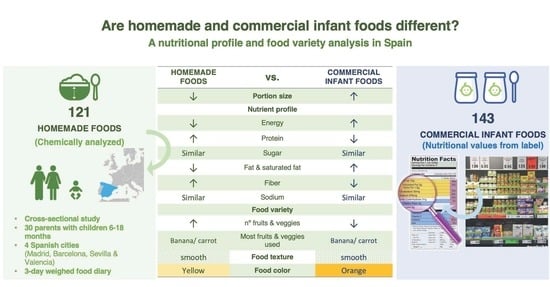
Are Homemade and Commercial Infant Foods Different? A Nutritional Profile and Food Variety Analysis in Spain
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Eligible Criteria
2.3. Study Procedure
2.3.1. Chemical Analysis of Nutrient Composition of HMFs Samples
2.3.2. CIFs in the Spanish Market
2.3.3. Food Variety
2.3.4. Food Texture and Colour
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Frequency and Type of HMFs and CIFs Consumed
3.3. Portion Size, Nutrient and Energy Profile Comparison between HMFs and CIFs
3.3.1. Meals
3.3.2. Fruits Purees
3.4. Food Variety
3.5. Food Texture and Colours in HMFs and CIFs
4. Discussion
4.1. Nutritional Profile Comparison
4.2. Food Variety, Texture and Colour Comparison
4.3. Limitations and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Schwartz, C.; Chabanet, C.; Lange, C.; Issanchou, S.; Nicklaus, S. The role of taste in food acceptance at the beginning of complementary feeding. Physiol. Behav. 2011, 104, 646–652. [Google Scholar] [CrossRef] [PubMed]
- Fewtrell, M.; Bronsky, J.; Campoy, C.; Domellof, M.; Embleton, N.; Fidler Mis, N.; Hojsak, I.; Hulst, J.M.; Indrio, F.; Lapillonne, A.; et al. Complementary Feeding: A Position Paper by the European Society for Paediatric Gastroenterology, Hepatology, and Nutrition (ESPGHAN) Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 119–132. [Google Scholar] [CrossRef]
- WHO. Guiding Principles for Complementary Feeding of the Breastfed Child. 2003. Available online: https://iris.paho.org/handle/10665.2/752/ (accessed on 15 March 2004).
- EFSA. EFSA Panel on Dietetic Products, Nutrition and Allergies. Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union. EFSA J. 2003, 11, 3408. [Google Scholar]
- EFSA. Scientific Opinion on the appropriate age for introduction of complementary feeding of infants. EFSA J. 2019, 17, 5780. [Google Scholar]
- SNE. Baby Foods Are a Targeted and Nutritionally Balanced Option during Weaning. 2019. Available online: https://www.specialisednutritioneurope.eu/wp-content/uploads/2019/07/2017110Final-SNE-Infographic-on-Baby-foods.pdf/ (accessed on 15 March 2020).
- Maslin, K.; Venter, C. Nutritional aspects of commercially prepared infant foods in developed countries: A narrative review. Nutr. Res. Rev. 2017, 30, 138–148. [Google Scholar] [CrossRef]
- Birch, L.; Savage, J.S.; Ventura, A. Influences on the Development of Children’s Eating Behaviours: From Infancy to Adolescence. Can. J. Diet. Pract. Res. 2007, 68, s1–s56. [Google Scholar] [PubMed]
- Ong, K.; Loos, R. Rapid infancy weight gain and subsequent obesity: Systematic reviews and hopeful suggestions. Acta Paediatr. 2006, 95, 904–908. [Google Scholar] [CrossRef]
- Huysentruyt, K.; Laire, D.; Van Avondt, T.; De Schepper, J.; Vandenplas, Y. Energy and macronutrient intakes and adherence to dietary guidelines of infants and toddlers in Belgium. Eur. J. Nutr. 2016, 55, 1595–1604. [Google Scholar] [CrossRef] [PubMed]
- Günther, A.L.B.; Buyken, A.E.; Kroke, A. Protein intake during the period of complementary feeding and early childhood and the association with body mass index and percentage body fat at 7 y of age. Am. J. Clin. Nutr. 2007, 85, 1623–1633. [Google Scholar] [CrossRef] [PubMed]
- Pimpin, L.; Jebb, S.; Johnson, L.; Wardle, J.; Ambrosini, G.L. Dietary protein intake is associated with body mass index and weight up to 5 y of age in a prospective cohort of twins. Am. J. Clin. Nutr. 2016, 103, 389–397. [Google Scholar] [CrossRef]
- WHO. Commercial Foods for Infants and Young Children in the WHO European Region. 2019. Available online: http://www.euro.who.int/en/health-topics/disease-prevention/nutrition/publications/2019/commercial-foods-for-infants-and-young-children-in-the-who-european-region-2019/ (accessed on 30 July 2019).
