Accuracy of Mobile Applications versus Wearable Devices in Long-Term Step Measurements
Abstract
:1. Introduction
2. Materials and Methods
2.1. Phone-Based Applications and Wearable Fitness Trackers
- (APP1) Huawei Health, v10.0.2.333 (https://consumer.huawei.com);
- (APP2) Bits&Coffee ActivityTracker, v1.2.2.400070 (https://activitytrackerapp.com);
- (APP3) Best Simple Apps Contapassi, v4.1.5 ([email protected]);
- (APP4) GALA MIX WinWalk, v1.9.6 (http://winwalk.club);
- (APP5) LG Electronics LG Health, v5.40.16 (https://www.lg.com);
- (APP6) Pacer Health’s Pacer, vp6.10.1 (https://www.mypacer.com).
- (WFT1) Decathlon OnCoach 100, v1.1.6(39), price ~EUR 25 (https://www.decathlon.com);
- (WFT2) Crane activity tracker, v1.45, price ~EUR 50 (https://www.suunto.com);
- (WFT3) Suunto 9, v4.17.4, price ~EUR 500 (https://consumer.huawei.com).
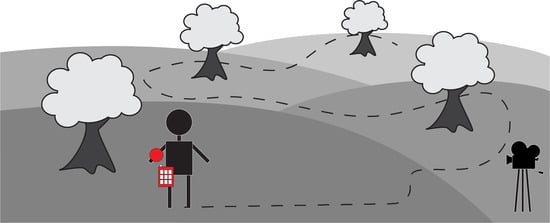
2.2. Tracker Accuracy: Experiment Description
2.3. Tracker Precision: Experiment Description
2.4. Statistics
3. Results
3.1. Tracker: Accuracy: Results
3.2. Tracker Precision: Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Ethics Statements
References
- Jee, H. Review of researches on smartphone applications for physical activity promotion in healthy adults. J. Exerc. Rehabil. 2017, 13, 3–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhao, S.; Li, S.; Ramos, J.; Luo, Z.; Jiang, Z.; Dey, A.K.; Pan, G. User profiling from their use of smartphone applications: A survey. Pervasive Mob. Comput. 2019, 59, 101052. [Google Scholar] [CrossRef]
- Kang, J.J.; Adibi, S. Systematic predictive analysis of personalized life expectancy using smart devices. Technologies 2018, 6, 74. [Google Scholar] [CrossRef] [Green Version]
- Bayo-Monton, J.L.; Martinez-Millana, A.; Han, W.; Fernandez-Llatas, C.; Sun, Y.; Traver, V. Wearable sensors integrated with Internet of Things for advancing eHealth care. Sensors 2018, 18, 1851. [Google Scholar] [CrossRef] [Green Version]
- Kranz, M.; MöLler, A.; Hammerla, N.; Diewald, S.; PlöTz, T.; Olivier, P.; Roalter, L. The mobile fitness coach: Towards individualized skill assessment using personalized mobile devices. Pervasive Mob. Comput. 2013, 9, 203–215. [Google Scholar] [CrossRef] [Green Version]
- Sadeghi, R.; Banerjee, T.; Hughes, J.C.; Lawhorne, L.W. Sleep quality prediction in caregivers using physiological signals. Comput. Biol. Med. 2019, 110, 276–288. [Google Scholar] [CrossRef]
- Purswani, J.M.; Dicker, A.P.; Champ, C.E.; Cantor, M.; Ohri, N. Big data from small devices: The future of smartphones in oncology. Semin. Radiat. Oncol. 2019, 29, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Dias, D.; Silva Cunha, J.P. Wearable health devices—Vital sign monitoring, systems and technologies. Sensors 2018, 18, 2414. [Google Scholar] [CrossRef] [Green Version]
