Advances in Laser Ablation Synthesized Silicon-Based Nanomaterials for the Prevention of Bacterial Infection
Abstract
:1. Introduction
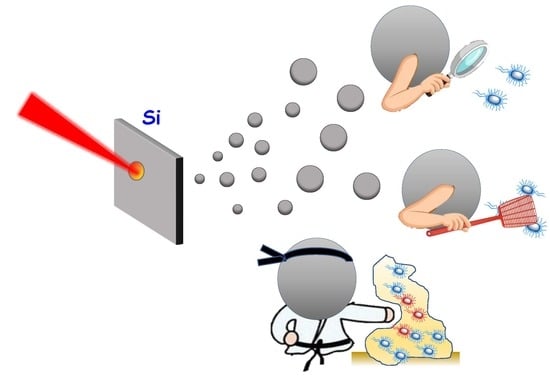
2. Methodologies and Parameters that Affect the Production of Silicon-Based Nanomaterials
2.1. Effects of the Ablation Method and the Ambient Media
2.2. Effects of Laser Processing Parameters
3. Antibacterial Effect of Silicon-Based Nanomaterials
4. Application of Silicon-Based Nanomaterials Synthesized by Laser Ablation for Combating Bacterial Infection
4.1. Silicon-Based Nanomaterials Synthesized by Laser Ablation for Preventing Bacterial Infection
4.2. Silicon-Based Nanomaterials Synthesized by Laser Ablation for Bacterial Detection
5. Conclusions and Future Perspectives
Funding
Acknowledgments
Conflicts of Interest
References
- Patel, K.D.; Singh, R.K.; Kim, H.-W. Carbon-based nanomaterials as an emerging platform for theranostics. Mater. Horiz. 2019, 6, 434–469. [Google Scholar] [CrossRef]
- Jeelani, P.G.; Mulay, P.; Venkat, R.; Ramalingam, C. Multifaceted Application of Silica Nanoparticles. A Review. Silicon 2020, 12, 1337–1354. [Google Scholar] [CrossRef]
- Nayfeh, M.H.; Mitas, L. Chapter One-Silicon Nanoparticles: New Photonic and Electronic Material at the Transition between Solid and Molecule; Kumar, V.B.T.-N., Ed.; Elsevier: Amsterdam, The Netherlands, 2008; pp. 1–78. ISBN 978-0-08-044528-1. [Google Scholar]
- Gribov, B.G.; Zinov’ev, K.V.; Kalashnik, O.N.; Gerasimenko, N.N.; Smirnov, D.I.; Sukhanov, V.N.; Kononov, N.N.; Dorofeev, S.G. Production of Silicon Nanoparticles for Use in Solar Cells. Semiconductors 2017, 51, 1675–1680. [Google Scholar] [CrossRef]
- Bouchoucha, M.; Béliveau, É.; Kleitz, F.; Calon, F.; Fortin, M.-A. Antibody-conjugated mesoporous silica nanoparticles for brain microvessel endothelial cell targeting. J. Mater. Chem. B 2017, 5, 7721–7735. [Google Scholar] [CrossRef]
- McInnes, S.J.P.; Turner, C.T.; Al-Bataineh, S.A.; Airaghi Leccardi, M.J.I.; Irani, Y.; Williams, K.A.; Cowin, A.J.; Voelcker, N.H. Surface engineering of porous silicon to optimise therapeutic antibody loading and release. J. Mater. Chem. B 2015, 3, 4123–4133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sheykhzadeh, S.; Luo, M.; Peng, B.; White, J.; Abdalla, Y.; Tang, T.; Mäkilä, E.; Voelcker, N.H.; Tong, W.Y. Transferrin-targeted porous silicon nanoparticles reduce glioblastoma cell migration across tight extracellular space. Sci. Rep. 2020, 10, 2320. [Google Scholar] [CrossRef] [Green Version]
- Martinez-Carmona, M.; Baeza, A.; Rodriguez-Milla, M.A.; Garcia-Castro, J.; Vallet-Regi, M. Mesoporous silica nanoparticles grafted with a light-responsive protein shell for highly cytotoxic antitumoral therapy. J. Mater. Chem. B 2015, 3, 5746–5752. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- López, V.; Villegas, M.R.; Rodríguez, V.; Villaverde, G.; Lozano, D.; Baeza, A.; Vallet-Regí, M. Janus Mesoporous Silica Nanoparticles for Dual Targeting of Tumor Cells and Mitochondria. ACS Appl. Mater. Interfaces 2017, 9, 26697–26706. [Google Scholar] [CrossRef]
- Jafari, S.; Derakhshankhah, H.; Alaei, L.; Fattahi, A.; Varnamkhasti, B.S.; Saboury, A.A. Mesoporous silica nanoparticles for therapeutic/diagnostic applications. Biomed. Pharmacother. 2019, 109, 1100–1111. [Google Scholar] [CrossRef]
- Moulari, B.; Pertuit, D.; Pellequer, Y.; Lamprecht, A. The targeting of surface modified silica nanoparticles to inflamed tissue in experimental colitis. Biomaterials 2008, 29, 4554–4560. [Google Scholar] [CrossRef]
