The Bradyzoite: A Key Developmental Stage for the Persistence and Pathogenesis of Toxoplasmosis
Abstract
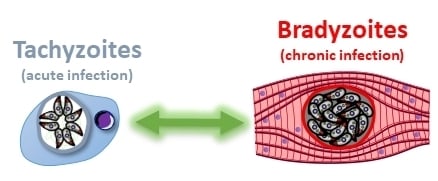
:1. Introduction
2. Importance of the Bradyzoites for the Pathology of Toxoplasmosis
2.1. Escaping the Immune System
2.2. The Differentiation Process
2.3. Reactivation
3. Immune Detection and Control of Bradyzoites
4. Current Research Strategies for Interfering with the Tachyzoite-Bradyzoite Interconversion
4.1. Blocking the Differentiation Process by Shutting down Transcriptional or Translational Programs
4.2. Interfering with the Biogenesis or the Integrity of the Cyst Wall
4.3. Identifying Metabolic Weak Spots
5. New Tools for Studying Bradyzoite Biology
5.1. Improved in vitro Differentiation Models
5.2. Tools for Genetic Engineering of Mutant Bradyzoites
5.3. Emerging Tools for the Phenotypic Characterization of Bradyzoites
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Dubey, J.P. The history and life cycle of Toxoplasma gondii. In Toxoplasma Gondii; Elsevier: Amsterdam, The Netherlands, 2014; pp. 1–17. ISBN 978-0-12-396481-6. [Google Scholar]
- Shapiro, K.; Bahia-Oliveira, L.; Dixon, B.; Dumètre, A.; de Wit, L.A.; VanWormer, E.; Villena, I. Environmental transmission of Toxoplasma gondii: Oocysts in water, soil and food. Food Waterborne Parasitol. 2019, 15, e00049. [Google Scholar] [CrossRef] [PubMed]
- Montoya, J.G.; Liesenfeld, O. Toxoplasmosis. Lancet 2004, 363, 1965–1976. [Google Scholar] [CrossRef]
- McAuley, J.B. Congenital Toxoplasmosis. J. Pediatr. Infect. Dis. Soc. 2014, 3, S30–S35. [Google Scholar] [CrossRef] [PubMed]
- Remington, J.S.; Cavanaugh, E.N. Isolation of the encysted form of Toxoplasma gondii from human skeletal muscle and brain. N. Engl. J. Med. 1965, 273, 1308–1310. [Google Scholar] [CrossRef]
- Rougier, S.; Montoya, J.G.; Peyron, F. Lifelong persistence of Toxoplasma cysts: A questionable dogma? Trends Parasitol. 2017, 33, 93–101. [Google Scholar] [CrossRef]
- Morisaki, J.H.; Heuser, J.E.; Sibley, L.D. Invasion of Toxoplasma gondii occurs by active penetration of the host cell. J. Cell. Sci. 1995, 108 Pt 6, 2457–2464. [Google Scholar]
- Blader, I.J.; Coleman, B.I.; Chen, C.-T.; Gubbels, M.-J. Lytic cycle of Toxoplasma gondii: 15 years Later. Annu. Rev. Microbiol. 2015, 69, 463–485. [Google Scholar] [CrossRef] [Green Version]
- Zenner, L.; Darcy, F.; Capron, A.; Cesbron-Delauw, M.-F. Toxoplasma gondii: Kinetics of the dissemination in the host tissues during the acute phase of infection of mice and rats. Exp. Parasitol. 1998, 90, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Harker, K.S.; Ueno, N.; Lodoen, M.B. Toxoplasma gondii dissemination: A parasite’s journey through the infected host. Parasite Immunol. 2015, 37, 141–149. [Google Scholar] [CrossRef]
- Sasai, M.; Yamamoto, M. Innate, adaptive, and cell-autonomous immunity against Toxoplasma gondii infection. Exp. Mol. Med. 2019, 51, 156. [Google Scholar] [CrossRef] [Green Version]
- Hakimi, M.-A.; Olias, P.; Sibley, L.D. Toxoplasma effectors targeting host signaling and transcription. Clin. Microbiol. Rev. 2017, 30, 615–645. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lima, T.S.; Lodoen, M.B. Mechanisms of human innate immune evasion by Toxoplasma gondii. Front. Cell. Infect. Microbiol. 2019, 9, 103. [Google Scholar] [CrossRef] [PubMed]
- Jeffers, V.; Tampaki, Z.; Kim, K.; Sullivan, W.J. A latent ability to persist: Differentiation in Toxoplasma gondii. Cell. Mol. Life Sci. 2018, 75, 2355–2373. [Google Scholar] [CrossRef] [PubMed]
- Tu, V.; Yakubu, R.; Weiss, L.M. Observations on bradyzoite biology. Microbes Infect. 2018, 20, 466–476. [Google Scholar] [CrossRef] [PubMed]
- Bohne, W.; Heesemann, J.; Gross, U. Reduced replication of Toxoplasma gondii is necessary for induction of bradyzoite-specific antigens: A possible role for nitric oxide in triggering stage conversion. Infect. Immun. 1994, 62, 1761–1767. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomavo, S.; Boothroyd, J.C. Interconnection between organellar functions, development and drug resistance in the protozoan parasite, Toxoplasma gondii. Int. J. Parasitol. 1995, 25, 1293–1299. [Google Scholar] [CrossRef]
- Fox, B.A.; Gigley, J.P.; Bzik, D.J. Toxoplasma gondii lacks the enzymes required for de novo arginine biosynthesis and arginine starvation triggers cyst formation. Int. J. Parasitol. 2004, 34, 323–331. [Google Scholar] [CrossRef]
- Boyle, J.P.; Saeij, J.P.J.; Cleary, M.D.; Boothroyd, J.C. Analysis of gene expression during development: Lessons from the Apicomplexa. Microbes Infect. 2006, 8, 1623–1630. [Google Scholar] [CrossRef]
- Bohne, W.; Heesemann, J.; Gross, U. Induction of bradyzoite-specific Toxoplasma gondii antigens in gamma interferon-treated mouse macrophages. Infect. Immun. 1993, 61, 1141–1145. [Google Scholar] [CrossRef] [Green Version]
- Soete, M.; Camus, D.; Dubremetz, J.F. Experimental induction of bradyzoite-specific antigen expression and cyst formation by the RH strain of Toxoplasma gondii in vitro. Exp. Parasitol. 1994, 78, 361–370. [Google Scholar] [CrossRef]