- WHO. Ending Inappropriate Promotion of Commercially Available Complementary Food for Infants and Young Children between 6 and 36 Months in Europe. 2019. Available online: http://www.euro.who.int/__data/assets/pdf_file/0004/406453/Ending_Final_3June2019.pdf?ua=1/ (accessed on 30 July 2019).
- HSC. Introducing Your Baby to Solid Food. Birth to Five. 2020. Available online: https://www.publichealth.hscni.net/sites/default/files/2020-05/Birth%20to%20five%202020%20-%20172%20pages.pdf/ (accessed on 30 June 2020).
- Synnott, K.; Bogue, J.; Edwards, C.A.; Scott, J.A.; Higgins, S.; Norin, E.; Frias, D.; Amarri, S.; Adam, R. Parental perceptions of feeding practices in five European countries: An exploratory study. Eur. J. Clin. Nutr. 2007, 61, 946–956. [Google Scholar] [CrossRef] [Green Version]
- Kostecka, M.; Jackowska, I.; Kostecka, J. Factors Affecting Complementary Feeding of Infants. A Pilot Study Conducted after the Introduction of New Infant Feeding Guidelines in Poland. Nutrients 2020, 13, 61. [Google Scholar] [CrossRef] [PubMed]
- NHS. Start 4 Life—What Is Weaning? Available online: https://www.nhs.uk/start4life/recipes/ (accessed on 12 February 2021).
- Public Health Dietitians—Vitalité Health Network. Guide and Recipes for Introducing Solid Food. Available online: https://www.vitalitenb.ca/sites/default/files/documents/intro_des_solides_bebes_fev_2019_en_liv_print.pdf/ (accessed on 12 February 2021).
- Southhampton Hospital Charity by NHS. Recipe Book for Babies Who Need to Get the Most Out of Every Mouthful. Available online: https://www.uhs.nhs.uk/Media/UHS-website-2019/Docs/Services/Child-health/DietaryAdvice/Recipe-book-For-babies-who-need-to-make-the-most-of-every-mouthful.pdf/ (accessed on 12 February 2021).
- Caroli, M.; Mele, R.M.; Tomaselli, M.A.; Cammisa, M.; Longo, F.; Attolini, E. Complementary feeding patterns in Europe with a special focus on Italy. Nutr. Metab. Cardiovasc. Dis. 2012, 22, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Koletzko, B.; Hirsch, N.L.; Jewell, J.M.; Dos Santos, Q.; Breda, J.; Fewtrell, M.; Weber, M.W. National Recommendations for Infant and Young Child Feeding in the World Health Organization European Region. J. Pediatr. Gastroenterol. Nutr. 2020, 71, 672–678. [Google Scholar] [CrossRef] [PubMed]
- Commission Directive 2006/125/EC of 5 December 2006 on Processed Cereal-Based Foods and Baby Foods for Infants and Young Children. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32006L0125&from=EN/ (accessed on 12 January 2020).
- Commission Regulation (EC) No 1881/2006 of 19 December 2006 Setting Maximum Levels for Certain Contaminants in Foodstuffs. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32006R1881&from=EN/ (accessed on 12 January 2020).
