinds of viruses including Middle East respiratory syndrome coronavirus. Indoor Built Environ. 2016, 26, 514–527. [Google Scholar] [CrossRef]
- Kim, S.-H.; Chang, S.Y.; Sung-Han, K.; Park, J.H.; BIN Kim, H.; Lee, H.; Choi, J.-P.; Choi, W.S.; Min, J.-Y. Extensive Viable Middle East Respiratory Syndrome (MERS) Coronavirus Contamination in Air and Surrounding Environment in MERS Isolation Wards. Clin. Infect. Dis. 2016, 63, 363–369. [Google Scholar] [CrossRef] [Green Version]
- Lane, M.A.; Brownsword, E.A.; Morgan, J.S.; Babiker, A.; Vanairsdale, S.A.; Lyon, G.M.; Mehta, A.K.; Ingersoll, J.M.; Lindsley, W.G.; Kraft, C.S. Bioaerosol sampling of a ventilated patient with COVID-19. Am. J. Infect. Control. 2020, 48, 1540–1542. [Google Scholar] [CrossRef]
- Gholipour, S.; Mohammadi, F.; Nikaeen, M.; Shamsizadeh, Z.; Khazeni, A.; Sahbaei, Z.; Mousavi, S.M.; Ghobadian, M.; Mirhendi, H. COVID-19 infection risk from exposure to aerosols of wastewater treatment plants. Chemosphere 2021, 273, 129701. [Google Scholar] [CrossRef] [PubMed]
- Robotto, A.; Quaglino, P.; Lembo, D.; Morello, M.; Brizio, E.; Bardi, L.; Civra, A. SARS-CoV-2 and indoor/outdoor air samples: A methodological approach to have consistent and comparable results. Environ. Res. 2021, 195, 110847. [Google Scholar] [CrossRef] [PubMed]
- Mainelis, G. Bioaerosol sampling: Classical approaches, advances, and perspectives. Aerosol Sci. Technol. 2019, 54, 496–519. [Google Scholar] [CrossRef]
- Franchitti, E.; Pascale, E.; Fea, E.; Anedda, E.; Traversi, D. Methods for Bioaerosol Characterization: Limits and Perspectives for Human Health Risk Assessment in Organic Waste Treatment. Atmosphere 2020, 11, 452. [Google Scholar] [CrossRef]
- Fung, A.O.; Mykhaylova, N. Analysis of Airborne Biomarkers for Point-of-Care Diagnostics. J. Lab. Autom. 2013, 19, 225–247. [Google Scholar] [CrossRef]
- Mbareche, H.; Brisebois, E.; Veillette, M.; Duchaine, C. Bioaerosol sampling and detection methods based on molecular approaches: No pain no gain. Sci. Total. Environ. 2017, 599–600, 2095–2104. [Google Scholar] [CrossRef]
- Huffman, J.A.; Perring, A.E.; Savage, N.J.; Clot, B.; Crouzy, B.; Tummon, F.; Shoshanim, O.; Damit, B.; Schneider, J.; Sivaprakasam, V.; et al. Real-time sensing of bioaerosols: Review and current perspectives. Aerosol Sci. Technol. 2020, 54, 465–495. [Google Scholar] [CrossRef] [Green Version]
- Jing, W.; Zhao, W.; Liu, S.; Li, L.; Tsai, C.-T.; Fan, X.; Wu, W.; Li, J.; Yang, X.; Sui, G. Microfluidic Device for Efficient Airborne Bacteria Capture and Enrichment. Anal. Chem. 2013, 85, 5255–5262. [Google Scholar] [CrossRef] [PubMed]
- Han, T.T.; Thomas, N.M.; Mainelis, G. Performance of personal electrostatic bioaerosol sampler (PEBS) when collecting airborne microorganisms. J. Aerosol Sci. 2018, 124, 54–67. [Google Scholar] [CrossRef]
- Foat, T.; Sellors, W.; Walker, M.; Rachwal, P.; Jones, J.; Despeyroux, D.; Coudron, L.; Munro, I.; McCluskey, D.; Tan, C.; et al. A prototype personal aerosol sampler based on electrostatic precipitation and electrowetting-on-dielectric actuation of droplets. J. Aerosol Sci. 2016, 95, 43–53. [Google Scholar] [CrossRef] [Green Version]
- Ladhani, L.; Pardon, G.; Meeuws, H.; Van Wesenbeeck, L.; Schmidt, K.; Stuyver, L.; Van Der Wijngaart, W. Sampling and detection of airborne influenza virus towards point-of-care applications. PLoS ONE 2017, 12, e0174314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, H.R.; Park, J.-W.; Kim, H.S.; Yong, D.; Hwang, J. Comparison of lab-made electrostatic rod-type sampler with single stage viable impactor for identification of indoor airborne bacteria. J. Aerosol Sci. 2018, 115, 190–197. [Google Scholar] [CrossRef]
- Park, M.; Son, A.; Chua, B. Microorganism-ionizing respirator with reduced breathing resistance suitable for removing airborne bacteria. Sens. Actuators B Chem. 2018, 276, 437–446. [Google Scholar] [CrossRef] [PubMed]
- Hyun, J.; Lee, S.-G.; Hwang, J. Application of corona discharge-generated air ions for filtration of aerosolized virus and inactivation of filtered virus. J. Aerosol Sci. 2017, 107, 31–40. [Google Scholar] [CrossRef]
- La, A.; Zhang, Q.; Levin, D.B.; Coombs, K.M. The Effectiveness of Air Ionization in Reducing Bioaerosols and Airborne PRRS Virus in a Ventilated Space. Trans. ASABE 2019, 62, 1299–1314. [Google Scholar] [CrossRef]