- Ihara, F.; Nishikawa, Y. Starvation of low-density lipoprotein-derived cholesterol induces bradyzoite conversion in Toxoplasma gondii. Parasit Vectors 2014, 7, 248. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bougdour, A.; Maubon, D.; Baldacci, P.; Ortet, P.; Bastien, O.; Bouillon, A.; Barale, J.-C.; Pelloux, H.; Ménard, R.; Hakimi, M.-A. Drug inhibition of HDAC3 and epigenetic control of differentiation in Apicomplexa parasites. J. Exp. Med. 2009, 206, 953–966. [Google Scholar] [CrossRef]
- Maubon, D.; Bougdour, A.; Wong, Y.-S.; Brenier-Pinchart, M.-P.; Curt, A.; Hakimi, M.-A.; Pelloux, H. Activity of the histone deacetylase inhibitor FR235222 on Toxoplasma gondii: Inhibition of stage conversion of the parasite cyst form and study of new derivative compounds. Antimicrob. Agents Chemother. 2010, 54, 4843–4850. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weiss, L.M.; Laplace, D.; Takvorian, P.M.; Tanowitz, H.B.; Cali, A.; Wittner, M. A cell culture system for study of the development of Toxoplasma gondii bradyzoites. J. Eukaryot. Microbiol. 1995, 42, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Bohne, W.; Roos, D.S. Stage-specific expression of a selectable marker in Toxoplasma gondii permits selective inhibition of either tachyzoites or bradyzoites. Mol. Biochem. Parasitol. 1997, 88, 115–126. [Google Scholar] [CrossRef]
- Gross, U.; Pohl, F. Influence of antimicrobial agents on replication and stage conversion of Toxoplasma gondii. Curr. Top. Microbiol. Immunol. 1996, 219, 235–245. [Google Scholar] [PubMed]
- Kirkman, L.A.; Weiss, L.M.; Kim, K. Cyclic nucleotide signaling in Toxoplasma gondii bradyzoite differentiation. Infect. Immun. 2001, 69, 148–153. [Google Scholar] [CrossRef] [Green Version]
- Radke, J.R.; Donald, R.G.; Eibs, A.; Jerome, M.E.; Behnke, M.S.; Liberator, P.; White, M.W. Changes in the expression of human cell division autoantigen-1 influence Toxoplasma gondii growth and development. PLoS Pathog. 2006, 2, e105. [Google Scholar] [CrossRef] [Green Version]
- Weiss, L.M.; Kim, K. The development and biology of bradyzoites of Toxoplasma gondii. Front. Biosci. 2000, 5, D391–D405. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, D.J.P. Use of molecular and ultrastructural markers to evaluate stage conversion of Toxoplasma gondii in both the intermediate and definitive host. Int. J. Parasitol. 2004, 34, 347–360. [Google Scholar] [CrossRef]
- Soete, M.; Fortier, B.; Camus, D.; Dubremetz, J.F. Toxoplasma gondii: Kinetics of bradyzoite-tachyzoite interconversion in vitro. Exp. Parasitol. 1993, 76, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Dzierszinski, F.; Nishi, M.; Ouko, L.; Roos, D.S. Dynamics of Toxoplasma gondii differentiation. Eukaryot. Cell 2004, 3, 992–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Watts, E.; Zhao, Y.; Dhara, A.; Eller, B.; Patwardhan, A.; Sinai, A.P. Novel Approaches Reveal that Toxoplasma gondii Bradyzoites within Tissue Cysts Are Dynamic and Replicating Entities In Vivo. MBio 2015, 6, e01155-15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sinai, A.P.; Watts, E.A.; Dhara, A.; Murphy, R.D.; Gentry, M.S.; Patwardhan, A. Reexamining chronic Toxoplasma gondii infection: Surprising activity for a “dormant” parasite. Curr. Clin. Microbiol. Rep. 2016, 3, 175–185. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, D.J.; Hutchison, W.M. An ultrastructural study of the early development and tissue cyst formation of Toxoplasma gondii in the brains of mice. Parasitol. Res. 1987, 73, 483–491. [Google Scholar] [CrossRef]
- Lemgruber, L.; Lupetti, P.; Martins-Duarte, E.S.; De Souza, W.; Vommaro, R.C. The organization of the wall filaments and characterization of the matrix structures of Toxoplasma gondii cyst form: Structure of Toxoplasma gondii cyst. Cell. Microbiol. 2011, 13, 1920–1932. [Google Scholar] [CrossRef]
- Tu, V.; Mayoral, J.; Sugi, T.; Tomita, T.; Han, B.; Ma, Y.F.; Weiss, L.M. Enrichment and Proteomic characterization of the cyst wall from in vitro Toxoplasma gondii cysts. mBio 2019, 10, e00469-19. [Google Scholar] [CrossRef] [Green Version]
- Tu, V.; Tomita, T.; Sugi, T.; Mayoral, J.; Han, B.; Yakubu, R.R.; Williams, T.; Horta, A.; Ma, Y.; Weiss, L.M. The Toxoplasma gondii cyst wall interactome. mBio 2020, 11, e02699-19. [Google Scholar] [CrossRef] [Green Version]
- Yang, S.; Parmley, S.F. Toxoplasma gondii expresses two distinct lactate dehydrogenase homologous genes during its life cycle in intermediate hosts. Gene 1997, 184, 1–12. [Google Scholar] [CrossRef]
- Dzierszinski, F.; Popescu, O.; Toursel, C.; Slomianny, C.; Yahiaoui, B.; Tomavo, S. The protozoan parasite Toxoplasma gondii expresses two functional plant-like glycolytic enzymes. Implications for evolutionary origin of apicomplexans. J. Biol. Chem. 1999, 274, 24888–24895. [Google Scholar] [CrossRef] [Green Version]
- Dzierszinski, F.; Mortuaire, M.; Dendouga, N.; Popescu, O.; Tomavo, S. Differential expression of two plant-like enolases with distinct enzymatic and antigenic properties during stage conversion of the protozoan parasite Toxoplasma gondii. J. Mol. Biol. 2001, 309, 1017–1027. [Google Scholar] [CrossRef] [PubMed]
- Tomavo, S. The differential expression of multiple isoenzyme forms during stage conversion of Toxoplasma gondii: An adaptive developmental strategy. Int. J. Parasitol. 2001, 31, 1023–1031. [Google Scholar] [CrossRef]