- Golley, R.K.; Smithers, L.G.; Mittinty, M.N.; Brazionis, L.; Emmett, P.; Northstone, K.; Campbell, K.; McNaughton, S.A.; Lynch, J.W. An index measuring adherence to complementary feeding guidelines has convergent validity as a measure of infant diet quality. J. Nutr. 2012, 142, 901–908. [Google Scholar] [CrossRef] [Green Version]
- Hilbig, A.; Foterek, K.; Kersting, M.; Alexy, U. Home-made and commercial complementary meals in German infants: Results of the DONALD study. J. Hum. Nutr. Diet. 2015, 28, 613–622. [Google Scholar] [CrossRef] [PubMed]
- Carstairs, S.A.; Craig, L.C.; Marais, D.; Bora, O.E.; Kiezebrink, K. A comparison of preprepared commercial infant feeding meals with home-cooked recipes. Arch. Dis. Child. 2016, 101, 1–6. [Google Scholar] [CrossRef]
- Foterek, K.; Buyken, A.E.; Bolzenius, K.; Hilbig, A.; Nöthlings, U.; Alexy, U. Commercial complementary food consumption is prospectively associated with added sugar intake in childhood. Br. J. Nutr. 2016, 115, 2067–2074. [Google Scholar] [CrossRef] [Green Version]
- Van den Boom, S.; Kimber, A.C.; Morgan, J.B. Nutritional composition of home-prepared baby meals in Madrid. Comparison with commercial products in Spain and home-made meals in England. Acta Paediatr. 1997, 86, 57–62. [Google Scholar] [CrossRef]
- Abeshu, M.A.; Adish, A.; Haki, G.D.; Lelisa, A.; Geleta, B. Assessment of Caregiver’s Knowledge, Complementary Feeding Practices, and Adequacy of Nutrient Intake from Homemade Foods for Children of 6–23 Months in Food Insecure Woredas of Wolayita Zone, Ethiopia. Front. Nutr. 2016, 3, 32. [Google Scholar] [CrossRef] [Green Version]
- Ortega, R.M.; Pérez-Rodrigo, C.; López-Sobaler, A.M. Dietary assessment methods: Dietary records. Nutr. Hosp. 2015, 31, 38–45. [Google Scholar] [CrossRef]
- Thompson, F.E.; Subar, A.F.; Coulston, C.J.; Boushey, M.G. (Eds.) Nutrition in the Prevention and Treatment of Disease, 4th ed.; Academic Press: San Diego, CA, USA, 2017; pp. 5–46. [Google Scholar]
- FAO. Dietary Assessment. A Resource Guide to Method Selection and Application in Low Resource Settings. Available online: http://www.fao.org/3/i9940en/I9940EN.pdf/ (accessed on 2 February 2019).
- Mennella, J.A. Ontogeny of taste preferences: Basic biology implications for health. Am. J. Clin. Nutr. 2014, 99, 704–711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Harris, G.; Coulthard, H. Early Eating Behaviours and Food Acceptance Revisited: Breastfeeding and Introduction of Complementary Foods as Predictive of Food Acceptance. Curr. Obes. Rep. 2016, 5, 113–120. [Google Scholar] [CrossRef] [Green Version]
- Tournier, C.; Bernad, C.; Madrelle, J.; Delarue, J.; Cuvelier, G.; Schwartz, C.; Nicklaus, S. Fostering infant food texture acceptance: A pilot intervention promoting food texture introduction between 8 and 15 months. Appetite 2020, 158, 104989. [Google Scholar] [CrossRef]
- Krebs-Smith, S.M.; Smiciklas-Wright, H.; Guthrie, H.A.; Krebs-Smith, J. The effects of variety in food choices on dietary quality. J. Am. Diet. Assoc. 1987, 87, 897–903. [Google Scholar]
- Nicklaus, S. Development of food variety in children. Appetite 2009, 52, 253–255. [Google Scholar] [CrossRef] [PubMed]
- Nicklaus, S. The role of food experiences during early childhood in food pleasure learning. Appetite 2016, 104, 3–9. [Google Scholar] [CrossRef]
- Nwaru, B.I.; Takkinen, H.M.; Kaila, M.; Erkkola, M.; Ahonen, S.; Pekkanen, J.; Simell, O.; Veijola, R.; Ilonen, J.; Hyöty, H.; et al. Food diversity in infancy and the risk of childhood asthma and allergies. J. Allergy Clin. Immunol. 2014, 133, 1084–1091. [Google Scholar] [CrossRef] [PubMed]
- Maslin, K.; Galvin, A.D.; Shepherd, S.; Dean, T.; Dewey, A.; Venter, C. A qualitative study of mothers’ perceptions of weaning and the use of commercial infant food in the United Kingdom. Matern. Paediatr. Nutr. J. 2015, 1, 1000103. [Google Scholar] [CrossRef] [Green Version]
- Mesch, C.M.; Stimming, M.; Foterek, K.; Hilbig, A.; Alexy, U.; Kersting, M.; Libuda, L. Food variety in commercial and HM complementary meals for infants in Germany. Market survey and dietary practice. Appetite 2014, 76, 113–119. [Google Scholar] [CrossRef]
- AOAC. Official Methods of Analysis of the Association of Official Analytical Chemists, 15th ed.; Association of Official Analytical Chemists: Arlington, TX, USA, 1990. [Google Scholar]
- Folch, J.; Less, M.; Stoane-Stanley, G.H. A simple method for the isolation and purification of total lipids from animal tissues. J. Biol. Chem. 1957, 226, 497–509. [Google Scholar] [CrossRef]
- FAO. Food Energy: Methods of Analysis and Conversion Factors: Report of a Technical Workshop. 2003. Available online: http://www.fao.org/uploads/media/FAO_2003_Food_Energy_02.pdf/ (accessed on 12 May 2020).