- Park, K.T.; Cho, D.G.; Park, J.W.; Hong, S.; Hwang, J. Detection of airborne viruses using electro-aerodynamic deposition and a field-effect transistor. Sci. Rep. 2015, 5, 17462. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roux, J.M.; Sarda-Estève, R.; Delapierre, G.; Nadal, M.H.; Bossuet, C.; Olmedo, L. Development of a new portable air sampler based on electrostatic precipitation. Environ. Sci. Pollut. Res. 2016, 23, 8175–8183. [Google Scholar] [CrossRef] [PubMed]
- Afshar-Mohajer, N.; Godfrey, W.H.; Rule, A.M.; Matsui, E.C.; Gordon, J.; Koehler, K. A Low-Cost Device for Bulk Sampling of Airborne Particulate Matter: Evaluation of an Ionic Charging Device. Aerosol Air Qual. Res. 2017, 17, 1452–1462. [Google Scholar] [CrossRef] [Green Version]
- Hong, S.; Bhardwaj, J.; Han, C.-H.; Jang, J. Gentle Sampling of Submicrometer Airborne Virus Particles using a Personal Electrostatic Particle Concentrator. Environ. Sci. Technol. 2016, 50, 12365–12372. [Google Scholar] [CrossRef]
- Park, J.-W.; Kim, H.R.; Hwang, J. Continuous and real-time bioaerosol monitoring by combined aerosol-to-hydrosol sampling and ATP bioluminescence assay. Anal. Chim. Acta 2016, 941, 101–107. [Google Scholar] [CrossRef]
- Priyamvada, H.; Kumaragama, K.; Chrzan, A.; Athukorala, C.; Sur, S.; Dhaniyala, S. Design and evaluation of a new electrostatic precipitation-based portable low-cost sampler for bioaerosol monitoring. Aerosol Sci. Technol. 2021, 55, 24–36. [Google Scholar] [CrossRef]
- Maestre, J.P.; Jennings, W.; Wylie, D.; Horner, S.D.; Siegel, J.; Kinney, K.A. Filter forensics: Microbiota recovery from residential HVAC filters. Microbiome 2018, 6, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Therkorn, J.; Thomas, N.; Scheinbeim, J.; Mainelis, G. Field performance of a novel passive bioaerosol sampler using polarized ferroelectric polymer films. Aerosol Sci. Technol. 2017, 51, 787–800. [Google Scholar] [CrossRef] [Green Version]
- Hurley, K.V.; Wharton, L.; Wheeler, M.J.; Skjøth, C.A.; Niles, C.; Hanson, M.C. Car cabin filters as sampling devices to study bioaerosols using eDNA and microbiological methods. Aerobiologia 2019, 35, 215–225. [Google Scholar] [CrossRef]
- Li, J.; Leavey, A.; Wang, Y.; ÓNeil, C.; Wallace, M.A.; Burnham, C.-A.D.; Boon, A.C.; Babcock, H.; Biswas, P. Comparing the performance of 3 bioaerosol samplers for influenza virus. J. Aerosol Sci. 2018, 115, 133–145. [Google Scholar] [CrossRef]
- Choi, D.Y.; Heo, K.J.; Kang, J.; An, E.J.; Jung, S.-H.; Lee, B.U.; Lee, H.M.; Jung, J.H. Washable antimicrobial polyester/aluminum air filter with a high capture efficiency and low pressure drop. J. Hazard. Mater. 2018, 351, 29–37. [Google Scholar] [CrossRef] [PubMed]
- Grayson, S.A.; Griffiths, P.S.; Perez, M.K.; Piedimonte, G. Detection of airborne respiratory syncytial virus in a pediatric acute care clinic. Pediatr. Pulmonol. 2017, 52, 684–688. [Google Scholar] [CrossRef] [PubMed]
- Kenny, L.C.; Thorpe, A.; Stacey, P. A collection of experimental data for aerosol monitoring cyclones. Aerosol Sci. Technol. 2017, 51, 1190–1200. [Google Scholar] [CrossRef] [Green Version]
- Prost, K.; Kloeze, H.; Mukhi, S.; Bozek, K.; Poljak, Z.; Mubareka, S. Bioaerosol and surface sampling for the surveillance of influenza A virus in swine. Transbound. Emerg. Dis. 2019, 66, 1210–1217. [Google Scholar] [CrossRef] [PubMed]
- Bekking, C.; Yip, L.; Groulx, N.; Doggett, N.; Finn, M.; Mubareka, S. Evaluation of bioaerosol samplers for the detection and quantification of influenza virus from artificial aerosols and influenza virus–infected ferrets. Influ. Other Respir. Viruses 2019, 13, 564–573. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sung, G.; Ahn, C.; Kulkarni, A.; Shin, W.G.; Kim, T. Highly efficient in-line wet cyclone air sampler for airborne virus detection. J. Mech. Sci. Technol. 2017, 31, 4363–4369. [Google Scholar] [CrossRef]
- Cho, Y.S.; Hong, S.C.; Choi, J.; Jung, J.H. Development of an automated wet-cyclone system for rapid, continuous and enriched bioaerosol sampling and its application to real-time detection. Sens. Actuators B Chem. 2019, 284, 525–533. [Google Scholar] [CrossRef]