- Abdelbaset, A.E.; Fox, B.A.; Karram, M.H.; Abd Ellah, M.R.; Bzik, D.J.; Igarashi, M. Lactate dehydrogenase in Toxoplasma gondii controls virulence, bradyzoite differentiation, and chronic infection. PLoS ONE 2017, 12, e0173745. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Denton, H.; Roberts, C.W.; Alexander, J.; Thong, K.W.; Coombs, G.H. Enzymes of energy metabolism in the bradyzoites and tachyzoites of Toxoplasma gondii. FEMS Microbiol. Lett. 1996, 137, 103–108. [Google Scholar] [CrossRef]
- Shukla, A.; Olszewski, K.L.; Llinás, M.; Rommereim, L.M.; Fox, B.A.; Bzik, D.J.; Xia, D.; Wastling, J.; Beiting, D.; Roos, D.S.; et al. Glycolysis is important for optimal asexual growth and formation of mature tissue cysts by Toxoplasma gondii. Int. J. Parasitol. 2018, 48, 955–968. [Google Scholar] [CrossRef]
- Dubey, J.P.; Lindsay, D.S.; Speer, C.A. Structures of Toxoplasma gondii tachyzoites, bradyzoites, and sporozoites and biology and development of tissue cysts. Clin. Microbiol. Rev. 1998, 11, 267–299. [Google Scholar] [CrossRef] [Green Version]
- Uboldi, A.D.; McCoy, J.M.; Blume, M.; Gerlic, M.; Ferguson, D.J.P.; Dagley, L.F.; Beahan, C.T.; Stapleton, D.I.; Gooley, P.R.; Bacic, A.; et al. Regulation of starch stores by a Ca(2+)-dependent protein kinase is essential for viable cyst development in Toxoplasma gondii. Cell Host Microbe 2015, 18, 670–681. [Google Scholar] [CrossRef] [Green Version]
- Sugi, T.; Tu, V.; Ma, Y.; Tomita, T.; Weiss, L.M. Toxoplasma gondii requires glycogen phosphorylase for balancing amylopectin storage and for efficient production of brain cysts. mBio 2017, 8, e01289-17. [Google Scholar] [CrossRef] [Green Version]
- Buchholz, K.R.; Fritz, H.M.; Chen, X.; Durbin-Johnson, B.; Rocke, D.M.; Ferguson, D.J.; Conrad, P.A.; Boothroyd, J.C. Identification of tissue cyst wall components by transcriptome analysis of in vivo and in vitro Toxoplasma gondii bradyzoites. Eukaryot. Cell 2011, 10, 1637–1647. [Google Scholar] [CrossRef] [Green Version]
- Pittman, K.J.; Aliota, M.T.; Knoll, L.J. Dual transcriptional profiling of mice and Toxoplasma gondii during acute and chronic infection. BMC Genom. 2014, 15, 806. [Google Scholar] [CrossRef] [Green Version]
- Garfoot, A.L.; Wilson, G.M.; Coon, J.J.; Knoll, L.J. Proteomic and transcriptomic analyses of early and late-chronic Toxoplasma gondii infection shows novel and stage specific transcripts. BMC Genom. 2019, 20, 859. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, K. The Epigenome, cell cycle, and development in Toxoplasma. Annu. Rev. Microbiol. 2018, 72, 479–499. [Google Scholar] [CrossRef] [PubMed]
- Saksouk, N.; Bhatti, M.M.; Kieffer, S.; Smith, A.T.; Musset, K.; Garin, J.; Sullivan, W.J.; Cesbron-Delauw, M.-F.; Hakimi, M.-A. Histone-modifying complexes regulate gene expression pertinent to the differentiation of the protozoan parasite Toxoplasma gondii. Mol. Cell. Biol. 2005, 25, 10301–10314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Naguleswaran, A.; Elias, E.V.; McClintick, J.; Edenberg, H.J.; Sullivan, W.J. Toxoplasma gondii lysine acetyltransferase GCN5-A functions in the cellular response to alkaline stress and expression of cyst genes. PLoS Pathog. 2010, 6, e1001232. [Google Scholar] [CrossRef]
- Balaji, S.; Babu, M.M.; Iyer, L.M.; Aravind, L. Discovery of the principal specific transcription factors of Apicomplexa and their implication for the evolution of the AP2-integrase DNA binding domains. Nucleic Acids Res. 2005, 33, 3994–4006. [Google Scholar] [CrossRef] [Green Version]
- Radke, J.B.; Lucas, O.; De Silva, E.K.; Ma, Y.; Sullivan, W.J.; Weiss, L.M.; Llinas, M.; White, M.W. ApiAP2 transcription factor restricts development of the Toxoplasma tissue cyst. Proc. Natl. Acad. Sci. USA 2013, 110, 6871–6876. [Google Scholar] [CrossRef] [Green Version]
- Hong, D.-P.; Radke, J.B.; White, M.W. Opposing Transcriptional Mechanisms Regulate Toxoplasma Development. mSphere 2017, 2, e00347-16. [Google Scholar] [CrossRef] [Green Version]
- Huang, S.; Holmes, M.J.; Radke, J.B.; Hong, D.-P.; Liu, T.-K.; White, M.W.; Sullivan, W.J. Toxoplasma gondii AP2IX-4 regulates gene expression during bradyzoite development. mSphere 2017, 2, e00054-17. [Google Scholar] [CrossRef] [Green Version]
- Radke, J.B.; Worth, D.; Hong, D.; Huang, S.; Sullivan, W.J.; Wilson, E.H.; White, M.W. Transcriptional repression by ApiAP2 factors is central to chronic toxoplasmosis. PLoS Pathog. 2018, 14, e1007035. [Google Scholar] [CrossRef] [Green Version]
- Waldman, B.S.; Schwarz, D.; Wadsworth, M.H.; Saeij, J.P.; Shalek, A.K.; Lourido, S. Identification of a master regulator of differentiation in Toxoplasma. Cell 2020, 180, 359–372.e16. [Google Scholar] [CrossRef] [Green Version]
- Ferguson, D.J.; Hutchison, W.M.; Pettersen, E. Tissue cyst rupture in mice chronically infected with Toxoplasma gondii. An immunocytochemical and ultrastructural study. Parasitol. Res. 1989, 75, 599–603. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Orellana, M.A.; Schreiber, R.D.; Remington, J.S. Interferon-gamma: The major mediator of resistance against Toxoplasma gondii. Science 1988, 240, 516–518. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, Y.; Remington, J.S. The effect of anti-IFN-gamma antibody on the protective effect of Lyt-2+ immune T cells against toxoplasmosis in mice. J. Immunol. 1990, 144, 1954–1956. [Google Scholar] [PubMed]