- Götz, H. Analysis of Carbohydrates in Food by HPLC; Hewlett Packard Application: Palo Alto, CA, USA, 1980. [Google Scholar]
- Prosky, L.; Asp, N.-G.; Furda, I.; DeVries, J.W.; Schweizer, T.F.; Harland, B.F. Determination of total dietary fiber in foods and food products: Collaborative study. J. AOAC Int. 1985, 68, 677–679. [Google Scholar] [CrossRef]
- AOAC. FAO Method 991.43 Total, Soluble and Insoluble Fiber in Foods. Enzymatic-Gravimetric Method 32.1.17. First Action 1991. Final Action 1994. Official Methods of Analysis, 16th ed.; AOAC Int.: Gaithersburg, MD, USA, 1996. [Google Scholar]
- Ros, G.; Abellán, P.; Rincón, F.; Periago, M.J. Electrolyte composition of meat-based infants beikosts. J. Food Compos. Anal. 1994, 7, 282–290. [Google Scholar] [CrossRef]
- Garcia, A.L.; Raza, S.; Parrett, A.; Wright, C.M. Nutritional content of infant commercial weaning foods in the UK. Arch. Dis. Child 2013, 98, 793–797. [Google Scholar] [CrossRef]
- Garcia, A.L.; McLean, K.; Wright, C.M. Types of fruits and vegetables used in commercial baby foods and their contribution to sugar content. Matern. Child Nutr. 2016, 12, 838–847. [Google Scholar] [CrossRef] [PubMed]
- USDA. Infant Nutrition and Feeding. A Guide for Use in the WIC and CSF Programs. 2019. Available online: https://wicworks.fns.usda.gov/sites/default/files/media/document/Infant_Nutrition_and_Feeding_Guide.pdf (accessed on 20 June 2019).
- Crawley, H. Eating Well the First Year: A Guide to Introducing Solids and Eating Well up to Baby’s First Birthday. 2015. Available online: https://static1.squarespace.com/static/59f75004f09ca48694070f3b/t/5a5a41479140b7e31a75ccbc/1515864404727/Eating_well_the_first_year_Sep_17_small.pdf/ (accessed on 5 April 2017).
- Damianidi, L.; Gruszfeld, D.; Verduci, E.; Vecchi, F.; Xhonneux, A.; Langhendries, J.P.; Luque, V.; Theurich, M.A.; Zaragoza-Jordana, M.; Koletzko, B.; et al. Protein intakes and their nutritional sources during the first 2 years of life: Secondary data evaluation from the European Childhood Obesity Project. Eur. J. Clin. Nutr. 2016, 70, 1291–1297. [Google Scholar] [CrossRef] [PubMed]
- Hörnell, A.; Lagström, H.; Lande, B.; Thorsdottir, I. Protein intake from 0 to 18 years of age and its relation to health: A systematic literature review for the 5th Nordic Nutrition Recommendations. Food Nutr. Res. 2013, 57, 1–42. [Google Scholar] [CrossRef] [Green Version]
- Thibault, J.F.; Lahaye, M.; Guillon, F. Physico-chemical Properties of Food Plant Cell Walls. In Dietary Fiber—A Component of Food. ILSI Human Nutrition Reviews; Schweizer, T.F., Edwards, C.A., Eds.; Springer: London, UK, 1992. [Google Scholar]
- Colin-Henrion, M.; Mehinagic, E.; Renard, C.; Richomme, P.; Frédérique Jourjon, F. From apple to applesauce: Processing effects on dietary fibers and cell wall polysaccharides. Food Chem. 2009, 117, 254–260. [Google Scholar] [CrossRef] [Green Version]
- Dahl, W.J.; Stewart, M.L. Position of the Academy of Nutrition and Dietetics: Health Implications of Dietary Fiber. J. Acad. Nutr. Diet. 2015, 115, 1861–1870. [Google Scholar] [CrossRef]
- Edwards, C.A.; Parrett, A.M. Intestinal flora during the first months of life: New perspectives. Br. J. Nutr. 2002, 88, S11–S18. [Google Scholar] [CrossRef] [PubMed]
- Cai, Y.; Folkerts, J.; Folkerts, G.; Maurer, M.; Braber, S. Microbiota-dependent and -independent effects of dietary fiber on human health. Br. J. Pharmacol. 2020, 177, 1363–1381. [Google Scholar] [CrossRef] [Green Version]
- AEP. Recomendaciones de la Asociación Española de Pediatría Sobre la Alimentación Complementaria 2018. Available online: https://www.aeped.es/sites/default/files/documentos/recomendaciones_aep_sobre_alimentacio_n_complementaria_nov2018_v3_final.pdf/ (accessed on 10 January 2020).
