In Situ Gel of Triamcinolone Acetonide-Loaded Solid Lipid Nanoparticles for Improved Topical Ocular Delivery: Tear Kinetics and Ocular Disposition Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.1.1. Animal Tissues and Animals
2.2. Methods
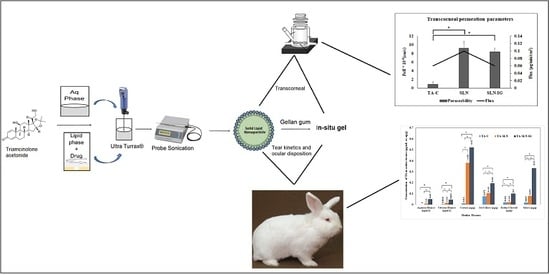
2.2.1. Preparation of TA-SLNs and TA-SLN-IG
2.2.2. Measurement of Particle Size, Zeta Potential, and Polydispersity Index
2.2.3. Chromatographic Conditions for Sample Analysis
2.2.4. Assay, Drug Loading, and Entrapment Efficiency
2.2.5. Measurement of pH, Rheological, and In Vitro Gelling Characteristics of TA-SLN-IG
2.2.6. Stability Studies
2.2.7. Differential Scanning Calorimetry (DSC)
2.2.8. Fourier Transform Infrared Spectroscopy (FTIR)
2.2.9. In Vitro Transcorneal Permeation Studies
2.2.10. Histology Studies
2.3. In Vivo Ocular Distribution Studies and Tear Kinetics
2.3.1. Sample Preparation
2.3.2. Bioanalytical Method
2.3.3. Statistical analysis
3. Results and Discussion
3.1. Preparation and Physical Characterization of TA-SLNs
3.2. Entrapment Efficiency, Drug Content, and Drug Loading of TA-SLNs
3.3. Preparation and Characterization of TA-SLN-IG
3.4. Stability Studies
3.5. Differential Scanning Calorimetry (DSC)
3.6. FTIR Studies
3.7. In Vitro Transcorneal Permeation
3.8. Corneal Histology
3.9. In Vivo Animal Studies
3.9.1. Tear Kinetics of TA-SLN and TA-SLN-IG
3.9.2. Ocular Distribution Studies of TA-SLN and TA-SLN-IG
4. Conclusion
Author Contributions
Funding
Conflicts of Interest
References
- Sarao, V.; Veritti, D.; Boscia, F.; Lanzetta, P. Intravitreal steroids for the treatment of retinal diseases. Sci. World. J. 2014. [Google Scholar] [CrossRef] [PubMed]
- Jermak, C.M.; Dellacroce, J.T.; Heffez, J.; Peyman, G.A. Triamcinolone acetonide in ocular therapeutics. Surv. Ophthalmol. 2007, 52, 503–522. [Google Scholar] [CrossRef] [PubMed]
- Degenring, R.F.; Jonas, J.B. Intravitreal injection of triamcinolone acetonide as treatment for chronic uveitis. Br. J. Ophthalmol. 2003, 87, 361. [Google Scholar] [CrossRef] [PubMed]
- Araújo, J.; Gonzalez-Mira, E.; Egea, M.A.; Garcia, M.L.; Souto, E.B. Optimization and physicochemical characterization of a triamcinolone acetonide-loaded NLC for ocular antiangiogenic applications. Int. J. Pharm. 2010, 393, 168–176. [Google Scholar] [CrossRef] [PubMed]
- Araújo, J.; Nikolic, S.; Egea, M.A.; Souto, E.B.; Garcia, M.L. Nanostructured lipid carriers for triamcinolone acetonide delivery to the posterior segment of the eye. Colloids. Surf. B Biointerf. 2011, 88, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Morrison, V.L.; Koh, H.J.; Cheng, L.; Bessho, K.; Davidson, M.C.; Freeman, W.R. Intravitreal toxicity of the kenalog vehicle (benzyl alcohol) in rabbits. Retina 2006, 26, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Jonas, J.B.; Kreissig, I.; Degenring, R. Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br. J. Ophthalmol. 2003, 87, 24–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gaudana, R.; Ananthula, H.K.; Parenky, A.; Mitra, A.K. Ocular Drug Delivery. AAPS. J. 2010, 12, 348–360. [Google Scholar] [CrossRef] [PubMed]