- Heintzman, N.D. A digital ecosystem of diabetes data and technology: Services, systems, and tools enabled by wearables, sensors, and apps. J. Diabetes Sci. Technol. 2016, 10, 35–41. [Google Scholar] [CrossRef] [Green Version]
- Villarreal, V.; Nielsen, M.; Samudio, M. Sensing and storing the blood pressure measure by patients through a platform and mobile devices. Sensors 2018, 18, 1805. [Google Scholar] [CrossRef] [Green Version]
- Sazonov, E.; Lopez-Meyer, P.; Tiffany, S. A wearable sensor system for monitoring cigarette smoking. J. Stud. Alcohol Drugs 2013, 74, 956–964. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.W.; Han, D.C.; Shin, H.J.; Yeom, S.H.; Ju, B.K.; Lee, W. PEDOT: PSS-based temperature-detection thread for wearable devices. Sensors 2018, 18, 2996. [Google Scholar] [CrossRef] [Green Version]
- Kessel, K.A.; Vogel, M.M.; Kessel, C.; Bier, H.; Biedermann, T.; Friess, H.; Herschbach, P.; von Eisenhart-Rothe, R.; Meyer, B.; Kiechle, M.; et al. Mobile health in oncology: A patient survey about app-assisted cancer care. JMIR mHealth uHealth 2017, 5, e81. [Google Scholar] [CrossRef]
- Kang, X.; Huang, B.; Qi, G. A novel walking detection and step counting algorithm using unconstrained smartphones. Sensors 2018, 18, 297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rajan, K.; Garofalo, E.; Chiolerio, A. Wearable intrinsically soft, stretchable, flexible devices for memories and computing. Sensors 2018, 18, 367. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Masse, L.C.; Tilert, T.; McDowell, M. Physical activity in the United States measured by accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Mansukhani, M.P.; Kolla, B.P. Apps and fitness trackers that measure sleep: Are they useful. Clevel. Clin. J. Med. 2017, 84, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Kinney, D.A.; Nabors, L.A.; Merianos, A.L.; Vidourek, R.A. College students’ use and perceptions of wearable fitness trackers. Am. J. Health Educ. 2019, 50, 298–307. [Google Scholar] [CrossRef]
- Arigo, D.; Jake-Schoffman, D.E.; Wolin, K.; Beckjord, E.; Hekler, E.B.; Pagoto, S.L. The history and future of digital health in the field of behavioral medicine. J. Behav. Med. 2019, 42, 67–83. [Google Scholar] [CrossRef]
- Larsen, G. Treatment of obesity. Tidsskr. Nor. laegeforen. 1949, 69, 442–446. [Google Scholar]
- Schulmann, J.L.; Reisman, J.M. An objective measurement of hyperactivity. Am. J. Ment. Defic. 1959, 64, 455–456. [Google Scholar]
- Burgdorf, A.; Güthe, I.; Jovanović, M.; Kutafina, E.; Kohlschein, C.; Bitsch, J.Á.; Jonas, S.M. The mobile sleep lab app: An open-source framework for mobile sleep assessment based on consumer-grade wearable devices. Comput. Biol. Med. 2018, 103, 8–16. [Google Scholar] [CrossRef] [PubMed]