- Muñoz, M.T.; Suárez, L. Manual Práctico de Nutrición en Pediatría; Asociación Española de Pediatría: Madrid, Spain, 2007; Available online: https://www.aeped.es/sites/default/files/documentos/manual_nutricion.pdf./ (accessed on 2 August 2020).
- Bouhlal, S.; Issanchou, S.; Chabanet, C.; Nicklaus, S. “Just a pinch of salt”. An experimental comparison of the effect of repeated exposure and flavor-flavor learning with salt or spice on vegetable acceptance in young children. Appetite 2014, 83, 209–217. [Google Scholar] [CrossRef]
- Bouhlal, S.; Issanchou, S.; Nicklaus, S. The impact of salt, fat and sugar levels on toddler food intake. Br. J. Nutr. 2011, 105, 645–653. [Google Scholar] [CrossRef] [Green Version]
- Stein, L.J.; Cowart, B.J.; Beauchamp, G.K. The development of salty taste acceptance is related to dietary experience in human infants: A prospective study. Am. J. Clin. Nutr. 2012, 95, 123–129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fitzhugh, K.; Lobstein, T. Children’s Food Examined: An Analysis of 358 Products Targeted at Children; The Food Commission: London, UK, 2000; Available online: http://www.foodcomm.org.uk/pdfs/Childrens_Food_Examined.pdf/ (accessed on 6 June 2020).
- Ahern, S.M.; Caton, S.J.; Bouhlal, S.; Hausner, H.; Olsen, A.; Nicklaus, S.; Møller, P.; Hetherington, M.M. Eating a Rainbow. Introducing vegetables in the first years of life in 3 European countries. Appetite 2013, 71, 48–56. [Google Scholar] [CrossRef]
- Koletzko, B.; Lien, E.; Agostoni, C.; Böhles, H.; Campoy, C.; Cetin, I.; Decsi, T.; Dudenhausen, J.W.; Dupont, C.; Forsyth, S.; et al. The roles of long-chain polyunsaturated fatty acids in pregnancy, lactation and infancy: Review of current knowledge and consensus recommendations. J. Perinat. Med. 2008, 36, 5–14. [Google Scholar] [CrossRef] [Green Version]
- Koletzko, B.; Uauy, R.; Palou, A.; Kok, F.; Hornstra, G.; Eilander, A.; Moretti, D.; Osendarp, S.; Zock, P.; Innis, S. Dietary intake of eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) in children—A workshop report. Br. J. Nutr. 2010, 103, 923–928. [Google Scholar] [CrossRef] [Green Version]
- Varela-Moreiras, G.; Ávila, J.M.; Cuadrado, C.; del Pozo, S.; Ruiz, E.; Moreiras, O. Evaluation of food consumption and dietary patterns in Spain by the Food Consumption Survey: Updated information. Eur. J. Clin. Nutr. 2010, 64, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Blossfield, I.; Collins, A.; Kiely, M.; Delahunty, C. Texture preferences of 12-month-old infants and the role of early experiences. Food Qual. Prefer. 2006, 18, 396–404. [Google Scholar] [CrossRef]
- Foterek, K.; Hilbig, A.; Alexy, U. Associations between commercial complementary food consumption and fruit and vegetable intake in children. Results of the DONALD study. Appetite 2015, 85, 84–90. [Google Scholar] [CrossRef]