- Gazzinelli, R.; Xu, Y.; Hieny, S.; Cheever, A.; Sher, A. Simultaneous depletion of CD4+ and CD8+ T lymphocytes is required to reactivate chronic infection with Toxoplasma gondii. J. Immunol. 1992, 149, 175–180. [Google Scholar]
- Dard, C.; Marty, P.; Brenier-Pinchart, M.-P.; Garnaud, C.; Fricker-Hidalgo, H.; Pelloux, H.; Pomares, C. Management of toxoplasmosis in transplant recipients: An update. Expert Rev. Anti-Infect. Ther. 2018, 16, 447–460. [Google Scholar] [CrossRef]
- Wang, Z.-D.; Wang, S.-C.; Liu, H.-H.; Ma, H.-Y.; Li, Z.-Y.; Wei, F.; Zhu, X.-Q.; Liu, Q. Prevalence and burden of Toxoplasma gondii infection in HIV-infected people: A systematic review and meta-analysis. Lancet HIV 2017, 4, e177–e188. [Google Scholar] [CrossRef]
- Frenkel, J.K.; Escajadillo, A. Cyst rupture as a pathogenic mechanism of toxoplasmic encephalitis. Am. J. Trop. Med. Hyg. 1987, 36, 517–522. [Google Scholar] [CrossRef]
- Salvioni, A.; Belloy, M.; Lebourg, A.; Bassot, E.; Cantaloube-Ferrieu, V.; Vasseur, V.; Blanié, S.; Liblau, R.S.; Suberbielle, E.; Robey, E.A.; et al. Robust control of a brain-persisting parasite through MHC I presentation by infected neurons. Cell Rep. 2019, 27, 3254–3268.e8. [Google Scholar] [CrossRef] [Green Version]
- Melzer, T.C.; Cranston, H.J.; Weiss, L.M.; Halonen, S.K. Host cell preference of Toxoplasma gondii cysts in murine brain: A confocal study. J. Neuroparasitol. 2010, 1, N100505. [Google Scholar] [CrossRef]
- Schaeffer, M.; Han, S.-J.; Chtanova, T.; van Dooren, G.G.; Herzmark, P.; Chen, Y.; Roysam, B.; Striepen, B.; Robey, E.A. Dynamic imaging of T Cell-parasite interactions in the brains of mice chronically infected with Toxoplasma gondii. J. Immunol. 2009, 182, 6379–6393. [Google Scholar] [CrossRef] [Green Version]
- John, B.; Ricart, B.; Tait Wojno, E.D.; Harris, T.H.; Randall, L.M.; Christian, D.A.; Gregg, B.; De Almeida, D.M.; Weninger, W.; Hammer, D.A.; et al. Analysis of behavior and trafficking of dendritic cells within the brain during toxoplasmic encephalitis. PLoS Pathog. 2011, 7, e1002246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krishnamurthy, S.; Saeij, J.P.J. Toxoplasma does not secrete the GRA16 and GRA24 effectors beyond the parasitophorous vacuole membrane of tissue cysts. Front. Cell Infect. Microbiol. 2018, 8, 366. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez, J.; Bittame, A.; Massera, C.; Vasseur, V.; Effantin, G.; Valat, A.; Buaillon, C.; Allart, S.; Fox, B.A.; Rommereim, L.M.; et al. Intravacuolar membranes regulate CD8 T cell recognition of membrane-bound Toxoplasma gondii protective antigen. Cell Rep. 2015, 13, 2273–2286. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwab, J.C.; Beckers, C.J.; Joiner, K.A. The parasitophorous vacuole membrane surrounding intracellular Toxoplasma gondii functions as a molecular sieve. Proc. Natl. Acad. Sci. USA 1994, 91, 509–513. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nance, J.P.; Vannella, K.M.; Worth, D.; David, C.; Carter, D.; Noor, S.; Hubeau, C.; Fitz, L.; Lane, T.E.; Wynn, T.A.; et al. Chitinase dependent control of protozoan cyst burden in the brain. PLoS Pathog. 2012, 8, e1002990. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hester, J.; Mullins, J.; Sa, Q.; Payne, L.; Mercier, C.; Cesbron-Delauw, M.-F.; Suzuki, Y. Toxoplasma gondii antigens recognized by IgG antibodies differ between mice with and without active proliferation of tachyzoites in the brain during the chronic stage of infection. Infect. Immun. 2012, 80, 3611–3620. [Google Scholar] [CrossRef] [Green Version]
- Miman, O.; Kusbeci, O.Y.; Aktepe, O.C.; Cetinkaya, Z. The probable relation between Toxoplasma gondii and Parkinson’s disease. Neurosci. Lett. 2010, 475, 129–131. [Google Scholar] [CrossRef]
- Torrey, E.F.; Bartko, J.J.; Yolken, R.H. Toxoplasma gondii and other risk factors for schizophrenia: An update. Schizophr. Bull. 2012, 38, 642–647. [Google Scholar] [CrossRef] [Green Version]
- Ngoungou, E.B.; Bhalla, D.; Nzoghe, A.; Dardé, M.-L.; Preux, P.-M. Toxoplasmosis and epilepsy—Systematic review and meta analysis. PLoS Negl. Trop. Dis. 2015, 9, e0003525. [Google Scholar] [CrossRef]
- Ngô, H.M.; Zhou, Y.; Lorenzi, H.; Wang, K.; Kim, T.-K.; Zhou, Y.; Bissati, K.E.; Mui, E.; Fraczek, L.; Rajagopala, S.V.; et al. Toxoplasma Modulates Signature Pathways of Human Epilepsy, Neurodegeneration & Cancer. Sci. Rep. 2017, 7, 11496. [Google Scholar]
- Ellen Tedford; Glenn McConkey Neurophysiological changes induced by chronic Toxoplasma gondii infection. Pathogens 2017, 6, 19. [CrossRef] [PubMed] [Green Version]
- Tyebji, S.; Seizova, S.; Hannan, A.J.; Tonkin, C.J. Toxoplasmosis: A pathway to neuropsychiatric disorders. Neurosci. Biobehav. Rev. 2019, 96, 72–92. [Google Scholar] [CrossRef]
- Araujo, F.G.; Huskinson-Mark, J.; Gutteridge, W.E.; Remington, J.S. In vitro and in vivo activities of the hydroxynaphthoquinone 566C80 against the cyst form of Toxoplasma gondii. Antimicrob. Agents Chemother. 1992, 36, 326–330. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferguson, D.J.; Huskinson-Mark, J.; Araujo, F.G.; Remington, J.S. An ultrastructural study of the effect of treatment with atovaquone in brains of mice chronically infected with the ME49 strain of Toxoplasma gondii. Int. J. Exp. Pathol. 1994, 75, 111–116. [Google Scholar] [PubMed]