- Kharlamov, A.N.; Tyurnina, A.E.; Veselova, V.S.; Kovtun, O.P.; Shur, V.Y.; Gabinsky, J.L. Silica-gold nanoparticles for atheroprotective management of plaques: Results of the NANOM-FIM trial. Nanoscale 2015, 7, 8003–8015. [Google Scholar] [CrossRef] [PubMed]
- Zilony-Hanin, N.; Rosenberg, M.; Richman, M.; Yehuda, R.; Schori, H.; Motiei, M.; Rahimipour, S.; Groisman, A.; Segal, E.; Shefi, O. Neuroprotective Effect of Nerve Growth Factor Loaded in Porous Silicon Nanostructures in an Alzheimer’s Disease Model and Potential Delivery to the Brain. Small 2019, 15, 1904203. [Google Scholar] [CrossRef] [PubMed]
- Jung, H.; Chung, Y.J.; Wilton, R.; Lee, C.H.; Lee, B.I.; Lim, J.; Lee, H.; Choi, J.-H.; Kang, H.; Lee, B.; et al. Silica Nanodepletors: Targeting and Clearing Alzheimer’s β-Amyloid Plaques. Adv. Funct. Mater. 2020, 30, 1910475. [Google Scholar] [CrossRef]
- Kim, B.; Pang, H.-B.; Kang, J.; Park, J.-H.; Ruoslahti, E.; Sailor, M.J. Immunogene therapy with fusogenic nanoparticles modulates macrophage response to Staphylococcus aureus. Nat. Commun. 2018, 9, 1969. [Google Scholar] [CrossRef]
- Iturrioz-Rodríguez, N.; Correa-Duarte, M.A.; Fanarraga, M.L. Controlled drug delivery systems for cancer based on mesoporous silica nanoparticles. Int. J. Nanomed. 2019, 14, 3389–3401. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Gun’ko, Y.; Vallet-Regí, M. Mesoporous Silica Materials as Drug Delivery: “The Nightmare” of Bacterial Infection. Pharmaceutics 2018, 10, 279. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Colilla, M.; Vallet-Regí, M. Smart Mesoporous Nanomaterials for Antitumor Therapy. Nanomaterials 2015, 5, 1906–1937. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Lozano, D.; Colilla, M.; Vallet-Regí, M. Selective topotecan delivery to cancer cells by targeted pH-sensitive mesoporous silica nanoparticles. RSC Adv. 2016, 6, 50923–50932. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Lozano, D.; Colilla, M.; Vallet-Regí, M. Lectin-conjugated pH-responsive mesoporous silica nanoparticles for targeted bone cancer treatment. Acta Biomater. 2017, 65, 393–404. [Google Scholar] [CrossRef]
- Destino, J.F.; Kraut, N.D.; Hargrave, L.E.; Bright, F.V. Robust pH-responsive group IV metal oxide functionalized porous silicon platforms. Mater. Lett. 2016, 181, 47–51. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Ho, Q.P.; Morand, J.; García, A.; Ortega, E.; Erthal, L.C.S.; Ruiz-Hernandez, E.; Santana, M.D.; Ruiz, J.; Vallet-Regí, M.; et al. Amino-Functionalized Mesoporous Silica Nanoparticle-Encapsulated Octahedral Organoruthenium Complex as an Efficient Platform for Combatting Cancer. Inorg. Chem. 2020, 59, 10275–10284. [Google Scholar] [CrossRef] [PubMed]
- Bernardos, A.; Mondragon, L.; Aznar, E.; Marcos, M.D.; Martinez-Mañez, R.; Sancenon, F.; Soto, J.; Barat, J.M.; Perez-Paya, E.; Guillem, C.; et al. Enzyme-responsive intracellular controlled release using nanometric silica mesoporous supports capped with “saccharides”. ACS Nano 2010, 4, 6353–6368. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Liu, F.; Shao, Q.; Min, Y.; Costa, M.; Yeow, E.K.L.; Xing, B. Enzyme-responsive cell-penetrating peptide conjugated mesoporous silica quantum dot nanocarriers for controlled release of nucleus-targeted drug molecules and real-time intracellular fluorescence imaging of tumor cells. Adv. Healthc. Mater. 