- Cho, Y.S.; Kim, H.R.; Ko, H.S.; Bin Jeong, S.; Kim, B.C.; Jung, J.H. Continuous Surveillance of Bioaerosols On-Site Using an Automated Bioaerosol-Monitoring System. ACS Sens. 2020, 5, 395–403. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-W.; Ting, Y.-T.; Horng, Y.-J. Collection efficiency of liquid-based samplers for fungi in indoor air. Indoor Air 2019, 29, 380–389. [Google Scholar] [CrossRef]
- Alonso, C.; Raynor, P.C.; Davies, P.R.; Torremorell, M. Concentration, Size Distribution, and Infectivity of Airborne Particles Carrying Swine Viruses. PLoS ONE 2015, 10, e0135675. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Kang, J.S.; Hong, S.C.; Bae, G.-N.; Jung, J.H. A new method for the real-time quantification of airborne biological particles using a coupled inertial aerosol system with in situ fluorescence imaging. Sens. Actuators B Chem. 2017, 244, 635–641. [Google Scholar] [CrossRef]
- Wu, Y.; Calis, A.; Luo, Y.; Chen, C.; Lutton, M.; Rivenson, Y.; Lin, X.; Koydemir, H.C.; Zhang, Y.; Wang, H.; et al. Label-Free Bioaerosol Sensing Using Mobile Microscopy and Deep Learning. ACS Photonics 2018, 5, 4617–4627. [Google Scholar] [CrossRef]
- Lindsley, W.G.; Blachere, F.M.; Beezhold, D.; Thewlis, R.E.; Noorbakhsh, B.; Othumpangat, S.; Goldsmith, W.T.; McMillen, C.M.; Andrew, M.E.; Burrell, C.N.; et al. Viable influenza A virus in airborne particles expelled during coughs versus exhalations. Influ. Other Respir. Viruses 2016, 10, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Cooper, C.W.; Aithinne, K.; Floyd, E.L.; Stevenson, B.S.; Johnson, D.L. A comparison of air sampling methods for Clostridium difficile endospore aerosol. Aerobiologia 2019, 35, 411–420. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, R.M.W.; Garcia-Alcega, S.; Coulon, F.; Dumbrell, A.J.; Whitby, C.; Colbeck, I. Bioaerosol biomonitoring: Sampling optimization for molecular microbial ecology. Mol. Ecol. Resour. 2019, 19, 672–690. [Google Scholar] [CrossRef]
- Nguyen, D.T.; Kim, H.R.; Jung, J.H.; Lee, K.-B.; Kim, B.C. The development of paper discs immobilized with luciferase/D-luciferin for the detection of ATP from airborne bacteria. Sens. Actuators B Chem. 2018, 260, 274–281. [Google Scholar] [CrossRef]
- Šantl-Temkiv, T.; Amato, P.; Gosewinkel, U.; Thyrhaug, R.; Charton, A.; Chicot, B.; Finster, K.; Bratbak, G.; Löndahl, J. High-Flow-Rate Impinger for the Study of Concentration, Viability, Metabolic Activity, and Ice-Nucleation Activity of Airborne Bacteria. Environ. Sci. Technol. 2017, 51, 11224–11234. [Google Scholar] [CrossRef]
- Zheng, Y.; Yao, M. Liquid impinger BioSampler’s performance for size-resolved viable bioaerosol particles. J. Aerosol Sci. 2017, 106, 34–42. [Google Scholar] [CrossRef]
- Pardon, G.; Ladhani, L.; Sandström, N.; Ettori, M.; Lobov, G.; van der Wijngaart, W. Aerosol sampling using an electrostatic precipitator integrated with a microfluidic interface. Sens. Actuators B Chem. 2015, 212, 344–352. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Han, Y.; Gao, Y.; Gao, J.; Ji, H.; He, Q.; Tu, J.; Xu, G.; Zhang, Y.; Han, L. Electrochemical sensor array with nanoporous gold nanolayer and ceria@gold corona-nanocomposites enhancer integrated into microfluidic for simultaneous ultrasensitive lead ion detection. Electrochim. Acta 2021, 373, 137921. [Google Scholar] [CrossRef]
- Zhang, X.; Chen, X.; Yao, Y.; Shang, X.; Lu, H.; Zhao, W.; Liu, S.; Chen, J.; Sui, G. A disc-chip based high-throughput acute toxicity detection system. Talanta 2021, 224, 121867. [Google Scholar] [CrossRef]
- Qi, W.; Zheng, L.; Wang, S.; Huang, F.; Liu, Y.; Jiang, H.; Lin, J. A microfluidic biosensor for rapid and automatic detection of Salmonella using metal-organic framework and Raspberry Pi. Biosens. Bioelectron. 2021, 178, 113020. [Google Scholar] [CrossRef] [PubMed]
- Chen, P.; Chen, C.; Su, H.; Zhou, M.; Li, S.; Du, W.; Feng, X.; Liu, B.-F. Integrated and finger-actuated microfluidic chip for point-of-care testing of multiple pathogens. Talanta 2021, 224, 121844. [Google Scholar] [CrossRef]
- Tsougeniab, K.; Kaprouac, G.; Loukas, C.; Papadakis, G.; Hamiot, A.; Eck, M.; Rabus, D.; Kokkoris, G.; Chatzandroulis, S.; Papadopoulos, V.; et al. Lab-on-Chip platform and protocol for rapid foodborne pathogen detection comprising on-chip cell capture, lysis, DNA amplification and surface-acoustic-wave detection. Sens. Actuators B Chem. 2020, 320, 128345. [Google Scholar] [CrossRef]