- Gormley, P.D.; Pavesio, C.E.; Minnasian, D.; Lightman, S. Effects of drug therapy on Toxoplasma cysts in an animal model of acute and chronic disease. Investig. Ophthalmol. Vis. Sci. 1998, 39, 1171–1175. [Google Scholar]
- Rutaganira, F.U.; Barks, J.; Dhason, M.S.; Wang, Q.; Lopez, M.S.; Long, S.; Radke, J.B.; Jones, N.G.; Maddirala, A.R.; Janetka, J.W.; et al. Inhibition of calcium dependent protein kinase 1 (CDPK1) by pyrazolopyrimidine analogs decreases establishment and reoccurrence of central nervous system disease by Toxoplasma gondii. J. Med. Chem. 2017, 60, 9976–9989. [Google Scholar] [CrossRef]
- Pakos-Zebrucka, K.; Koryga, I.; Mnich, K.; Ljujic, M.; Samali, A.; Gorman, A.M. The integrated stress response. EMBO Rep. 2016, 17, 1374–1395. [Google Scholar] [CrossRef] [Green Version]
- Holmes, M.J.; da Silva Augusto, L.; Zhang, M.; Wek, R.C.; Sullivan, W.J. Translational control in the latency of apicomplexan parasites. Trends Parasitol. 2017, 33, 947–960. [Google Scholar] [CrossRef]
- Narasimhan, J.; Joyce, B.R.; Naguleswaran, A.; Smith, A.T.; Livingston, M.R.; Dixon, S.E.; Coppens, I.; Wek, R.C.; Sullivan, W.J. Translation regulation by eukaryotic initiation factor-2 kinases in the development of latent cysts in Toxoplasma gondii. J. Biol. Chem. 2008, 283, 16591–16601. [Google Scholar] [CrossRef] [Green Version]
- Konrad, C.; Queener, S.F.; Wek, R.C.; Sullivan, W.J. Inhibitors of eIF2α dephosphorylation slow replication and stabilize latency in Toxoplasma gondii. Antimicrob. Agents Chemother. 2013, 57, 1815–1822. [Google Scholar] [CrossRef] [Green Version]
- Benmerzouga, I.; Checkley, L.A.; Ferdig, M.T.; Arrizabalaga, G.; Wek, R.C.; Sullivan, W.J. Guanabenz repurposed as an antiparasitic with activity against acute and latent toxoplasmosis. Antimicrob. Agents Chemother. 2015, 59, 6939–6945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martynowicz, J.; Augusto, L.; Wek, R.C.; Boehm, S.L.; Sullivan, W.J. Guanabenz reverses a key behavioral change caused by latent toxoplasmosis in mice by reducing neuroinflammation. mBio 2019, 10, e00381-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guevara, R.B.; Fox, B.A.; Falla, A.; Bzik, D.J. Toxoplasma gondii intravacuolar-network-associated dense granule proteins regulate maturation of the cyst matrix and cyst wall. mSphere 2019, 4, e00487-19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Craver, M.P.J.; Rooney, P.J.; Knoll, L.J. Isolation of Toxoplasma gondii development mutants identifies a potential proteophosphogylcan that enhances cyst wall formation. Mol. Biochem. Parasitol. 2010, 169, 120–123. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomita, T.; Bzik, D.J.; Ma, Y.F.; Fox, B.A.; Markillie, L.M.; Taylor, R.C.; Kim, K.; Weiss, L.M. The Toxoplasma gondii cyst wall protein CST1 is critical for cyst wall integrity and promotes bradyzoite persistence. PLoS Pathog. 2013, 9, e1003823. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Acquarone, M.; Ferreira-da-Silva, M.d.F.; Guimarães, E.V.; Barbosa, H.S. Toxoplasma gondii tissue cyst: Cyst wall incorporation activity and matrix cytoskeleton proteins paving the way to nutrient acquisition. In Toxoplasmosis; Akyar, I., Ed.; InTech: London, UK, 2017; ISBN 978-953-51-3269-1. [Google Scholar]
- Caffaro, C.E.; Koshy, A.A.; Liu, L.; Zeiner, G.M.; Hirschberg, C.B.; Boothroyd, J.C. A nucleotide sugar transporter involved in glycosylation of the Toxoplasma tissue cyst wall is required for efficient persistence of bradyzoites. PLoS Pathog. 2013, 9, e1003331. [Google Scholar] [CrossRef] [Green Version]
- Tomita, T.; Sugi, T.; Yakubu, R.; Tu, V.; Ma, Y.; Weiss, L.M. Making home sweet and sturdy: Toxoplasma gondii ppGalNAc-Ts glycosylate in hierarchical order and confer cyst wall rigidity. mBio 2017, 8, e02048-16. [Google Scholar] [CrossRef] [Green Version]
- Radke, J.R.; Guerini, M.N.; Jerome, M.; White, M.W. A change in the premitotic period of the cell cycle is associated with bradyzoite differentiation in Toxoplasma gondii. Mol. Biochem. Parasitol. 2003, 131, 119–127. [Google Scholar] [CrossRef]
- Xue, Y.; Theisen, T.C.; Rastogi, S.; Ferrel, A.; Quake, S.R.; Boothroyd, J.C. A single-parasite transcriptional atlas of Toxoplasma gondii reveals novel control of antigen expression. Elife 2020, 9, e54129. [Google Scholar] [CrossRef] [Green Version]
- Paredes-Santos, T.C.; Martins-Duarte, E.S.; de Souza, W.; Attias, M.; Vommaro, R.C. Toxoplasma gondii reorganizes the host cell architecture during spontaneous cyst formation in vitro. Parasitology 2018, 145, 1027–1038. [Google Scholar] [CrossRef]