- Michael, S. Intravitreal Injection of Triamcinolone. Diabetes. Care 2004, 27, 1794–1796. [Google Scholar]
- Sánchez-López, E.; Espina, M.; Doktorovova, S.; Souto, E.B.; García, M.L. Lipid nanoparticles (SLN, NLC): Overcoming the anatomical and physiological barriers of the eye—Part I—Barriers and determining factors in ocular delivery. Eur. J. Pharm. Biopharm. 2017, 110, 70–75. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Espina, M.; Doktorovova, S.; Souto, E.B.; García, M.L. Lipid nanoparticles (SLN, NLC): Overcoming the anatomical and physiological barriers of the eye—Part II—Barriers and determining factors in ocular delivery. Eur. J. Pharm. Biopharm. 2017, 110, 58–69. [Google Scholar]
- Chodankar, R. Formulation and Characterisation of Triamcinolone Acetonide Emulgel. World J. Pharm. Pharm. Sci. 2017, 6, 1795–1810. [Google Scholar] [CrossRef]
- Clares, B.; Gallardo, V.; Medina, M.M.; Ruiz, M. Multilamellar liposomes of triamcinolone acetonide: Preparation, stability, and characterization. J. Liposome Res. 2009, 19, 197–206. [Google Scholar] [CrossRef]
- Altamirano-Vallejo, J.C.; Navarro-Partida, J.; Gonzalez-Dela, R.A.; Hsiao, J.H.; Olguín-Gutierrez, J.S.; Gonzalez-Villegas, A.C.; et al. Characterization and pharmacokinetics of triamcinolone acetonide-loaded liposomes topical formulations for vitreoretinal drug delivery. J. Ocul. Pharmacol. Ther. 2018, 34, 416–425. [Google Scholar] [CrossRef]
- Müller, R.H.; Mäder, K.; Gohla, S. Solid lipid nanoparticles (SLN) for controlled drug delivery—A review of the state of the art. Eur. J. Pharm. Biopharm. 2000, 50, 161–177. [Google Scholar] [CrossRef]
- Mehnert, W.; Mäder, K. Solid lipid nanoparticles. production, characterization and applications. Adv. Drug Deliv. Rev. 2012, 64, 83–101. [Google Scholar] [CrossRef]
- Hippalgaonkar, K.; Adelli, G.R.; Hippalgaonkar, K.; Repka, M.A.; Majumdar, S. Indomethacin-loaded solid lipid nanoparticles for ocular delivery: Development, characterization, and in vitro evaluation. J. Ocul. Pharmacol. Ther. 2013, 29, 216–228. [Google Scholar] [CrossRef]
- Balguri, S.P.; Adelli, G.R.; Janga, K.Y.; Bhagav, P.; Majumdar, S. Ocular disposition of ciprofloxacin from topical, pegylated nanostructured lipid carriers: Effect of molecular weight and density of poly (ethylene) glycol. Int. J. Pharm. 2017, 529, 32–43. [Google Scholar] [CrossRef]
- Mohanty, B.; Majumdar, D.K.; Mishra, S.K.; Panda, A.K.; Patnaik, S. Development and characterization of itraconazole-loaded solid lipid nanoparticles for ocular delivery. Pharm. Dev. Technol. 2015, 20, 458–464. [Google Scholar] [CrossRef]
- Agrawal, A.K.; Das, M.; Jain, S. In situ gel systems as ‘smart’ carriers for sustained ocular drug delivery. Expert. Opin. Drug Deliv. 2012, 9, 383–402. [Google Scholar] [CrossRef]
- Edsman, K.; Carlfors, J.; Petersson, R. Rheological evaluation of Poloxamer as an in situ gel for ophthalmic use. Eur. J. Pharm. Sci. 1998, 6, 105–112. [Google Scholar] [CrossRef]