- Liu, Y.; Tan, Y.; Fu, Q.; Lin, M.; He, J.; He, S.; Yang, M.; Chen, S.; Zhou, J. Reciprocating-flowing on-a-chip enables ultra-fast immunobinding for multiplexed rapid ELISA detection of SARS-CoV-2 antibody. Biosens. Bioelectron. 2021, 176, 112920. [Google Scholar] [CrossRef] [PubMed]
- Hosokawa, K. Biomarker Analysis on a Power-free Microfluidic Chip Driven by Degassed Poly(dimethylsiloxane). Anal. Sci. 2021, 37, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Tsagkaris, A.S.; Migliorelli, D.; Uttl, L.; Filippini, D.; Pulkrabova, J.; Hajslova, J. A microfluidic paper-based analytical device (muPAD) with smartphone readout for chlorpyrifos-oxon screening in human serum. Talanta 2021, 222, 121535. [Google Scholar] [CrossRef]
- Li, X.; Zhang, X.; Liu, Q.; Zhao, W.; Liu, S.; Sui, G. Microfluidic System for Rapid Detection of Airborne Pathogenic Fungal Spores. ACS Sens. 2018, 3, 2095–2103. [Google Scholar] [CrossRef]
- Hong, S.C.; Kang, J.S.; Lee, J.E.; Kim, S.S.; Jung, J.H. Continuous aerosol size separator using inertial microfluidics and its application to airborne bacteria and viruses. Lab Chip 2015, 15, 1889–1897. [Google Scholar] [CrossRef]
- Ma, Z.; Zheng, Y.; Cheng, Y.; Xie, S.; Ye, X.; Yao, M. Development of an integrated microfluidic electrostatic sampler for bioaerosol. J. Aerosol Sci. 2016, 95, 84–94. [Google Scholar] [CrossRef]
- Jing, W.; Jiang, X.; Zhao, W.; Liu, S.; Cheng, X.; Sui, G. Microfluidic Platform for Direct Capture and Analysis of Airborne Mycobacterium tuberculosis. Anal. Chem. 2014, 86, 5815–5821. [Google Scholar] [CrossRef]
- Choi, J.; Hong, S.C.; Kim, W.; Jung, J.H. Highly Enriched, Controllable, Continuous Aerosol Sampling Using Inertial Microfluidics and Its Application to Real-Time Detection of Airborne Bacteria. ACS Sens. 2017, 2, 513–521. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, X.; Yao, Y.; Jing, W.; Liu, S.; Sui, G. A novel microfluidic module for rapid detection of airborne and waterborne pathogens. Sens. Actuators B Chem. 2018, 258, 1138–1145. [Google Scholar] [CrossRef]
- Nasrabadi, A.M.; Park, J.-W.; Kim, H.S.; Han, J.S.; Hyun, J.; Yong, D.; Hwang, J. Assessment of indoor bioaerosols using a lab-made virtual impactor. Aerosol Sci. Technol. 2016, 51, 159–167. [Google Scholar] [CrossRef] [Green Version]
- Yuan, H.; Zhang, D.; Shi, Y.; Li, B.; Yang, J.; Yu, X.; Chen, N.; Kakikawa, M. Cell concentration, viability and culture composition of airborne bacteria during a dust event in Beijing. J. Environ. Sci. 2017, 55, 33–40. [Google Scholar] [CrossRef]
- Huang, H.-L.; Lee, M.-K.; Shih, H.-W. Assessment of Indoor Bioaerosols in Public Spaces by Real-Time Measured Airborne Particles. Aerosol Air Qual. Res. 2017, 17, 2276–2288. [Google Scholar] [CrossRef]
- Hsiao, P.-K.; Cheng, C.-C.; Chang, K.-C.; Yiin, L.-M.; Hsieh, C.-J.; Tseng, C.-C. Performance of CHROMagar VRE Medium for the Detection of Airborne Vancomycin-Resistant/Sensitive Enterococcus Species. Aerosol Sci. Technol. 2013, 48, 173–183. [Google Scholar] [CrossRef]
- Mirhoseini, S.H.; Nikaeen, M.; Satoh, K.; Makimura, K. Assessment of Airborne Particles in Indoor Environments: Applicability of Particle Counting for Prediction of Bioaerosol Concentrations. Aerosol Air Qual. Res. 2016, 16, 1903–1910. [Google Scholar] [CrossRef]
- Duquenne, P. On the Identification of Culturable Microorganisms for the Assessment of Biodiversity in Bioaerosols. Ann. Work. Expo. Health 2017, 62, 139–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jäckel, U.; Martin, E.; Schäfer, J. Heterogeneity in Cultivation-Based Monitoring of Airborne Bacterial Biodiversity in Animal Farms. Ann. Work. Expo. Health 2017, 61, 643–655. [Google Scholar] [CrossRef]
- Schäfer, J.; Weiß, S.; Jäckel, U. Preliminary Validation of a Method Combining Cultivation and Cloning-Based Approaches to Monitor Airborne Bacteria. Ann. Work. Expo. Health 2017, 61, 633–642. [Google Scholar] [CrossRef] [PubMed]
- Blais-Lecours, P.; Perrott, P.; Duchaine, C. Non-culturable bioaerosols in indoor settings: Impact on health and molecular approaches for detection. Atmos. Environ. 2015, 110, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Mbareche, H.; Veillette, M.; Bilodeau, G.J.; Duchaine, C. Fungal aerosols at dairy farms using molecular and culture techniques. Sci. Total Environ. 2019, 653, 253–263. [Google Scholar] [CrossRef]