- Lüder, C.G.K.; Giraldo-Velásquez, M.; Sendtner, M.; Gross, U. Toxoplasma gondii in primary rat CNS cells: Differential contribution of neurons, astrocytes, and microglial cells for the intracerebral development and stage differentiation. Exp. Parasitol. 1999, 93, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-da-Silva, M.d.F.; Takács, A.C.; Barbosa, H.S.; Gross, U.; Lüder, C.G.K. Primary skeletal muscle cells trigger spontaneous Toxoplasma gondii tachyzoite-to-bradyzoite conversion at higher rates than fibroblasts. Int. J. Med. Microbiol. 2009, 299, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-da-Silva, M.d.F.; Rodrigues, R.M.; Andrade, E.F.d.; Carvalho, L.d.; Gross, U.; Lüder, C.G.K.; Barbosa, H.S. Spontaneous stage differentiation of mouse-virulent Toxoplasma gondii RH parasites in skeletal muscle cells: An ultrastructural evaluation. Mem. Inst. Oswaldo Cruz 2009, 104, 196–200. [Google Scholar] [CrossRef] [PubMed]
- Swierzy, I.J.; Lüder, C.G.K. Withdrawal of skeletal muscle cells from cell cycle progression triggers differentiation of Toxoplasma gondii towards the bradyzoite stage. Cell. Microbiol. 2015, 17, 2–17. [Google Scholar] [CrossRef] [PubMed]
- Weilhammer, D.R.; Iavarone, A.T.; Villegas, E.N.; Brooks, G.A.; Sinai, A.P.; Sha, W.C. Host metabolism regulates growth and differentiation of Toxoplasma gondii. Int. J. Parasitol. 2012, 42, 947–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blume, M.; Seeber, F. Metabolic interactions between Toxoplasma gondii and its host. F1000Research 2018, 7. [Google Scholar] [CrossRef] [Green Version]
- Nolan, S.J.; Romano, J.D.; Kline, J.T.; Coppens, I. Novel approaches to kill Toxoplasma gondii by exploiting the uncontrolled uptake of unsaturated fatty acids and vulnerability to lipid storage inhibition of the parasite. Antimicrob. Agents Chemother. 2018, 62, e00347-18. [Google Scholar] [CrossRef] [Green Version]
- Marino, N.D.; Boothroyd, J.C. Toxoplasma growth in vitro is dependent on exogenous tyrosine and is independent of AAH2 even in tyrosine-limiting conditions. Exp. Parasitol. 2017, 176, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Besteiro, S. Autophagy in apicomplexan parasites. Curr. Opin. Microbiol. 2017, 40, 14–20. [Google Scholar] [CrossRef]
- Di Cristina, M.; Dou, Z.; Lunghi, M.; Kannan, G.; Huynh, M.-H.; McGovern, O.L.; Schultz, T.L.; Schultz, A.J.; Miller, A.J.; Hayes, B.M.; et al. Toxoplasma depends on lysosomal consumption of autophagosomes for persistent infection. Nat. Microbiol. 2017, 2, 17096. [Google Scholar] [CrossRef] [Green Version]
- Kannan, G.; Di Cristina, M.; Schultz, A.J.; Huynh, M.-H.; Wang, F.; Schultz, T.L.; Lunghi, M.; Coppens, I.; Carruthers, V.B. Role of Toxoplasma gondii chloroquine resistance transporter in bradyzoite viability and digestive vacuole maintenance. mBio 2019, 10, e01324-19. [Google Scholar] [CrossRef] [Green Version]
- van Dooren, G.G.; Striepen, B. The algal past and parasite present of the apicoplast. Annu. Rev. Microbiol. 2013, 67, 271–289. [Google Scholar] [CrossRef]
- Frénal, K.; Jacot, D.; Hammoudi, P.-M.; Graindorge, A.; Maco, B.; Soldati-Favre, D. Myosin-dependent cell-cell communication controls synchronicity of division in acute and chronic stages of Toxoplasma gondii. Nat. Commun. 2017, 8, 15710. [Google Scholar] [CrossRef]
- Mayoral, J.; Di Cristina, M.; Carruthers, V.B.; Weiss, L.M. Toxoplasma gondii: Bradyzoite differentiation in vitro and in vivo. Methods Mol. Biol. 2020, 2071, 269–282. [Google Scholar]
- Fritz, H.M.; Buchholz, K.R.; Chen, X.; Durbin-Johnson, B.; Rocke, D.M.; Conrad, P.A.; Boothroyd, J.C. Transcriptomic analysis of toxoplasma development reveals many novel functions and structures specific to sporozoites and oocysts. PLoS ONE 2012, 7, e29998. [Google Scholar] [CrossRef]
- Halonen, S. Use of Human Neurons Derived via Cellular Reprogramming Methods to Study Host-Parasite Interactions of Toxoplasma gondii in Neurons. Cells 2017, 6, 32. [Google Scholar] [CrossRef]
- Swierzy, I.J.; Muhammad, M.; Kroll, J.; Abelmann, A.; Tenter, A.M.; Lüder, C.G.K. Toxoplasma gondii within skeletal muscle cells: A critical interplay for food-borne parasite transmission. Int. J. Parasitol. 2014, 44, 91–98. [Google Scholar] [CrossRef]
- Colinot, D.L.; Garbuz, T.; Bosland, M.C.; Wang, L.; Rice, S.E.; Sullivan, W.J.; Arrizabalaga, G.; Jerde, T.J. The common parasite Toxoplasma gondii induces prostatic inflammation and microglandular hyperplasia in a mouse model. Prostate 2017, 77, 1066–1075. [Google Scholar] [CrossRef]
- Guimarães, E.V.; de Carvalho, L.; Barbosa, H.S. Primary culture of skeletal muscle cells as a model for studies of Toxoplasma gondii cystogenesis. J. Parasitol. 2008, 94, 72–83. [Google Scholar] [CrossRef]
- Guimarães, E.V.; Carvalho, L.d.; Barbosa, H.S. Interaction and cystogenesis of Toxoplasma gondii within skeletal muscle cells in vitro. Mem. Inst. Oswaldo Cruz 2009, 104, 170–174. [Google Scholar] [CrossRef] [Green Version]
- Creuzet, C.; Robert, F.; Roisin, M.P.; Van Tan, H.; Benes, C.; Dupouy-Camet, J.; Fagard, R. Neurons in primary culture are less efficiently infected by Toxoplasma gondii than glial cells. Parasitol. Res. 1998, 84, 25–30. [Google Scholar] [CrossRef]
- Tanaka, N.; Ashour, D.; Dratz, E.; Halonen, S. Use of human induced pluripotent stem cell-derived neurons as a model for Cerebral Toxoplasmosis. Microbes Infect. 2016, 18, 496–504. [Google Scholar] [CrossRef]