2014, 3, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Martinez-Carmona, M.; Lozano, D.; Baeza, A.; Colilla, M.; Vallet-Regi, M. A novel visible light responsive nanosystem for cancer treatment. Nanoscale 2017, 9, 15967–15973. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, J.; Zhang, W.; Gao, Y.; Tong, H.; Chen, Z.; Shi, J.; Santos, H.A.; Xia, B. Near-infrared light and magnetic field dual-responsive porous silicon-based nanocarriers to overcome multidrug resistance in breast cancer cells with enhanced efficiency. J. Mater. Chem. B 2020, 8, 546–557. [Google Scholar] [CrossRef]
- Paris, J.L.; Cabanas, M.V.; Manzano, M.; Vallet-Regí, M. Polymer-Grafted Mesoporous Silica Nanoparticles as Ultrasound-Responsive Drug Carriers. ACS Nano 2015, 9, 11023–11033. [Google Scholar] [CrossRef] [Green Version]
- Baeza, A.; Guisasola, E.; Ruiz-Hernandez, E.; Vallet-Regi, M. Magnetically Triggered Multidrug Release by Hybrid Mesoporous Silica Nanoparticles. Chem. Mater. 2012, 24, 517–524. [Google Scholar] [CrossRef]
- Vallet-Regí, M.; Lozano, D.; González, B.; Izquierdo-Barba, I. Biomaterials against Bone Infection. Adv. Healthc. Mater. 2020, 2000310. [Google Scholar] [CrossRef]
- Vallet-Regi, M.; Rámila, A.; del Real, R.P.; Pérez-Pariente, J. A New Property of MCM-41: Drug Delivery System. Chem. Mater. 2001, 13, 308–311. [Google Scholar] [CrossRef]
- Huh, A.J.; Kwon, Y.J. “Nanoantibiotics”: A new paradigm for treating infectious diseases using nanomaterials in the antibiotics resistant era. J. Control. Release 2011, 156, 128–145. [Google Scholar] [CrossRef]
- Jaganathan, H.; Godin, B. Biocompatibility assessment of Si-based nano-and micro-particles. Adv. Drug Deliv. Rev. 2012, 64, 1800–1819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asefa, T.; Tao, Z. Biocompatibility of Mesoporous Silica Nanoparticles. Chem. Res. Toxicol. 2012, 25, 2265–2284. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Yun, H.-S.; Kim, S.-H. The comparative effects of mesoporous silica nanoparticles and colloidal silica on inflammation and apoptosis. Biomaterials 2011, 32, 9434–9443. [Google Scholar] [CrossRef] [PubMed]
- Hon, N.K.; Shaposhnik, Z.; Diebold, E.D.; Tamanoi, F.; Jalali, B. Tailoring the biodegradability of porous silicon nanoparticles. J. Biomed. Mater. Res. A 2012, 100, 3416–3421. [Google Scholar] [CrossRef]
- Bhavsar, D.; Patel, V.; Sawant, K. Systematic investigation of in vitro and in vivo safety, toxicity and degradation of mesoporous silica nanoparticles synthesized using commercial sodium silicate. Microporous Mesoporous Mater. 2019, 284, 343–352. [Google Scholar] [CrossRef]
- Yang, S.-A.; Choi, S.; Jeon, S.M.; Yu, J. Silica nanoparticle stability in biological media revisited. Sci. Rep. 2018, 8, 185. [Google Scholar] [CrossRef] [Green Version]
- Yildirim, A.; Bayindir, M. A porosity difference based selective dissolution strategy to prepare shape-tailored hollow mesoporous silica nanoparticles. J. Mater. Chem. A 2015, 3, 3839–3846. [Google Scholar] [CrossRef]
- Kang, R.H.; Lee, S.H.; Kang, S.; Kang, J.; Hur, J.K.; Kim, D. Systematic degradation rate analysis of surface-functionalized porous silicon nanoparticles. Materials 2019, 12, 580. [Google Scholar] [CrossRef] [Green Version]
- Oya, N.; Kurs, C.; Tümtas, Y.; Yas, Ö.; Ortac, B. Particuology Novel one-step synthesis of silica nanoparticles from sugarbeet bagasse by laser ablation and their effects on the growth of freshwater algae culture. Particuology 2014, 17, 29–35. [Google Scholar] [CrossRef]