- Gupta, H.; Velpandian, T.; Jain, S. Ion and pH-activated novel in-situ gel system for sustained ocular drug delivery. J. Drug. Target. 2010, 18, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Ceulemans, J.; Vinckier, I.; Ludwig, A. The use of xanthan gum in an ophthalmic liquid dosage form: Rheological characterization of the interaction with mucin. J. Pharm. Sci. 2002, 91, 1117–1127. [Google Scholar] [CrossRef] [PubMed]
- Janga, K.Y.; Tatke, A.; Balguri, S.P.; Lamichanne, S.P.; Ibrahim, M.M.; Maria, D.N.; Jablonski, M.M.; Majumdar, S. Ion-sensitive in situ hydrogels of natamycinbilosomes for enhanced and prolonged ocular pharmacotherapy: In vitro permeability, cytotoxicity and in vivo evaluation. Artif. Cells Nanomed. Biotechnol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Narendar, D.; Kishan, V. Candesartan cilexetil loaded solid lipid nanoparticles for oral delivery: Characterization, pharmacokinetic and pharmacodynamic evaluation. Drug Deliv. 2016, 23, 395–404. [Google Scholar]
- USP Monographs: Triamcinolone Acetonide. USP Off. Monogr. 2012, 35, pp. 4923–4924. Available online: https://www.drugfuture.com/Pharmacopoeia/usp35/PDF/4923-4924 Triamcinolone Acetonide.pdf (accessed on 10 July 2016).
- Majumdar, S.; Hippalgaonkar, K.; Srirangam, R. Vitreal kinetics of quinidine in rabbits in the presence of topically coadministered p-glycoprotein substrates/modulators. Drug. Metab. Dispos. 2009, 37, 1718–1725. [Google Scholar] [CrossRef] [PubMed]
- Prit, L.; Akash, P.; Pranjal, T.; Eman, A.; Soumyajit, M. Curcumin-loaded nanostructured lipid carriers for ocular drug delivery: Design optimization and characterization. J. Drug Deliv. Sci. Technol. 2018, 47, 159–166. [Google Scholar]
- Inactive Ingredient Search for Approved Drug Products. IIG Data Base—2017; FDA, 2017. Available online: https://www.accessdata.fda.gov/scripts/cder/iig/index.Cfm (accessed on 15 April 2017).
- Salminen, H.; Helgason, T.; Aulbach, S.; Kristinsson, B.; Kristbergsson, K.; Weiss, J. Influence of co-surfactants on crystallization and stability of solid lipid nanoparticles. J. Colloid Interface Sci. 2014, 426, 256–263. [Google Scholar] [CrossRef]
- Rakesh, K.; Sinha, V.R. Solid Lipid Nanoparticle: An efficient carrier for improved ocular permeation of voriconazole. Drug Dev. Ind. Pharm. 2016, 42, 1956–1967. [Google Scholar]
- Narendar, D.; Kishan, V. Improved anti-hyperlipidemic activity of rosuvastatin calcium via lipid nanoparticles: Pharmacokinetic and pharmacodynamic evaluation. Eur. J. Pharm. Biopharm. 2017, 110, 47–57. [Google Scholar]
- Rozier, A.; Mazuel, C.; Grove, J.; Plazonnet, B. Gelrite®: A novel, ion-activated, in-situ gelling polymer for ophthalmic vehicles. Effect on bioavailability of timolol. Int. J. Pharm. 1989, 57, 163–168. [Google Scholar] [CrossRef]
- Uddin, M.S.; Abdullah, A.M.; Kabir, M.T. Quality control tests for ophthalmic pharmaceuticals: Pharmacopoeial standards and specifications. J. Adv. Med. Pharm. Sci. 2017, 14, 1–17. [Google Scholar] [CrossRef]