- Bassett, D.R.; Toth, L.P.; LaMunion, S.R.; Crouter, S.E. Step counting: A review of measurement considerations and health-related applications. Sports Med. 2017, 47, 1303–1315. [Google Scholar] [CrossRef] [Green Version]
- Purswani, J.M.; Ohri, N.; Champ, C. Tracking steps in oncology: The time is now. Cancer Manag. Res. 2018, 10, 2439. [Google Scholar] [CrossRef] [Green Version]
- El-Amrawy, F.; Nounou, M.I. Are currently available wearable devices for activity tracking and heart rate monitoring accurate, precise, and medically beneficial? Health Inform. Res. 2015, 21, 315–320. [Google Scholar] [CrossRef]
- Evenson, K.R.; Goto, M.M.; Furberg, R.D. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 159. [Google Scholar] [CrossRef] [Green Version]
- Peake, J.; Kerr, G.K.; Sullivan, J.P. A critical review of consumer wearables, mobile applications and equipment for providing biofeedback, monitoring stress and sleep in physically active populations. Front. Physiol. 2018, 9, 743. [Google Scholar] [CrossRef]
- Hershman, S.G.; Bot, B.M.; Shcherbina, A.; Doerr, M.; Moayedi, Y.; Pavlovic, A.; Waggott, D.; Cho, M.K.; Rosenberger, M.E.; Haskell, W.L.; et al. Physical activity, sleep and cardiovascular health data for 50,000 individuals from the MyHeart Counts Study. Sci. Data 2019, 6, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Cox, S.M.; Lane, A.; Volchenboum, S.L. Use of wearable, mobile, and sensor technology in cancer clinical trials. JCO Clin. Cancer Inform. 2018, 2, 1–11. [Google Scholar] [CrossRef]
- Gresham, G.; Schrack, J.; Gresham, L.M.; Shinde, A.M.; Hendifar, A.E.; Tuli, R.; Rimel, B.J.; Figlin, R.; Meinert, C.L.; Piantadosi, S. Wearable activity monitors in oncology trials: Current use of an emerging technology. Contemp. Clin. Trials 2018, 64, 13–21. [Google Scholar] [CrossRef] [Green Version]
- Chandwani, K.D.; Perkins, G.; Nagendra, H.R.; Raghuram, N.V.; Spelman, A.; Nagarathna, R.; Johnson, K.; Fortier, A.; Arun, B.; Wei, Q.; et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J. Clin. Oncol. 2014, 32, 1058. [Google Scholar] [CrossRef] [Green Version]
- Kitahara, C.M.; Platz, E.A.; Freeman, L.E.B.; Black, A.; Hsing, A.W.; Linet, M.S.; Park, Y.; Schairer, C.; De González, A.B. Physical activity, diabetes, and thyroid cancer risk: A pooled analysis of five prospective studies. Cancer Causes Control. 2012, 23, 463–471. [Google Scholar] [CrossRef] [Green Version]
- Leitzmann, M.F.; Brenner, A.; Moore, S.C.; Koebnick, C.; Park, Y.; Hollenbeck, A.; Schatzkin, A.; Ron, E. Prospective study of body mass index, physical activity and thyroid cancer. Int. J. Cancer 2010, 126, 2947–2956. [Google Scholar] [CrossRef] [Green Version]
- Rossing, M.A.; Remler, R.; Voigt, L.F.; Wicklund, K.G.; Daling, J.R. Recreational physical activity and risk of papillary thyroid cancer (United States). Cancer Causes Control. 2001, 12, 881–885. [Google Scholar] [CrossRef] [PubMed]