- Unterwurzacher, V.; Pogner, C.; Berger, H.; Strauss, J.; Strauss-Goller, S.; Gorfer, M. Validation of a quantitative PCR based detection system for indoor mold exposure assessment in bioaerosols. Environ. Sci. Process. Impacts 2018, 20, 1454–1468. [Google Scholar] [CrossRef]
- Gaviria-Figueroa, A.; Preisner, E.C.; Hoque, S.; Feigley, C.E.; Norman, R.S. Emission and dispersal of antibiotic resistance genes through bioaerosols generated during the treatment of municipal sewage. Sci. Total. Environ. 2019, 686, 402–412. [Google Scholar] [CrossRef] [PubMed]
- Uhrbrand, K.; Koponen, I.K.; Schultz, A.C.; Madsen, A.M. Evaluation of air samplers and filter materials for collection and recovery of airborne norovirus. J. Appl. Microbiol. 2018, 124, 990–1000. [Google Scholar] [CrossRef]
- Coleman, K.K.; Sigler, W.V. Airborne Influenza A Virus Exposure in an Elementary School. Sci. Rep. 2020, 10, 1–7. [Google Scholar] [CrossRef]
- Allegra, S.; Riffard, S.; Leclerc, L.; Girardot, F.; Stauffert, M.; Forest, V.; Pourchez, J. A valuable experimental setup to model exposure to Legionella’s aerosols generated by shower-like systems. Water Res. 2020, 172, 115496. [Google Scholar] [CrossRef] [Green Version]
- Anderson, B.D.; Yondon, M.; Bailey, E.S.; Duman, E.K.; Simmons, R.A.; Greer, A.G.; Gray, G.C. Environmental bioaerosol surveillance as an early warning system for pathogen detection in North Carolina swine farms: A pilot study. Transbound. Emerg. Dis. 2021, 68, 361–367. [Google Scholar] [CrossRef] [PubMed]
- Orlofsky, E.; Benami, M.; Gross, A.; Dutt, M.; Gillor, O. Rapid MPN-Qpcr Screening for Pathogens in Air, Soil, Water, and Agricultural Produce. Water, Air Soil Pollut. 2015, 226, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Santos, R.; Sau, N.; Certucha, M.; Almendáriz, F.; Monge, A.; Zepeda, I.; Hernández, L. Rapid detection of bacteria, Enterococcus faecalis, in airborne particles of Hermosillo, Sonora, México. J. Environ. Biol. 2019, 40, 619–625. [Google Scholar] [CrossRef]
- Yin, H.; Wu, Z.; Shi, N.; Qi, Y.; Jian, X.; Zhou, L.; Tong, Y.; Cheng, Z.; Zhao, J.; Mao, H. Ultrafast multiplexed detection of SARS-CoV-2 RNA using a rapid droplet digital PCR system. Biosens. Bioelectron. 2021, 188, 113282. [Google Scholar] [CrossRef]
- Aoki, K.; Takai, K.; Nagasawa, T.; Kashiwagi, K.; Mori, N.; Matsubayashi, K.; Satake, M.; Tanaka, I.; Kodama, N.; Shimodaira, T.; et al. Combination of a SARS-CoV-2 IgG Assay and RT-PCR for Improved COVID-19 Diagnosis. Ann. Lab. Med. 2021, 41, 568–576. [Google Scholar] [CrossRef]
- Liu, Q.; Zhang, X.; Li, X.; Liu, S.; Sui, G. A semi-quantitative method for point-of-care assessments of specific pathogenic bioaerosols using a portable microfluidics-based device. J. Aerosol Sci. 2018, 115, 173–180. [Google Scholar] [CrossRef]
- Kwon, K.; Park, J.-W.; Hyun, K.-A.; Kwak, B.S.; Yong, D.E.; Hwang, J.; Jung, H.-I. Continuous adsorption and photothermal lysis of airborne bacteria using a gold-nanoparticle-embedded-geometrically activated surface interaction (gold-GASI) chip. Sens. Actuators B Chem. 2017, 248, 580–588. [Google Scholar] [CrossRef]
- Qiu, G.; Gai, Z.; Saleh, L.; Tang, J.; Gui, T.; Kullak-Ublick, G.A.; Wang, J. Thermoplasmonic-Assisted Cyclic Cleavage Amplification for Self-Validating Plasmonic Detection of SARS-CoV-2. ACS Nano 2021, 15, 7536–7546. [Google Scholar] [CrossRef]
- Cherkaoui, D.; Huang, D.; Miller, B.S.; Turbe, V.; McKendry, R.A. Harnessing recombinase polymerase amplification for rapid multi-gene detection of SARS-CoV-2 in resource-limited settings. Biosens. Bioelectron. 2021, 189, 113328. [Google Scholar] [CrossRef] [PubMed]
- He, Y.; Xie, T.; Tong, Y. Rapid and highly sensitive one-tube colorimetric RT-LAMP assay for visual detection of SARS-CoV-2 RNA. Biosens. Bioelectron. 2021, 187, 113330. [Google Scholar] [CrossRef]
- Yin, K.; Ding, X.; Xu, Z.; Li, Z.; Wang, X.; Zhao, H.; Otis, C.; Li, B.; Liu, C. Multiplexed colorimetric detection of SARS-CoV-2 and other pathogens in wastewater on a 3D printed integrated microfluidic chip. Sens. Actuators B Chem. 2021, 344, 130242. [Google Scholar] [CrossRef]
- King, M.D.; Lacey, R.E.; Pak, H.; Fearing, A.; Ramos, G.; Baig, T.; Smith, B.; Koustova, A. Assays and enumeration of bioaerosols-traditional approaches to modern practices. Aerosol Sci. Technol. 2020, 54, 611–633. [Google Scholar] [CrossRef]