- Moumin, N.; Green, T.; Golley, R.; Netting, M. Are the Nutrient and Textural Properties of Australian Commercial Infant and Toddler Foods Consistent with Infant Feeding Advice? Br. J. Nutr. 2020, 1–19. [Google Scholar] [CrossRef]
- Minich, D.M. A Review of the Science of Colorful, Plant-Based Food and Practical Strategies for “Eating the Rainbow”. J. Nutr. Metab. 2019, 2019, 2125070. [Google Scholar] [CrossRef] [PubMed]
- Cömert, E.D.; Mogol, B.A.; Gökmen, V. Relationship between color and antioxidant capacity of fruits and vegetables. Curr. Res. Nutr. Food Sci. 2020, 2, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Melendez-Martinez, A.J.; Britton, G.; Vicario, I.M.; Heredia, F.J. Relationship between the colour and the chemical structure of carotenoid pigments. Food Chem. 2007, 101, 1145–1150. [Google Scholar] [CrossRef]
- Retondario, A.; Silva, D.L.; Salgado, S.M.; Alves, M.A.; Ferreira, S.M. Nutritional composition of school meals serving children from 7 to 36 months of age in municipal day-care centres in the metropolitan area of Curitiba, Paraná, Brazil. Br. J. Nutr. 2016, 115, 2203–2211. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Randhawa, S.; Kakùda, Y.; Wong, C.L.; Yeung, D. Microbial Safety, Nutritive Value and Residual Pesticide Levels are Comparable among Commercial, Laboratory and Homemade Baby Food Samples—A Pilot Study. Open Nutr. J. 2012, 6, 89–96. [Google Scholar] [CrossRef]
- Garcia, A.L.; Curtin, L.; Ronquillo, J.D.; Parrett, A.; Wright, C.M. Changes in the UK baby food market surveyed in 2013 and 2019: The rise of baby snacks and sweet/savoury foods. Arch. Dis. Child 2020, 105, 1162–1166. [Google Scholar] [CrossRef]


| 6–11 Months (n = 17) | 12–18 Months (n = 13) | |
|---|---|---|
| Characteristic of the children | ||
| Age (months) (mean ± SD) | 8.3 ± 1.4 | 14.4 ± 1.9 |
| Gender (% Male) | 58.8 | 84.6 |
| Birth weight (g) (mean ± SD) 1 | 3173.3 ± 455.0 | 3178.9 ± 451.3 |
| Actual weight (kg) (mean ± SD) | 8.6 ± 1.3 | 10.6 ± 1.2 |
| Attend day-care (%) 1 | 16.7 | 68.8 |
| Total complementary food intake (g/day) | 465.6 ± 185.5 | 690.0 ± 243.0 * |
| Commercial infant cereals intake (g/day) | 50.8 ± 27.7 | 22.5 ± 13.1 * |
| BM/Formula intake (mL/day) | 677.4 ± 228.0 | 350.9 ± 234.5 * |
| Characteristic of the mothers 1 | ||
| Age (years) (mean ± SD) | 32.5 ± 4.5 | 35.1 ± 5.2 |
| Education (%) | ||
| Primary school | 46.7 | 12.5 |
| High school | 33.3 | 37.5 |
| Some college | 33.3 | 31.3 |
| Univ. or above | 16.7 | 18.8 |
| Main activity (%) | ||
| Employed | 50.0 | 69.0 |
| Student | 8.3 | 0 |
| Unemployed | 41.7 | 31.0 |
| Family Status (%) | ||
| Single/divorced | 8.3 | 6.3 |
| Married | 75.0 | 62.5 |
| Couple | 16.7 | 31.3 |
| 6–11 Months (n = 17) | 12–18 Months (n = 13) | |||||