- Carbonaro, A.; Piccinini, F.; Reda, R. Integrating heterogeneous data of healthcare devices to enable domain data management. J. e-Learn. Knowl. Soc. 2018, 14, 1–12. [Google Scholar]
- Dijkhuis, T.B.; Blaauw, F.J.; Van Ittersum, M.W.; Velthuijsen, H.; Aiello, M. Personalized physical activity coaching: A machine learning approach. Sensors 2018, 18, 623. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tam, M.K.; Cheung, S.Y. Validation of consumer wearable activity tracker as step measurement in free-living conditions. Finn. J. eHealth eWelfare 2019, 11, 68–75. [Google Scholar] [CrossRef] [Green Version]
- Sears, T.; Alvalos, E.; Lawson, S.; McAlister, I.; Eschbach, L.C.; Bunn, J. Wrist-worn physical activity trackers tend to underestimate steps during walking. Int. J. Exerc. Sci. 2017, 10, 764–773. [Google Scholar]
- Takacs, J.; Pollock, C.L.; Guenther, J.R.; Bahar, M.; Napier, C.; Hunt, M.A. Validation of the Fitbit One activity monitor device during treadmill walking. J. Sci. Med. Sport 2014, 17, 496–500. [Google Scholar] [CrossRef]
- Huang, Y.; Xu, J.; Yu, B.; Shull, P.B. Validity of FitBit, Jawbone UP, Nike+ and other wearable devices for level and stair walking. Gait Posture 2016, 48, 36–41. [Google Scholar] [CrossRef]
- Ngueleu, A.M.; Blanchette, A.K.; Bouyer, L.; Maltais, D.; McFadyen, B.J.; Moffet, H.; Batcho, C.S. Design and accuracy of an instrumented insole using pressure sensors for step count. Sensors 2019, 19, 984. [Google Scholar] [CrossRef] [Green Version]
- Case, M.A.; Burwick, H.A.; Volpp, K.G.; Patel, M.S. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA 2015, 313, 625–626. [Google Scholar] [CrossRef] [Green Version]
- Modave, F.; Guo, Y.; Bian, J.; Gurka, M.J.; Parish, A.; Smith, M.D.; Lee, A.M.; Buford, T.W. Mobile device accuracy for step counting across age groups. JMIR mHealth uHealth 2017, 5, e88. [Google Scholar] [CrossRef]
- Bunn, J.A.; Jones, C.; Oliviera, A.; Webster, M.J. Assessment of step accuracy using the Consumer Technology Association standard. J. Sports Sci. 2019, 37, 244–248. [Google Scholar] [CrossRef]
- Soto-Perez-De-Celis, E.; Kim, H.; Rojo-Castillo, M.P.; Sun, C.L.; Chavarri-Guerra, Y.; Navarrete-Reyes, A.P.; Waisman, J.R.; Avila-Funes, J.A.; Aguayo, A.; Hurria, A. A pilot study of an accelerometer-equipped smartphone to monitor older adults with cancer receiving chemotherapy in Mexico. J. Geriatr. Oncol. 2018, 9, 145–151. [Google Scholar] [CrossRef]
- Jones, M.; Morris, J.; Deruyter, F. Mobile healthcare and people with disabilities: Current state and future needs. Int. J. Environ. Res. Public Health 2018, 15, 515. [Google Scholar] [CrossRef] [Green Version]