- Bonifait, L.; Veillette, M.; Létourneau, V.; Grenier, D.; Duchaine, C. Detection of Streptococcus suis in Bioaerosols of Swine Confinement Buildings. Appl. Environ. Microbiol. 2014, 80, 3296–3304. [Google Scholar] [CrossRef] [Green Version]
- Chang, C.-W.; Lin, M.-H.; Huang, S.-H.; Horng, Y.-J. Parameters affecting recoveries of viable Staphylococcus aureus bioaerosols in liquid-based samplers. J. Aerosol Sci. 2019, 136, 82–90. [Google Scholar] [CrossRef]
- Chang, C.-W.; Hung, N.-T.; Chen, N.-T. Optimization and application of propidium monoazide-quantitative PCR method for viable bacterial bioaerosols. J. Aerosol Sci. 2017, 104, 90–99. [Google Scholar] [CrossRef]
- Fronczek, C.F.; Yoon, J.-Y. Biosensors for Monitoring Airborne Pathogens. J. Lab. Autom. 2015, 20, 390–410. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Langer, V.; Hartmann, G.; Niessner, R.; Seidel, M. Rapid quantification of bioaerosols containing L. pneumophila by Coriolis® μ air sampler and chemiluminescence antibody microarrays. J. Aerosol Sci. 2012, 48, 46–55. [Google Scholar] [CrossRef]
- Yoo, M.S.; Shin, M.; Kim, Y.; Jang, M.; Choi, Y.E.; Park, S.J.; Choi, J.; Lee, J.; Park, C. Development of electrochemical biosensor for detection of pathogenic microorganism in Asian dust events. Chemosphere 2017, 175, 269–274. [Google Scholar] [CrossRef]
- Kim, J.; Jin, J.-H.; Kim, H.S.; Song, W.; Shin, S.-K.; Yi, H.; Jang, D.-H.; Shin, S.; Lee, B.Y. Fully Automated Field-Deployable Bioaerosol Monitoring System Using Carbon Nanotube-Based Biosensors. Environ. Sci. Technol. 2016, 50, 5163–5171. [Google Scholar] [CrossRef]
- Shen, F.; Tan, M.; Wang, Z.; Yao, M.; Xu, Z.; Wu, Y.; Wang, J.; Guo, X.; Zhu, T. Integrating Silicon Nanowire Field Effect Transistor, Microfluidics and Air Sampling Techniques For Real-Time Monitoring Biological Aerosols. Environ. Sci. Technol. 2011, 45, 7473–7480. [Google Scholar] [CrossRef]
- Morris, D.R.; Fatisson, J.; Olsson, A.L.; Tufenkji, N.; Ferro, A.R. Real-time monitoring of airborne cat allergen using a QCM-based immunosensor. Sens. Actuators B Chem. 2014, 190, 851–857. [Google Scholar] [CrossRef] [Green Version]
- Farka, Z.; Kovar, D.; Skládal, P. Quartz crystal microbalance biosensor for rapid detection of aerosolized microorganisms. In Chemical, Biological, Radiological, Nuclear, and Explosives (CBRNE) Sensing XVI; International Society for Optics and Photonics: Bellingham, WA, USA, 2015; Volume 9455, p. 945507. [Google Scholar] [CrossRef]
- Kovar, D.; Farka, Z.; Skládal, P. Detection of Aerosolized Biological Agents Using the Piezoelectric Immunosensor. Anal. Chem. 2014, 86, 8680–8686. [Google Scholar] [CrossRef] [PubMed]
- Toma, K.; Miki, D.; Kishikawa, C.; Yoshimura, N.; Miyajima, K.; Arakawa, T.; Yatsuda, H.; Mitsubayashi, K. Repetitive Immunoassay with a Surface Acoustic Wave Device and a Highly Stable Protein Monolayer for On-Site Monitoring of Airborne Dust Mite Allergens. Anal. Chem. 2015, 87, 10470–10474. [Google Scholar] [CrossRef] [PubMed]
- Toma, K.; Harashima, Y.; Yoshimura, N.; Arakawa, T.; Yatsuda, H.; Kanamori, K.; Mitsubayashi, K. Semicontinuous Measurement of Mite Allergen (Der f 2) Using a Surface Acoustic Wave Immunosensor under Moderate pH for Long Sensor Lifetime. Sens. Mater. 2017, 29, 1679–1687. [Google Scholar]
- Toma, K.; Miki, D.; Yoshimura, N.; Arakawa, T.; Yatsuda, H.; Mitsubayashi, K. A gold nanoparticle-assisted sensitive SAW (surface acoustic wave) immunosensor with a regeneratable surface for monitoring of dust mite allergens. Sens. Actuators B Chem. 2017, 249, 685–690. [Google Scholar] [CrossRef]
- Toma, K.; Horibe, M.; Kishikawa, C.; Yoshimura, N.; Arakawa, T.; Yatsuda, H.; Shimomura, H.; Mitsubayashi, K. Rapid and repetitive immunoassay with a surface acoustic wave device for monitoring of dust mite allergens. Sens. Actuators B Chem. 2017, 248, 924–929. [Google Scholar] [CrossRef]
- Toma, K.; Oishi, K.; Kato, M.; Kurata, K.; Yoshimura, N.; Arakawa, T.; Yatsuda, H.; Kanamori, K.; Mitsubayashi, K. Precipitate-enhanced SAW immunosensor for sensitive monitoring of mite allergens. Sens. Actuators B Chem. 2019, 296, 126579. [Google Scholar] [CrossRef]