|---|---|---|---|---|---|---|
| Type of food | HMFs | CIFs | p Value | HMFs | CIFs | p Value |
| Number of infant or young children who consume (%) | 17 (100%) | 9 (53%) | 13 (100%) | 4 (31%) | ||
| Fruit purees intake (g/day) 1 | 106.1 ± 68.9 | 75.5 ± 34.6 | 0.20 | 166.1 ± 99.9 | 86.7 ± 0 | 0.50 |
| Meals intake (g/day) 1 | 186.9 ± 115.5 | 83.3 ± 29.6 | 0.15 | 191.1 ± 105.7 | 70.8 ± 8.3 | 0.042 |
| Meals (%) 2 | 94 | 18 | 100 | 31 | ||
| Meat (%) 1 | 82 | 12 | 85 | 23 | ||
| Fish (%) 1 | 65 | 12 | 69 | 8 | ||
| Vegetables (%) 1 | 12 | - | 38 | - | ||
| Fruits purees (%) 1 | 70 | 53 | 46 | 8 | ||
| 6–11 Months (n = 17) | 12–18 Months (n = 13) | Overall (p Value) 1 | ||||||
|---|---|---|---|---|---|---|---|---|
| HMFs | CIFs | p Value | HMFs | CIFs | p Value | HMFs | CIFs | |
| Meals (n) | 48 | 94 | 38 | 10 | ||||
| Portion size (g/meal) 2 | 185.5 (138.7, 211.5) | 200.0 (200.0, 250.0) | ≤0.001 | 218.0 (113.5, 254.5) | 250.0 (246.2, 250.0) | 0.04 | 0.30 | ≤0.001 |
| Energy (kcal) | 48.0 (34.5, 54.6) | 68.5 (64.0, 71.0) | ≤0.001 | 66.2 (52.8, 80.0) | 69.5 (66.0, 72.0) | 0.49 | ≤0.001 | 0.37 |
| Protein (g) | 3.6 (2.9, 4.3) | 3.0 (2.6, 3.6) | 0.002 | 3.8 (3.4, 4.6) | 2.9 (2.6, 3.0) | ≤0.001 | 0.21 | 0.24 |
| Carbohydrates (g) | 3.9 (2.9, 5.0) | 8.4 (7.6, 9.2) | ≤0.001 | 5.1 (3.6, 6.4) | 7.9 (7.3, 9.0) | ≤0.001 | 0.03 | 0.48 |
| Sugar (g) | 1.3 (1.0, 1.5) | 1.3 (0.9, 1.8) | 0.60 | 1.4 (0.8, 2.1) | 1.3 (1.1, 1.8) | 0.85 | 0.49 | 0.85 |
| Fiber (g) | 2.6 (2.0, 3.0) | 0.8 (0.5, 1.0) | ≤0.001 | 2.0 (1.4, 2.8) | 0.8 (0.8, 1.0) | ≤0.001 | 0.03 | 0.15 |
| Fat (g) | 1.5 (0.6, 2.1) | 2.3 (2.2, 2.5) | ≤0.001 | 2.7 (1.2, 4.5) | 2.5 (2.4, 2.7) | 0.79 | ≤0.001 | ≤0.001 |
| Saturated (g) | 0.3 (0.1, 0.35) | 0.6 (0.5, 0.7) | ≤0.001 | 0.4 (0.3, 0.7) | 0.5 (0.5, 7.2) | 0.11 | ≤0.001 | 0.68 |
| Sodium (mg) | 34.4 (23.1, 56.0) | 28.0 (28.0, 48.0) | 0.86 | 65.2 (39.5, 126.1) | 111.0 (93.0, 140.0) | 0.04 | ≤0.001 | ≤0.001 |
| Fruit purees (n) | 22 | 29 | 13 | 10 | ||||
| Portion size (g/fruit) 2 | 172.0 (129.5, 214.7) | 200.0 (95.0, 250.0) | 0.77 | 206.0 (188.5, 245.0) | 100.0 (90.0, 113.0) | ≤0.001 | 0.048 | 0.01 |
| Energy (kcal) | 69.2 (64.7, 71.9) | 72.0 (69.5, 78.5) | 0.06 | 78.0 (63.2, 84.8) | 61.0 (56.7, 63.0) | 0.02 | 0.06 | ≤0.001 |
| Protein (g) | 1.0 (0.9, 1.2) | 0.8 (0.7, 1.0) | 0.003 | 1.0 (0.7, 1.1) | 0.8 (0.5, 0.8) | 0.02 | 0.57 | 0.28 |
| Carbohydrates (g) 3 | 15.3 ± 2.5 | 16.0 ± 2.3 | 0.30 | 16.3 ± 3.3 | 13.0 ± 0.70 | 0.005 | 0.30 | ≤0.001 |
| Sugar (g) 3 | 12.6 ± 1.4 | 11.9 ± 2.2 | 0.26 | 11.9 ± 1.9 | 11.7 ± 0.7 | 0.77 | 0.22 | 0.60 |
| Fiber (g) 3 | 2.1 ± 0.2 | 1.3 ± 0.5 | ≤0.001 | 1.9 ± 0.28 | 1.6 ± 0.48 | 0.13 | 0.02 | 0.11 |
| Fat (g) | 0.6 (0.2, 0.7) | 0.2 (0.1, 0.4) | 0.005 | 0.6 (0.2, 0.5) | 0.2 (0.1, 0.3) | 0.02 | 0.42 | 0.79 |
| Saturated (g) | 0.3 (0.2, 0.3) | - | ≤0.001 | 0.3 (0.1, 0.5) | - | ≤0.001 | 0.69 | 0.47 |