- Muzny, M.; Henriksen, A.; Giordanengo, A.; Muzik, J.; Grottland, A.; Blixgard, H.; Hartvigsen, G.; Arsand, E. Wearable sensors with possibilities for data exchange: Analyzing status and needs of different actors in mobile health monitoring systems. Int. J. Med. Inform. 2020, 133, 104017. [Google Scholar] [CrossRef] [PubMed]
- Díaz, S.; Stephenson, J.B.; Labrador, M.A. Use of wearable sensor technology in gait, balance, and range of motion analysis. Appl. Sci. 2020, 10, 234. [Google Scholar] [CrossRef] [Green Version]
- Hildebrand, M.; Van Hees, V.T.; Hansen, B.H.; Ekelund, U.L.F. Age group comparability of raw accelerometer output from wrist-and hip-worn monitors. Med. Sci. Sports Exerc. 2014, 46, 1816–1824. [Google Scholar] [CrossRef]
- Colley, R.; Gorber, S.C.; Tremblay, M.S. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 2010, 21, 63. [Google Scholar]


| Operator | Operator1 | Operator2 | Operator3 |
|---|---|---|---|
| GROUND TRUTH [steps] | 1027 | 1409 | 1175 |
| APP1 [steps] | 1036 | 1410 | 1176 |
| APP2 [steps] | 1036 | 1410 | 1176 |
| APP3 [steps] | 1036 | 1410 | 1176 |
| APP4 [steps] | 1036 | 1293 | 1095 |
| APP5 [steps] | 1036 | 1410 | 1176 |
| APP6 [steps] | 1036 | 1410 | 1176 |
| WFT1 [steps] | 1016 | 1380 | 1230 |
| WFT1 [steps] | 944 | 1424 | 1197 |
| WFT1 [steps] | 994 | 1402 | 1159 |
| APP1 (PAND) | 0.88 | 0.07 | 0.09 |
| APP2 (PAND) | 0.88 | 0.07 | 0.09 |
| APP3 (PAND) | 0.88 | 0.07 | 0.09 |
| APP4 (PAND) | 0.88 | 8.23 | 6.81 |
| APP5 (PAND) | 0.88 | 0.07 | 0.09 |
| APP6 (PAND) | 0.88 | 0.07 | 0.09 |
| WFT1 (PAND) | 1.07 | 2.06 | 4.68 |
| WFT1 (PAND) | 8.08 | 1.06 | 1.87 |
| WFT1 (PAND) | 3.21 | 0.50 | 1.36 |
| Day | APP1 | APP2 | APP3 | APP4 | APP5 | APP6 | WFT1 | WFT2 | WFT3 |
|---|---|---|---|---|---|---|---|---|---|
| 01 * | 6767 | 5000 | 6203 | 6100 | 6328 | 6140 | 7139 | 7216 | 7899 |
| 02 ** | 5507 | 5389 | 5070 | 5400 | 5310 | 4594 | 5907 | 6095 | 6631 |
| 03 *** | 5015 | 5015 | 4760 | 5000 | 5082 | 5015 | 6114 | 6387 | 7326 |
| 04 | 16,234 | 16,150 | 15,469 | 16,100 | 15,951 | 16,150 | 15,082 | 20,687 | 18,774 |
| 05 *** | 5363 | 5286 | 4823 | 4900 | 5233 | 5286 | 6596 | 9336 | 8853 |
| 06 *** | 1188 | 1188 | 1004 | 1200 | 792 | 1188 | 4011 | 6405 | 5018 |
| 07 *** | 5296 | 5255 | 4319 | 5300 | 5255 | 5255 | 7110 | 8817 | 8102 |
| 08 ** | 1793 | 1793 | 1589 | 1700 | 1793 | 1733 | 2759 | 3991 | 5452 |
| 09 | 13,997 | 629 | 13,699 | 629 | 629 | 629 | 10,112 | 13,966 | 14,618 |
| 10 * | 11,305 | 3662 | 11,047 | 2000 | 3663 | 3674 | 12,090 | 14,023 | 13,480 |
| 11 ** | 5568 | 4337 | 4651 | 2600 | 4169 | 5443 | 8661 | 7564 | 6381 |
| 12 | 8846 | 2396 | 8426 | 3800 | 8708 | 8738 | 8835 | 10,962 | 10,372 |
| 13 *** | 6299 | 6199 | 5959 | 4800 | 6101 | 6059 | 9633 | 8314 | 9241 |
| 14 ** | 9158 | 8931 | 7976 | 8000 | 8488 | 9621 | 10,356 | 11,972 | 11,192 |