- Usachev, E.V.; Tam, A.M.; Usacheva, O.V.; Agranovski, I.E. The sensitivity of surface plasmon resonance based viral aerosol detection. J. Aerosol Sci. 2014, 76, 39–47. [Google Scholar] [CrossRef]
- Usachev, E.V.; Agranovski, E.; Usacheva, O.V.; Agranovski, I.E. Multiplexed Surface Plasmon Resonance based real time viral aerosol detection. J. Aerosol Sci. 2015, 90, 136–143. [Google Scholar] [CrossRef]
- Usachev, E.; Usacheva, O.; Agranovski, I. Surface plasmon resonance-based bacterial aerosol detection. J. Appl. Microbiol. 2014, 117, 1655–1662. [Google Scholar] [CrossRef]
- Qiu, G.; Yue, Y.; Tang, J.; Zhao, Y.-B.; Wang, J. Total Bioaerosol Detection by a Succinimidyl-Ester-Functionalized Plasmonic Biosensor To Reveal Different Characteristics at Three Locations in Switzerland. Environ. Sci. Technol. 2019, 54, 1353–1362. [Google Scholar] [CrossRef]
- Negron, A.; DeLeon-Rodriguez, N.; Waters, S.; Ziemba, L.D.; Anderson, B.; Bergin, M.; Konstantinidis, K.T.; Nenes, A. Using flow cytometry and light-induced fluorescence to characterize the variability and characteristics of bioaerosols in springtime in Metro Atlanta, Georgia. Atmos. Chem. Phys. Discuss. 2020, 20, 1817–1838. [Google Scholar] [CrossRef] [Green Version]
- Feeney, P.; Fernández-Rodríguez, S.; Molina, R.; McGillicuddy, E.; Hellebust, S.; Quirke, M.; Daly, S.; ÓConnor, D.; Sodeau, J. A comparison of on-line and off-line bioaerosol measurements at a biowaste site. Waste Manag. 2018, 76, 323–338. [Google Scholar] [CrossRef]
- Lu, C.; Zhang, P.; Wang, G.; Zhu, J.; Tang, X.; Huang, W.; Chen, S.; Xu, X.; Huang, H. Accurate measurement of airborne biological particle concentration based on laser-induced fluorescence technique. J. Aerosol Sci. 2018, 117, 24–33. [Google Scholar] [CrossRef]
- Gaudiuso, R.; Melikechi, N.; Abdel-Salam, Z.A.; Harith, M.A.; Palleschi, V.; Motto-Ros, V.; Busser, B. Laser-induced breakdown spectroscopy for human and animal health: A review. Spectrochim. Acta Part B At. Spectrosc. 2019, 152, 123–148. [Google Scholar] [CrossRef]
- Esquivel-Gonzalez, S.; Aizpuru, A.; Patrón-Soberano, A.; Arriaga, S. Characterization of bioaerosol emissions from two biofilters during treatment of toluene vapours using epifluorescence microscopy. Int. Biodeterior. Biodegrad. 2017, 123, 78–86. [Google Scholar] [CrossRef]
- Chen, L.-W.A.; Zhang, M.; Liu, T.; Fortier, K.; Chow, J.C.; Alonzo, F.; Kolberg, R.; Cao, J.; Lin, G.; Patel, T.Y.; et al. Evaluation of epifluorescence methods for quantifying bioaerosols in fine and coarse particulate air pollution. Atmos. Environ. 2019, 213, 620–628. [Google Scholar] [CrossRef]
- Nasir, Z.; Rolph, C.; Collins, S.; Stevenson, D.; Gladding, T.; Hayes, E.; Williams, B.; Khera, S.; Jackson, S.; Bennett, A.; et al. A Controlled Study on the Characterisation of Bioaerosols Emissions from Compost. Atmosphere 2018, 9, 379. [Google Scholar] [CrossRef] [Green Version]
- Gong, Z.; Pan, Y.L.; Videen, G.; Wang, C. Optical trapping-Raman spectroscopy (OT-RS) with embedded microscopy imaging for concurrent characterization and monitoring of physical and chemical properties of single particles. Anal. Chim. Acta 2018, 1020, 86–94. [Google Scholar] [CrossRef]
- Groulx, N.; Lecours, C.; Turgeon, N.; Volckens, J.; Tremblay, M.-E.; Duchaine, C. Nanoscale aerovirology: An efficient yet simple method to analyze the viral distribution of single bioaerosols. Aerosol Sci. Technol. 2016, 50, 732–739. [Google Scholar] [CrossRef] [Green Version]
- Valsan, A.E.; Priyamvada, H.; Ravikrishna, R.; Després, V.R.; Biju, C.; Sahu, L.K.; Kumar, A.; Verma, R.; Philip, L.; Gunthe, S.S. Morphological characteristics of bioaerosols from contrasting locations in southern tropical India—A case study. Atmos. Environ. 2015, 122, 321–331. [Google Scholar] [CrossRef]
- Park, J.-W.; Park, C.W.; Lee, S.H.; Hwang, J. Fast Monitoring of Indoor Bioaerosol Concentrations with ATP Bioluminescence Assay Using an Electrostatic Rod-Type Sampler. PLoS ONE 2015, 10, e0125251. [Google Scholar] [CrossRef]
- Kim, H.R.; An, S.; Hwang, J.; Park, J.H.; Byeon, J.H. In situ lysis droplet supply to efficiently extract ATP from dust particles for near-real-time bioaerosol monitoring. J. Hazard. Mater. 2019, 369, 684–690. [Google Scholar] [CrossRef] [PubMed]