| Sodium (mg) | 21.7 (19.8, 21.7) | 12.0 (6.0, 16.0) | ≤0.001 | 21.7 (17.6, 30.1) | 12.0 (12.0, 20.0) | 0.003 | 0.57 | 0.10 |
| 6–11 Months 1 | 12–18 Months 1 | |||
|---|---|---|---|---|
| Meal purees | HMFs (n = 48) | CIFs (n = 94) | HMFs (n = 38) | CIFs (n = 10) |
| Vegetable type 1 | ||||
| Carrot | 64.6 (16.7) | 80.8 (52.9) | 94.7 (23.7) | 90.0 (30.0) |
| Zucchini | 68.7 (47.9) | 1.9 (1.0) | 73.7 (44.7) | 10.0 (-) |
| Green beans | 58.3 (8.3) | 22.1 (8.6) | 63.1 (10.5) | - |
| Onion | 33.3 (10.4) | 79.8 (3.8) | 52.6 (13.1) | 80.0 (-) |
| Tomato | 27.1 (6.2) | 41.3 (15.4) | 7.9 (-) | 80.0 (70.0) |
| Leek | 47.9 (-) | 6.7 (1.9) | 34.2 (2.6) | 20.0 (-) |
| Pumpkin | 50.0 (10.4) | 1.0 (-) | 15.8 (5.3) | - |
| Celery | 6.2 (-) | 20.2 (-) | 2.6 (-) | 30.0 (-) |
| Peas | 8.3 (-) | 37.5 (6.7) | 2.6 (-) | 30.0 (-) |
| Pepper | - | 1.9 (-) | 5.3 (-) | 20.0 (-) |
| Broccoli | 4.2 (2.1) | - | 2.6 (-) | 10.0 (-) |
| Chard | - | - | 13.1 (-) | |
| Fennel | - | - | - | 10.0 (-) |
| Turnip | - | - | 7.9 (-) | - |
| Parsnip | - | 2.9 (-) | 2.6 (-) | - |
| Lettuce | - | 2.6 (-) | ||
| Spinach | - | 1.4 (-) | - | - |
| Fruit purees | HMFs (n = 22) | CIFs (n = 29) | HMFs (n = 13) | CIFs (n = 10) |
| Fruit type 1 | ||||
| Banana | 86.4 (4.5) | 93.1 (34.5) | 100.0 (15.4) | 100.0 (40.0) |
| Apple | 72.7 (22.7) | 86.2 (44.8) | 84.6 (61.5) | 70.0 (30.0) |
| Pear | 90.9 (31.8) | 27.6 (6.9) | 76.9 (7.7) | 50.0 (10.0) |
| Orange | 68.2 (36.4) | 10.3 (6.9) | 61.5 (7.7) | - |
| Peach | 4.5 (4.5) | 31.0 (3.4) | - | 20.0 (-) |
| Mandarin | 4.5 (-) | 10.3 (3.4) | 7.7 (7.7) | - |
| Apricot | - | 10.3 (-) | - | 20.0 (-) |
| Kiwi | - | 3.4 (-) | - | 20.0 (-) |
| Strawberry | - | - | - | 20.0 (-) |
| Plum | - | 3.4 (-) | 15.4 (-) | - |
| Mango | - | 6.9 (-) | - | 10.0 (-) |
| Pineapple | - | 3.4 (-) | - | 10.0 (-) |
| Passion fruit | - | - | - | 10.0 (-) |
| Raspberry | - | 3.4 (-) | - | - |
| Cranberry | - | 3.4 (-) | - | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernal, M.J.; Roman, S.; Klerks, M.; Haro-Vicente, J.F.; Sanchez-Siles, L.M. Are Homemade and Commercial Infant Foods Different? A Nutritional Profile and Food Variety Analysis in Spain. Nutrients 2021, 13, 777. https://doi.org/10.3390/nu13030777
Bernal MJ, Roman S, Klerks M, Haro-Vicente JF, Sanchez-Siles LM. Are Homemade and Commercial Infant Foods Different? A Nutritional Profile and Food Variety Analysis in Spain. Nutrients. 2021; 13(3):777. https://doi.org/10.3390/nu13030777
Chicago/Turabian StyleBernal, Maria Jose, Sergio Roman, Michelle Klerks, Juan Francisco Haro-Vicente, and Luis Manuel Sanchez-Siles. 2021. "Are Homemade and Commercial Infant Foods Different? A Nutritional Profile and Food Variety Analysis in Spain" Nutrients 13, no. 3: 777. https://doi.org/10.3390/nu13030777