| 15 ** | 4966 | 2764 | 4508 | 3400 | 3383 | 3591 | 5848 | 6504 | 6120 |
| 16 ** | 10,179 | 10,493 | 9640 | 10,000 | 10,493 | 10,103 | 11,770 | 17,065 | 15,826 |
| 17 *** | 6926 | 6926 | 6046 | 6200 | 6924 | 6926 | 9917 | 10,366 | 10,291 |
| 18 *** | 2777 | 2788 | 2631 | 2600 | 2604 | 2788 | 5159 | 5013 | 5893 |
| 19 *** | 3948 | 3948 | 3846 | 4100 | 3907 | 3948 | 6666 | 5785 | 6068 |
| 20 | 6050 | 6154 | 9211 | 6900 | 6154 | 6048 | 8000 | 8831 | 8543 |
| 21 * | 7798 | 7798 | 6052 | 5000 | 7652 | 7798 | 9306 | 8831 | 9062 |
| 22 *** | 4036 | 3988 | 4858 | 4400 | 3988 | 3988 | 6354 | 5841 | 7265 |
| 23 * | 6403 | 6403 | 6429 | 4200 | 6403 | 6403 | 7613 | 8051 | 7811 |
| 24 *** | 1306 | 1306 | 1155 | 2100 | 1306 | 1306 | 3105 | 2880 | 3466 |
| 25 *** | 2891 | 2862 | 2840 | 2700 | 2772 | 2862 | 4858 | 4592 | 5199 |
| 26 ** | 4741 | 4413 | 4259 | 5800 | 4399 | 4393 | 7262 | 6573 | 5391 |
| 27 * | 3800 | 3800 | 3615 | 4000 | 3800 | 3800 | 5618 | 4752 | 4107 |
| 28 | 12,487 | 12,410 | 12,414 | 14,000 | 12,410 | 12,410 | 11,813 | 16,608 | 16,767 |
| 29 | 6442 | 6395 | 6107 | 6500 | 6252 | 6309 | 5275 | 9551 | 8598 |
| 30 ** | 5220 | 4987 | 4818 | 3800 | 4987 | 4987 | 6131 | 6130 | 7361 |
| 31 * | 5505 | 5373 | 5154 | 9600 | 5370 | 5373 | 9108 | 8936 | 8252 |
| 32 *** | 3067 | 3059 | 2740 | 2600 | 3057 | 2991 | 6646 | 5655 | 6898 |
| 33 *** | 6972 | 7189 | 6748 | 8900 | 7187 | 6817 | 10,567 | 10,244 | 10,292 |
| 34 | 4645 | 4428 | 4015 | 6500 | 4428 | 4428 | 4838 | 5860 | 6421 |
| 35 *** | 3188 | 3023 | 2967 | 3800 | 2964 | 3023 | 6174 | 7824 | 8364 |
| 36 *** | 4045 | 3921 | 3565 | 4600 | 3921 | 3921 | 9744 | 10,198 | 9900 |
| 37 ** | 11,294 | 11,035 | 10,648 | 9400 | 11,035 | 11,035 | 13,264 | 19,936 | 19,899 |
| 38 *** | 6323 | 6187 | 5705 | 6000 | 6041 | 6187 | 8226 | 8135 | 8289 |
| 39 *** | 3919 | 3697 | 3278 | 3500 | 3563 | 3697 | 6939 | 5700 | 5900 |
| 40 * | 6113 | 5809 | 5296 | 4900 | 5809 | 5809 | 7062 | 6118 | 7123 |
| 41 ** | 6765 | 6574 | 6232 | 8900 | 6574 | 6574 | 9763 | 9020 | 9004 |
| 42 *** | 8707 | 8617 | 8305 | 9000 | 8587 | 8617 | 10,972 | 12,499 | 13,511 |
| 43 *** | 5132 | 5129 | 5142 | 4700 | 5129 | 5129 | 7411 | 10,038 | 10,260 |
| 44 * | 7439 | 7487 | 7252 | 8200 | 7311 | 7436 | 7536 | 11,673 | 12,831 |
| 45 | 11,226 | 11,226 | 10,800 | 7600 | 11,226 | 11,226 | 11,935 | 12,368 | 12,228 |
| 46 *** | 4729 | 4731 | 4458 | 4200 | 4580 | 4729 | 6836 | 7442 | 8118 |
| 47 | 17,699 | 17,699 | 17,271 | 10,900 | 17,560 | 17,699 | 17,440 | 20,016 | 18,621 |
| 48 * | 6055 | 6055 | 5863 | 6700 | 5851 | 6055 | 6396 | 6533 | 7151 |
| 49 ** | 13,563 | 13,188 | 13,309 | 11,200 | 13,188 | 13,188 | 13,889 | 17,786 | 18,717 |
| 50 | 7744 | 7744 | 7600 | 12,100 | 7606 | 7606 | 10,101 | 8938 | 10,198 |
| 51 *** | 2473 | 2473 | 2400 | 2400 | 2407 | 2407 | 5109 | 4265 | 4340 |