- Pandurangan, D.K.; Bodagala, P.; Palanirajan, V.K.; Govindaraj, S. Formulation and evaluation of voriconazole ophthalmic solid lipid nanoparticles in situ gel. Int. J. Pharm. Investig. 2016, 6, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Jeong, H.; Hong, J.; Chang, M.; Kim, M.; Chuck, R.S.; Lee, J.K.; Park, C.-Y. The effect of silica nanoparticles on human corneal epithelial cells. Sci. Rep. 2016, 6, 37762. [Google Scholar]
- Balguri, S.P.; Adelli, G.R.; Majumdar, S. Topical ophthalmic lipid nanoformulations (SLN, NLC) of indomethacin for delivery to the posterior segment of ocular tissues. Eur. J. Pharm. Biopharm. 2016, 109, 224–235. [Google Scholar] [CrossRef] [PubMed]
- Attama, A.; Reichl, S.; Müller-Goymann, C. Sustained release and permeation of timolol from surface-modified solid lipid nanoparticles through bioengineered human cornea. Curr. Eye. Res. 2009, 34, 698–705. [Google Scholar] [CrossRef] [PubMed]
- Hao, J.; Wang, X.; Bi, Y.; Teng, Y.; Wang, J.; Li, F.; Li, Q.; Zhang, J.; Guo, F.; Liu, J. Fabrication of a composite system combining solid lipid nanoparticles and thermosensitive hydrogel for challenging ophthalmic drug delivery. Colloids. Surf. B Biointerfaces 2014, 114, 111–120. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Liu, Y.; Li, X.; Kebebe, D.; Zhang, B.; Ren, J.; Lu, J.; Li, J.; Du, S.; Liu, Z. Research progress of in-situ gelling ophthalmic drug delivery system. Asain J. Pharm. Sci. 2018. [Google Scholar] [CrossRef]
- Tayel, S.A.; El-Nabarawi, M.A.; Tadros, M.I.; Abd-Elsalam, W.H. Promising ion-sensitive in situ ocular nanoemulsion gels of terbinafine hydrochloride: Design, in vitro characterization and in vivo estimation of the ocular irritation and drug pharmacokinetics in the aqueous humor of rabbits. Int. J. Pharm. 2013, 443, 293–305. [Google Scholar] [CrossRef]
- Fernández-Ferreiro, A.; Fernández, B.N.; Varela, M.S.; Martínez, M.G.; Pardo, M.; Piñeiro, C.A.; Méndez, J.B.; Barcia, M.G.; Lamas, M.J.; Otero-Espinar, F. Cyclodextrin–polysaccharide-based, in situ-gelled system for ocular antifungal delivery. Beilstein J. Org. Chem. 2014, 10, 2903–2911. [Google Scholar] [CrossRef] [Green Version]






| Formulation Composition (%) | F1 | F2 | F3 | F4 | F5 * | F11 | F12 | F13 † | F14 | F15 | TA-C |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Triamcinolone acetonide | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | 4 |
| Glyceryl mono stearate (GMS) | 1.7 | 1 | 1.7 | 1.5 | 1.7 | 1.7 | 1.7 | 1.7 | 1.7 | 1.7 | - |
| Compritol® 888 ATO | 0.3 | 1 | 0.3 | 0.5 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | 0.3 | - |
| Tween ® 80 | 0.5 | 0.5 | 0.9 | 0.9 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | 0.75 | - |
| Pluronic® F-68 | 0.5 | 0.5 | 0.1 | 0.1 | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | 0.25 | - |
| Glycerin | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | 2.25 | - |
| Gellan gum | -- | -- | -- | -- | -- | 0.2 | 0.5 | 0.3 | 0.4 | 0.6 | - |