- Passeri, E.; Jones-Brando, L.; Bordón, C.; Sengupta, S.; Wilson, A.M.; Primerano, A.; Rapoport, J.L.; Ishizuka, K.; Kano, S.-i.; Yolken, R.H.; et al. Infection and characterization of Toxoplasma gondii in human induced neurons from patients with brain disorders and healthy controls. Microbes Infect. 2016, 18, 153–158. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.-L.; Huang, S.-Y.; Behnke, M.S.; Chen, K.; Shen, B.; Zhu, X.-Q. The past, present, and future of genetic manipulation in Toxoplasma gondii. Trends Parasitol. 2016, 32, 542–553. [Google Scholar] [CrossRef]
- Pfefferkorn, E.R.; Kasper, L.H. Toxoplasma gondii: Genetic crosses reveal phenotypic suppression of hydroxyurea resistance by fluorodeoxyuridine resistance. Exp. Parasitol. 1983, 55, 207–218. [Google Scholar] [CrossRef]
- Donald, R.G.; Roos, D.S. Insertional mutagenesis and marker rescue in a protozoan parasite: Cloning of the uracil phosphoribosyltransferase locus from Toxoplasma gondii. Proc. Natl. Acad. Sci. USA 1995, 92, 5749–5753. [Google Scholar] [CrossRef] [Green Version]
- Knoll, L.J.; Boothroyd, J.C. Isolation of Developmentally Regulated Genes from Toxoplasma gondii by a Gene Trap with the Positive and Negative Selectable Marker Hypoxanthine-Xanthine-Guanine Phosphoribosyltransferase. Mol. Cell. Biol. 1998, 18, 807–814. [Google Scholar] [CrossRef] [Green Version]
- Farrell, A.; Coleman, B.I.; Benenati, B.; Brown, K.M.; Blader, I.J.; Marth, G.T.; Gubbels, M.-J. Whole genome profiling of spontaneous and chemically induced mutations in Toxoplasma gondii. BMC Genom. 2014, 15, 354. [Google Scholar] [CrossRef] [Green Version]
- Fox, B.A.; Ristuccia, J.G.; Gigley, J.P.; Bzik, D.J. Efficient gene replacements in Toxoplasma gondii strains deficient for nonhomologous end joining. Eukaryot. Cell 2009, 8, 520–529. [Google Scholar] [CrossRef] [Green Version]
- Huynh, M.-H.; Carruthers, V.B. Tagging of endogenous genes in a Toxoplasma gondii strain lacking Ku80. Eukaryot. Cell 2009, 8, 530–539. [Google Scholar] [CrossRef] [Green Version]
- Fox, B.A.; Falla, A.; Rommereim, L.M.; Tomita, T.; Gigley, J.P.; Mercier, C.; Cesbron-Delauw, M.F.; Weiss, L.M.; Bzik, D.J. Type II Toxoplasma gondii KU80 knockout strains enable functional analysis of genes required for Cyst development and latent infection. Eukaryot. Cell 2011, 10, 1193–1206. [Google Scholar] [CrossRef] [Green Version]
- Sidik, S.M.; Hackett, C.G.; Tran, F.; Westwood, N.J.; Lourido, S. Efficient genome engineering of Toxoplasma gondii using CRISPR/Cas9. PLoS ONE 2014, 9, e100450. [Google Scholar] [CrossRef] [Green Version]
- Shen, B.; Brown, K.M.; Lee, T.D.; David Sibley, L. Efficient gene disruption in diverse strains of toxoplasma gondii Using CRISPR/CAS9. mBio 2014, 5, e01114-14. [Google Scholar] [CrossRef] [Green Version]
- Singh, U.; Brewer, J.L.; Boothroyd, J.C. Genetic analysis of tachyzoite to bradyzoite differentiation mutants in Toxoplasma gondii reveals a hierarchy of gene induction. Mol. Microbiol. 2002, 44, 721–733. [Google Scholar] [CrossRef]
- Jinek, M.; Chylinski, K.; Fonfara, I.; Hauer, M.; Doudna, J.A.; Charpentier, E. A programmable dual-RNA-guided DNA endonuclease in adaptive bacterial immunity. Science 2012, 337, 816–821. [Google Scholar] [CrossRef]
- Sidik, S.M.; Huet, D.; Ganesan, S.M.; Huynh, M.-H.; Wang, T.; Nasamu, A.S.; Thiru, P.; Saeij, J.P.J.; Carruthers, V.B.; Niles, J.C.; et al. A Genome-wide CRISPR Screen in Toxoplasma Identifies Essential Apicomplexan Genes. Cell 2016, 166, 1423–1435. [Google Scholar] [CrossRef] [Green Version]
- Young, J.; Dominicus, C.; Wagener, J.; Butterworth, S.; Ye, X.; Kelly, G.; Ordan, M.; Saunders, B.; Instrell, R.; Howell, M.; et al. A CRISPR platform for targeted in vivo screens identifies Toxoplasma gondii virulence factors in mice. Nat. Commun. 2019, 10, 3963. [Google Scholar] [CrossRef] [Green Version]
- Andenmatten, N.; Egarter, S.; Jackson, A.J.; Jullien, N.; Herman, J.P.; Meissner, M. Conditional genome engineering in Toxoplasma gondii uncovers alternative invasion mechanisms. Nat. Methods 2013, 10, 125–127. [Google Scholar] [CrossRef] [Green Version]
- Meissner, M.; Brecht, S.; Bujard, H.; Soldati, D. Modulation of myosin A expression by a newly established tetracycline repressor-based inducible system in Toxoplasma gondii. Nucleic Acids Res. 2001, 29, E115. [Google Scholar] [CrossRef] [Green Version]
- Pieperhoff, M.S.; Pall, G.S.; Jiménez-Ruiz, E.; Das, S.; Melatti, C.; Gow, M.; Wong, E.H.; Heng, J.; Müller, S.; Blackman, M.J.; et al. Conditional U1 gene silencing in Toxoplasma gondii. PLoS ONE 2015, 10, e0130356. [Google Scholar] [CrossRef] [Green Version]
- Herm-Götz, A.; Agop-Nersesian, C.; Münter, S.; Grimley, J.S.; Wandless, T.J.; Frischknecht, F.; Meissner, M. Rapid control of protein level in the apicomplexan Toxoplasma gondii. Nat. Methods 2007, 4, 1003–1005. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.M.; Long, S.; Sibley, L.D. Plasma membrane association by N-acylation governs PKG function in Toxoplasma gondii. mBio 2017, 8, e00375-17. [Google Scholar] [CrossRef] [Green Version]
- Brown, K.; Long, S.; Sibley, L. Conditional Knockdown of Proteins Using Auxin-inducible Degron (AID) Fusions in Toxoplasma gondii. Bio-Protocol 2018, 8. [Google Scholar] [CrossRef] [Green Version]
- Pardridge, W.M. CNS drug design based on principles of blood-brain barrier transport. J. Neurochem. 1998, 70, 1781–1792. [Google Scholar] [CrossRef]