| 52 *** | 4694 | 4694 | 4631 | 3900 | 4498 | 4694 | 7346 | 6078 | 6859 |
| 53 *** | 5578 | 5408 | 5456 | 5400 | 5385 | 5577 | 7974 | 7373 | 9056 |
| 54 *** | 4435 | 4363 | 3986 | 3200 | 4363 | 4363 | 6572 | 6236 | 6530 |
| 55 * | 3257 | 3228 | 2992 | 3700 | 3228 | 3228 | 4890 | 9674 | 5193 |
| 56 ** | 4279 | 4249 | 4120 | 4900 | 4246 | 4249 | 7162 | 11,407 | 7133 |
| 57 *** | 6719 | 6553 | 6468 | 4600 | 6553 | 6553 | 9663 | 10,120 | 11,205 |
| 58 | 4304 | 3981 | 3807 | 3700 | 3917 | 3981 | 5891 | 6018 | 7882 |
| 59 ** | 7811 | 7651 | 7370 | 9700 | 7651 | 7532 | 9423 | 10,990 | 11,043 |
| 60 *** | 10,967 | 10,967 | 10,752 | 11,000 | 10,967 | 10,967 | 14,003 | 14,171 | 14,559 |
| Block | APP1 | APP2 | APP3 | APP4 | APP5 | APP6 | WFT1 | WFT2 | WFT3 |
|---|---|---|---|---|---|---|---|---|---|
| I ** | 72,465 | 49,367 | 67,983 | 48,329 | 50,036 | 49,664 | 76,920 | 96,923 | 96,153 |
| II *** | 64,717 | 54,936 | 62,894 | 52,400 | 60,931 | 63,265 | 84,845 | 92,376 | 89,927 |
| III *** | 55,124 | 54,362 | 52,547 | 52,500 | 53,969 | 54,256 | 67,335 | 73,809 | 75,027 |
| IV *** | 55,071 | 53,721 | 50,116 | 59,800 | 53,375 | 53,281 | 82,568 | 88,606 | 91,338 |
| V *** | 89,059 | 88,450 | 86,232 | 83,500 | 87,612 | 88,259 | 10,2279 | 11,6313 | 12,0639 |
| VI *** | 54,517 | 53,567 | 51,982 | 52,500 | 53,215 | 53,551 | 78,033 | 86,332 | 83,800 |
| DAY | APP1 | APP2 | APP3 | APP4 | APP5 | APP6 | WFT1 | WFT2 | WFT3 |
|---|---|---|---|---|---|---|---|---|---|
| 01 | 11 | −18 | 2 | 0 | 4 | 1 | −4 | −3 | 6 |
| 02 | 6 | 3 | −3 | 4 | 2 | −12 | −5 | −2 | 7 |
| 03 | 1 | 1 | −4 | 0 | 2 | 1 | −7 | −3 | 11 |
| 04 | 1 | 1 | −3 | 1 | 0 | 1 | −17 | 14 | 3 |
| 05 | 4 | 3 | −6 | −5 | 2 | 3 | −20 | 13 | 7 |
| 06 | 9 | 9 | −8 | 10 | −28 | 9 | −22 | 24 | −2 |
| 07 | 4 | 3 | −16 | 4 | 3 | 3 | −11 | 10 | 1 |
| 08 | 3 | 3 | −8 | −2 | 3 | 0 | −32 | −2 | 34 |
| 09 | 178 | −88 | 172 | −88 | −88 | −88 | −22 | 8 | 13 |
| 10 | 92 | −38 | 87 | −66 | −38 | −38 | −8 | 6 | 2 |
| 11 | 25 | −3 | 4 | −42 | −7 | 22 | 15 | 0 | −15 |
| 12 | 30 | −65 | 24 | −44 | 28 | 28 | −12 | 9 | 3 |
| 13 | 7 | 5 | 1 | −19 | 3 | 3 | 6 | −8 | 2 |
| 14 | 5 | 3 | −8 | −8 | −2 | 11 | −7 | 7 | 0 |
| 15 | 32 | −27 | 20 | −10 | −10 | −5 | −5 | 6 | −1 |
| 16 | 0 | 3 | −5 | −1 | 3 | 0 | −21 | 15 | 6 |
| 17 | 4 | 4 | −9 | −7 | 4 | 4 | −3 | 2 | 1 |
| 18 | 3 | 3 | −2 | −4 | −3 | 3 | −4 | −6 | 10 |
| 19 | 0 | 0 | −3 | 4 | −1 | 0 | 8 | −6 | −2 |
| 20 | −10 | −9 | 36 | 2 | −9 | −10 | −5 | 4 | 1 |
| 21 | 11 | 11 | −14 | −29 | 9 | 11 | 3 | −3 | 0 |
| 22 | −4 | −5 | 15 | 5 | −5 | −5 | −2 | −10 | 12 |
| 23 | 6 | 6 | 6 | −30 | 6 | 6 | −3 | 3 | 0 |
| 24 | −8 | −8 | −18 | 49 | −8 | −8 | −1 | −9 | 10 |
| 25 | 2 | 1 | 1 | −4 | −2 | 1 | −1 | −6 | 6 |
| 26 | 2 | −5 | −9 | 24 | −6 | −6 | 13 | 3 | −16 |
| 27 | 0 | 0 | −5 | 5 | 0 | 0 | 16 | −2 | −15 |