| Sodium Carboxy Methyl Cellulose | -- | -- | -- | -- | -- | -- | -- | -- | -- | -- | 0.5 |
| Water | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 | 100 |
| Formulation | Size (nm) | PDI | ZP (mV) | Entrapment Efficiency (%) | Assay (%) | Drug Loading (%) | Viscosity (cP) |
|---|---|---|---|---|---|---|---|
| F1 | 400 ± 6.3 | 0.47 ± 0.15 | −32.2 ± 2.4 | 91.4 ± 3.64 | 92.31 ± 1.31 | 4.96 ± 0.01 | 24.15 ± 2.6 |
| F2 | 197.9 ± 5.2 | 0.53 ± 0.23 | −38.1 ± 2.1 | 93.4 ± 2.1 | 81.45 ± 4.60 | 3.68 ± 0.01 | 22.62 ± 9.2 |
| F3 | 280.7 ± 3.6 | 0.55 ± 0.16 | −36.3 ± 1.9 | 90.0 ± 2.96 | 90.42 ± 5.70 | 4.95 ± 0.01 | 20.43 ± 2.7 |
| F4 | 360.5 ± 4.3 | 0.49 ± 0.11 | −35 ± 3.3 | 92.8 ± 2.37 | 85.2 ± 4.20 | 4.96 ± 0.01 | 22.91 ± 2.1 |
| F5 | 187.5 ± 1.8 | 0.35 ± 0.09 | −33 ± 2.5 | 95.1 ± 1.3 | 95.43 ± 5.33 | 4.98 ± 0.01 | 23.51 ± 3.5 |
| Formulation | Gellan Gum (%) | In vitro Gelling Time | Gel Residence Time (h) | Viscosity (cP) Without STF | Viscosity (cP) With STF |
|---|---|---|---|---|---|
| F11 | 0.2 | Immediate | 2–3 | 27.32 ± 3.2 | 105.6 ± 2.7 |
| F13 | 0.3 | Immediate | 6–7 | 43.8 ± 7.6 | 531.9 ± 6.2 |
| F 14 | 0.4 | Immediate | > 10 | 70.8 ± 15.5 | 1296.7 ± 8.9 |
| F 12 | 0.5 | Immediate | > 24 | 185.2 ± 20.3 | 2246.8 ± 5.4 |
| F 15 | 0.6 | Immediate | > 24 | 220.2 ± 20.3 | > 3024 |
| Duration | Condition | Size (nm) | PDI | Assay (%) | Entrapment Efficiency (%) |
|---|---|---|---|---|---|
| Day 1 | - | 187.5 ± 1.8 | 0.35 ± 0.09 | 95.42 ± 5.4 | 97.56 ± 2.3 |
| 4 °C | 188.3 ± 4.1 | 0.32 ± 0.11 | 92.94 ± 4.8 | 94.52 ± 3.3 | |
| Week 4 | 25 °C | 195.6 ±15.6 | 0.31 ± 0.13 | 91.65 ± 6.7 | 96.02 ± 1.8 |
| 40 °C | 200.3 ± 9.6 | 0.33 ± 0.21 | 89.55 ± 4.4 | 93.68 ± 2.7 |
| Pharmacokinetic Parameters | TA-C | TA-SLN | TA-SLN-IG |
|---|---|---|---|
| Cmax (µg/mL) | 42.2 | 9.75 | 13.38 # |
| tmax (h) | 1 | 1 | 2 # |
| AUC0-6 (µg·h/mL) | 26.52 ± 8.04 | 20.41 ± 2.07 | 29.99 ± 2.39 # |
| MRT (h) | 1.29 ± 0.42 | 2.04 ± 0.20 * | 2.75 ± 0.11 * |
| t1/2 (h) | 1.72 ± 0.29 | 3.76 ± 1.14 * | 3.54 ± 0.42 * |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tatke, A.; Dudhipala, N.; Janga, K.Y.; Balguri, S.P.; Avula, B.; Jablonski, M.M.; Majumdar, S. In Situ Gel of Triamcinolone Acetonide-Loaded Solid Lipid Nanoparticles for Improved Topical Ocular Delivery: Tear Kinetics and Ocular Disposition Studies. Nanomaterials 2019, 9, 33. https://doi.org/10.3390/nano9010033
Tatke A, Dudhipala N, Janga KY, Balguri SP, Avula B, Jablonski MM, Majumdar S. In Situ Gel of Triamcinolone Acetonide-Loaded Solid Lipid Nanoparticles for Improved Topical Ocular Delivery: Tear Kinetics and Ocular Disposition Studies. Nanomaterials. 2019; 9(1):33. https://doi.org/10.3390/nano9010033
Chicago/Turabian StyleTatke, Akshaya, Narendar Dudhipala, Karthik Yadav Janga, Sai Prachetan Balguri, Bharathi Avula, Monica M. Jablonski, and Soumyajit Majumdar. 2019. "In Situ Gel of Triamcinolone Acetonide-Loaded Solid Lipid Nanoparticles for Improved Topical Ocular Delivery: Tear Kinetics and Ocular Disposition Studies" Nanomaterials 9, no. 1: 33. https://doi.org/10.3390/nano9010033