- Brown, K.M.; Sibley, L.D. Essential cGMP signaling in Toxoplasma is initiated by a hybrid P-type ATPase-guanylate cyclase. Cell Host Microbe 2018, 24, 804–816. [Google Scholar] [CrossRef] [Green Version]
- Lacroix, C.; Giovannini, D.; Combe, A.; Bargieri, D.Y.; Späth, S.; Panchal, D.; Tawk, L.; Thiberge, S.; Carvalho, T.G.; Barale, J.-C.; et al. FLP/FRT-mediated conditional mutagenesis in pre-erythrocytic stages of Plasmodium berghei. Nat. Protoc. 2011, 6, 1412–1428. [Google Scholar] [CrossRef]
- Hasin, Y.; Seldin, M.; Lusis, A. Multi-omics approaches to disease. Genome Biol. 2017, 18, 83. [Google Scholar] [CrossRef]
- Wang, Z.-X.; Zhou, C.-X.; Elsheikha, H.M.; He, S.; Zhou, D.-H.; Zhu, X.-Q. Proteomic differences between developmental stages of Toxoplasma gondii revealed by iTRAQ-based quantitative proteomics. Front. Microbiol. 2017, 8, 985. [Google Scholar] [CrossRef]
- Cleary, M.D.; Singh, U.; Blader, I.J.; Brewer, J.L.; Boothroyd, J.C. Toxoplasma gondii asexual development: Identification of developmentally regulated genes and distinct patterns of gene expression. Eukaryot. Cell 2002, 1, 329–340. [Google Scholar] [CrossRef] [Green Version]
- Krishnan, A.; Kloehn, J.; Lunghi, M.; Chiappino-Pepe, A.; Waldman, B.S.; Nicolas, D.; Varesio, E.; Hehl, A.; Lourido, S.; Hatzimanikatis, V.; et al. Functional and computational genomics reveal unprecedented flexibility in stage-specific Toxoplasma metabolism. Cell Host Microbe 2020, 27, 290–306.e11. [Google Scholar] [CrossRef]
- Hu, Y.; An, Q.; Sheu, K.; Trejo, B.; Fan, S.; Guo, Y. Single cell multi-omics technology: Methodology and application. Front. Cell Dev. Biol. 2018, 6, 28. [Google Scholar] [CrossRef] [Green Version]
- Di Cristina, M.; Marocco, D.; Galizi, R.; Proietti, C.; Spaccapelo, R.; Crisanti, A. Temporal and spatial distribution of Toxoplasma gondii differentiation into bradyzoites and tissue cyst formation in vivo. Infect. Immun. 2008, 76, 3491–3501. [Google Scholar] [CrossRef] [Green Version]
- Koshy, A.A.; Cabral, C.M. 3-D imaging and analysis of neurons infected in vivo with Toxoplasma gondii. JoVE 2014, 94, e52237. [Google Scholar]
- Cabral, C.M.; Tuladhar, S.; Dietrich, H.K.; Nguyen, E.; MacDonald, W.R.; Trivedi, T.; Devineni, A.; Koshy, A.A. Neurons are the primary target cell for the brain-tropic intracellular parasite Toxoplasma gondii. PLoS Pathog. 2016, 12, e1005447. [Google Scholar] [CrossRef]
- Wilson, E.H.; Harris, T.H.; Mrass, P.; John, B.; Tait, E.D.; Wu, G.F.; Pepper, M.; Wherry, E.J.; Dzierzinski, F.; Roos, D.; et al. Behavior of parasite-specific effector CD8+ T cells in the brain and visualization of a kinesis-associated system of reticular fibers. Immunity 2009, 30, 300–311. [Google Scholar] [CrossRef] [Green Version]
- Naemat, A.; Elsheikha, H.M.; Al-Sandaqchi, A.; Kong, K.; Ghita, A.; Notingher, I. Analysis of interaction between the apicomplexan protozoan Toxoplasma gondii and host cells using label-free Raman spectroscopy. Analyst 2015, 140, 756–764. [Google Scholar] [CrossRef]
- Tenter, A.M. Toxoplasma gondii in animals used for human consumption. Mem. Inst. Oswaldo Cruz 2009, 104, 364–369. [Google Scholar] [CrossRef] [Green Version]
- Innes, E.A.; Hamilton, C.; Garcia, J.L.; Chryssafidis, A.; Smith, D. A one health approach to vaccines against Toxoplasma gondii. Food Waterborne Parasitol. 2019, 15, e00053. [Google Scholar] [CrossRef]
- Vallette, F.M.; Olivier, C.; Lézot, F.; Oliver, L.; Cochonneau, D.; Lalier, L.; Cartron, P.-F.; Heymann, D. Dormant, quiescent, tolerant and persister cells: Four synonyms for the same target in cancer. Biochem. Pharmacol. 2019, 162, 169–176. [Google Scholar] [CrossRef] [Green Version]
- Fauvart, M.; De Groote, V.N.; Michiels, J. Role of persister cells in chronic infections: Clinical relevance and perspectives on anti-persister therapies. J. Med. Microbiol. 2011, 60, 699–709. [Google Scholar] [CrossRef]



| Stress Condition | Selected References |
|---|---|
| Alkaline pH (pH 8) | [21] |
| Heat shock (43 °C) | [21] |
| Nutrient deprivation | |
| Arginine starvation | [18] |
| Pyrimidine starvation | [26] |
| Cholesterol deprivation | [22] |
| Modulators of immunity and inflammation | |
| IFN-Υ | [20] |
| NO | [16] |
| IL-6 | [25] |
| LPS | [16] |
| Metabolic inhibitors | |
| Oligomycin, antimycin A | [16] |
| Myxothiazol, rotenone, atovaquone | [17] |
| Drugs and small compounds | |
| Compound 1 | [29] |
| Pyrimethamine | [16] |
| Sulfadiazine | [27] |
| Cyclic nucleotide signaling modulators | [28] |
| Apicidin, FR235222 (HDAC inhibitors) | [19,23,24] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cerutti, A.; Blanchard, N.; Besteiro, S. The Bradyzoite: A Key Developmental Stage for the Persistence and Pathogenesis of Toxoplasmosis. Pathogens 2020, 9, 234. https://doi.org/10.3390/pathogens9030234
Cerutti A, Blanchard N, Besteiro S. The Bradyzoite: A Key Developmental Stage for the Persistence and Pathogenesis of Toxoplasmosis. Pathogens. 2020; 9(3):234. https://doi.org/10.3390/pathogens9030234
Chicago/Turabian StyleCerutti, Aude, Nicolas Blanchard, and Sébastien Besteiro. 2020. "The Bradyzoite: A Key Developmental Stage for the Persistence and Pathogenesis of Toxoplasmosis" Pathogens 9, no. 3: 234. https://doi.org/10.3390/pathogens9030234