| 28 | −2 | −2 | −2 | 10 | −2 | −2 | −22 | 10 | 11 |
| 29 | 2 | 1 | −4 | 3 | −1 | 0 | −32 | 22 | 10 |
| 30 | 9 | 4 | 0 | −21 | 4 | 4 | −6 | −6 | 13 |
| 31 | −9 | −11 | −15 | 58 | −11 | −11 | 4 | 2 | −6 |
| 32 | 5 | 5 | −6 | −11 | 5 | 2 | 4 | −12 | 8 |
| 33 | −5 | −2 | −8 | 22 | −2 | −7 | 2 | −1 | −1 |
| 34 | −2 | −7 | −15 | 37 | −7 | −7 | −15 | 3 | 13 |
| 35 | 1 | −4 | −6 | 20 | −6 | −4 | −17 | 5 | 12 |
| 36 | 1 | −2 | −11 | 15 | −2 | −2 | −2 | 3 | 0 |
| 37 | 5 | 3 | −1 | −12 | 3 | 3 | −25 | 13 | 12 |
| 38 | 4 | 2 | −6 | −1 | −1 | 2 | 0 | −1 | 1 |
| 39 | 9 | 2 | −9 | −3 | −1 | 2 | 12 | −8 | −5 |
| 40 | 9 | 3 | −6 | −13 | 3 | 3 | 4 | −10 | 5 |
| 41 | −2 | −5 | −10 | 28 | −5 | −5 | 5 | −3 | −3 |
| 42 | 1 | 0 | −4 | 4 | −1 | 0 | −11 | 1 | 10 |
| 43 | 1 | 1 | 2 | −7 | 1 | 1 | −20 | 9 | 11 |
| 44 | −1 | 0 | −4 | 9 | −3 | −1 | −29 | 9 | 20 |
| 45 | 6 | 6 | 2 | −28 | 6 | 6 | −2 | 2 | 0 |
| 46 | 3 | 3 | −2 | −8 | 0 | 3 | −8 | 0 | 9 |
| 47 | 7 | 7 | 5 | −34 | 7 | 7 | −7 | 7 | 0 |
| 48 | −1 | −1 | −4 | 10 | −4 | −1 | −4 | −2 | 7 |
| 49 | 5 | 2 | 3 | −13 | 2 | 2 | −17 | 6 | 11 |
| 50 | −8 | −8 | −10 | 44 | −9 | −9 | 4 | −8 | 5 |
| 51 | 2 | 2 | −1 | −1 | −1 | −1 | 12 | −7 | −5 |
| 52 | 4 | 4 | 2 | −14 | 0 | 4 | 9 | −10 | 1 |
| 53 | 2 | −1 | 0 | −1 | −2 | 2 | −2 | −9 | 11 |
| 54 | 8 | 6 | −3 | −22 | 6 | 6 | 2 | −3 | 1 |
| 55 | 0 | −1 | −9 | 13 | −1 | −1 | −26 | 47 | −21 |
| 56 | −1 | −2 | −5 | 13 | −2 | −2 | −16 | 33 | −17 |
| 57 | 8 | 5 | 4 | −26 | 5 | 5 | −6 | −2 | 8 |
| 58 | 9 | 1 | −4 | −6 | −1 | 1 | −11 | −9 | 19 |
| 59 | −2 | −4 | −7 | 22 | −4 | −5 | −10 | 5 | 5 |
| 60 | 0 | 0 | −2 | 1 | 0 | 0 | −2 | −1 | 2 |
| AVERAGE | 8 | −3 | 2 | −3 | −3 | −1 | −6 | 2 | 4 |
| Block | APP1 | APP2 | APP3 | APP4 | APP5 | APP6 | WFT1 | WFT2 | WFT3 |
|---|---|---|---|---|---|---|---|---|---|
| I | 29 | −12 | 21 | −14 | −11 | −12 | −15 | 8 | 7 |
| II | 8 | −8 | 5 | −12 | 2 | 6 | −5 | 4 | 1 |
| III | 2 | 1 | −2 | −2 | 0 | 1 | −7 | 2 | 4 |
| IV | 2 | −1 | −8 | 10 | −2 | −2 | −6 | 1 | 4 |
| V | 2 | 1 | −1 | −4 | 0 | 1 | −10 | 3 | 7 |
| VI | 2 | 1 | −2 | −1 | 0 | 1 | −6 | 4 | 1 |
| AVERAGE | 8 | −3 | 2 | −4 | −2 | −1 | −8 | 4 | 4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piccinini, F.; Martinelli, G.; Carbonaro, A. Accuracy of Mobile Applications versus Wearable Devices in Long-Term Step Measurements. Sensors 2020, 20, 6293. https://doi.org/10.3390/s20216293
Piccinini F, Martinelli G, Carbonaro A. Accuracy of Mobile Applications versus Wearable Devices in Long-Term Step Measurements. Sensors. 2020; 20(21):6293. https://doi.org/10.3390/s20216293
Chicago/Turabian StylePiccinini, Filippo, Giovanni Martinelli, and Antonella Carbonaro. 2020. "Accuracy of Mobile Applications versus Wearable Devices in Long-Term Step Measurements" Sensors 20, no. 21: 6293. https://doi.org/10.3390/s20216293