- Nasrabadi, A.M.; Han, J.S.; Farid, M.M.; Lee, S.-G.; Hwang, J. Real-time separation of aerosolized Staphylococcus epidermidis and polystyrene latex particles with similar size distributions. Aerosol Sci. Technol. 2017, 51, 1389–1397. [Google Scholar] [CrossRef] [Green Version]
- Bryan, N.C.; Christner, B.C.; Guzik, T.G.; Granger, D.J.; Stewart, M.F. Abundance and survival of microbial aerosols in the troposphere and stratosphere. ISME J. 2019, 13, 2789–2799. [Google Scholar] [CrossRef]
- Hou, P.; Xu, Y.; Wang, H.; He, H. Detection of bovine viral diarrhea virus genotype 1 in aerosol by a real time RT-PCR assay. BMC Vet. Res. 2020, 16, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Kim, S.-J.; Bae, P.K.; Choi, M.; Keem, J.O.; Chung, W.; Shin, Y.-B. Fabrication and Application of Levan–PVA Hydrogel for Effective Influenza Virus Capture. ACS Appl. Mater. Interfaces 2020, 12, 29103–29109. [Google Scholar] [CrossRef] [PubMed]
- Miyajima, K.; Suzuki, Y.; Miki, D.; Arai, M.; Arakawa, T.; Shimomura, H.; Shiba, K.; Mitsubayashi, K. Direct analysis of airborne mite allergen (Der f1) in the residential atmosphere by chemifluorescent immunoassay using bioaerosol sampler. Talanta 2014, 123, 241–246. [Google Scholar] [CrossRef] [Green Version]
- Skladal, P.; Svabenska, E.; Žeravík, J.; Pribyl, J.; Šišková, P.; Tjarnhage, T.; Gustafson, I. Electrochemical Immunosensor Coupled to Cyclone Air Sampler for Detection of Escherichia coli DH5α in Bioaerosols. Electroanalysis 2011, 24, 539–546. [Google Scholar] [CrossRef]
- Rahmani, A.R.; Leili, M.; Azarian, G.; Poormohammadi, A. Sampling and detection of corona viruses in air: A mini review. Sci. Total. Environ. 2020, 740, 140207. [Google Scholar] [CrossRef] [PubMed]









| Detection Method | Target | Detection Range | Detection Time | LOD | References |
|---|---|---|---|---|---|
| Culture | Enterococcus | - | 24 h | 103 CFU/mL | [76] |
| PCR | Enterococcus faecalis | 1.5 × 103–1.5 × 108 CFU/mL | 72 min | 1.5 × 103 CFU/mL | [90] |
| RT-PCR | Bovine viral diarrhea virus | 5.2 × 100–5.2 × 108 RNA molecules | <30 min | 5.2 RNA molecules | [134] |
| RT-PCR | Influenza virus | 3.7 × 104–3.7 × 106 TCID50/mL | <50 min | 3.7 × 104 TCID50/mL | [135] |
| Chemiluminescence immunoassays | Legionella | 8 × 103–8 × 106 cells/mL | 1 h | 1 × 103 cells/mL | [104] |
| Chemiluminescence immunoassays | Dermatophagoides farinae | 0.49–250 ng/mL | - | 0.49 ng/mL | [136] |
| Electrochemical biosensor | Escherichia coli DH5a | 103–108 CFU/mL | 20 min | 150 CFU/mL | [137] |
| Electrochemical biosensor | Bacillus subtilis | 102–1010 CFU/mL | 10 min | 102 CFU/mL | [105] |
| FET biosensor | Alternaria alternate | 101–106 pg/mL | - | 10 pg/mL | [106] |
| QCM biosensor | Cat allergens | 5.2 × 100–1.6 × 105 ng/L | 30 min | 5.2 ng/L | [108] |
| QCM biosensor | Escherichia coli | 1.45 × 104–1.45 × 106 CFU/L | 16 min | 104 CFU/L | [109] |
| SAW biosensor | Dust mite allergens | 100–103 ng/mL | 24 min | 6.1 ng/mL | [111] |
| SAW biosensor | Dust mite allergens | 1.0–3000 ng/mL | 20 min | 6.3 ng/mL | [112] |
| SAW biosensor | Dust mite allergens | 0.3–1000 ng/mL | 36 min | 2.5 ng/mL | [113] |
| SAW biosensor | Dust mite allergens | 102–3 × 103 ng/mL | - | 20.1 ng/mL | [114] |
| SAW biosensor | Dust mite allergens | 0.08–1 ng/mL | - | 35 pg/mL | [115] |
| SPR biosensor | MS2 phage | 2.2 × 106–2.2 × 1011 PFU/mL | <1 min | 1.12 × 106 PFU/mL | [116] |
| SPR biosensor | Escherichia coli | 1.5 × 103–1.5 × 108 CFU/mL | - | 1.5 × 103 CFU/mL | [118] |
| ATP-based bioluminescence assay | Escherichia coli | 103–108 CFU/mL | 5 min | 2.32 × 103 CFU/mL | [55] |
| ATP-based bioluminescence assay | Escherichia coli | 3.7 × 101–3.7 × 107 CFU/mL | 5 min | 375 CFU/mL | [47] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, M.; Wang, L.; Qi, W.; Liu, Y.; Lin, J. Challenges and Perspectives for Biosensing of Bioaerosol Containing Pathogenic Microorganisms. Micromachines 2021, 12, 798. https://doi.org/10.3390/mi12070798
Li M, Wang L, Qi W, Liu Y, Lin J. Challenges and Perspectives for Biosensing of Bioaerosol Containing Pathogenic Microorganisms. Micromachines. 2021; 12(7):798. https://doi.org/10.3390/mi12070798
Chicago/Turabian StyleLi, Meixuan, Lei Wang, Wuzhen Qi, Yuanjie Liu, and Jianhan Lin. 2021. "Challenges and Perspectives for Biosensing of Bioaerosol Containing Pathogenic Microorganisms" Micromachines 12, no. 7: 798. https://doi.org/10.3390/mi12070798