- He, Q.; Zhang, Z.; Gao, Y.; Shi, J.; Li, Y. Intracellular localization and cytotoxicity of spherical mesoporous silica nano- and microparticles. Small 2009, 5, 2722–2729. [Google Scholar] [CrossRef]
- Brzozowska, W.; Sprynskyy, M.; Wojtczak, I. “Outsourcing” Diatoms in Fabrication of Metal-Doped 3D Biosilica. Materials 2020, 13, 2576. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Schröder, H.C.; Wiens, M.; Schloßmacher, U.; Müller, W.E.G. Chapter five-Biosilica: Molecular Biology, Biochemistry and Function in Demosponges as well as its Applied Aspects for Tissue Engineering. In Advances in Sponge Science: Physiology, Chemical and Microbial Diversity, Biotechnology; Becerro, M.A., Uriz, M.J., Maldonado, M., Turon, X., Eds.; Advances in Marine Biology; Elsevier: London, UK, 2012; Volume 62, pp. 231–271. [Google Scholar]
- Jiang, W.; Luo, S.; Liu, P.; Deng, X.; Jing, Y.; Bai, C.; Li, J. Purification of biosilica from living diatoms by a two-step acid cleaning and baking method. J. Appl. Phycol. 2014, 26, 1511–1518. [Google Scholar] [CrossRef]
- Kabashin, A.; Delaporte, P.; Pereira, A.; Grojo, D.; Torres, R.; Sarnet, T.; Sentis, M. Nanofabrication with pulsed lasers. Nanoscale Res. Lett. 2010, 5, 454–463. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rawat, R.; Tiwari, A.; Vendamani, V.S.; Pathak, A.P.; Rao, S.V.; Tripathi, A. Synthesis of Si/SiO2 nanoparticles using nanosecond laser ablation of silicate-rich garnet in water. Opt. Mater. 2018, 75, 350–356. [Google Scholar] [CrossRef]
- Fibroblasts, L.; Voicu, S.N.; Balas, M.; Stan, M.S.; Tric, B.; Serban, A.I.; Stanca, L.; Hermenean, A.; Dinischiotu, A. Amorphous Silica Nanoparticles Obtained by Laser Ablation Induce Inflammatory Response in Human. Materials 2019, 12, 1026. [Google Scholar] [CrossRef] [Green Version]
- Kim, M.; Osone, S.; Kim, T.; Higashi, H.; Seto, T. Synthesis of Nanoparticles by Laser Ablation: A Review. KONA Powder Part. J. 2017, 34, 80–90. [Google Scholar] [CrossRef] [Green Version]
- Kannatey-Asibu, E. Background on Laser Processing. In Principles of Laser Materials Processing; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2008; pp. 407–430. ISBN 9780470459300. [Google Scholar]
- Steen, W.M. Laser material processing—An overview. J. Opt. A Pure Appl. Opt. 2003, 5, S3–S7. [Google Scholar] [CrossRef]
- Eason, R. (Ed.) Pulsed Laser Deposition of Thin Films: Applications-Led Growth of Functional Materials; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2007; ISBN 9780470052129. [Google Scholar]
- Kabashin, A.V.; Singh, A.; Swihart, M.T.; Zavestovskaya, I.N.; Prasad, P.N. Laser-Processed Nanosilicon: A Multifunctional Nanomaterial for Energy and Healthcare. ACS Nano 2019, 13, 9841–9867. [Google Scholar] [CrossRef]
- Mathelié-Guinlet, M.; Grauby-Heywang, C.; Martin, A.; Février, H.; Moroté, F.; Vilquin, A.; Béven, L.; Delville, M.-H.; Cohen-Bouhacina, T. Detrimental impact of silica nanoparticles on the nanomechanical properties of Escherichia coli, studied by AFM. J. Colloid Interface Sci. 2018, 529, 53–64. [Google Scholar] [CrossRef] [Green Version]
- Mathelié-Guinlet, M.; Béven, L.; Moroté, F.; Moynet, D.; Grauby-Heywang, C.; Gammoudi, I.; Delville, M.; Cohen-Bouhacina, T. Probing the threshold of membrane damage and cytotoxicity effects induced by silica nanoparticles in Escherichia coli bacteria. Adv. Colloid Interface Sci. 2017, 245, 81–91. [Google Scholar] [CrossRef]
- Wang, L.; Hu, C.; Shao, L. The antimicrobial activity of nanoparticles: Present situation and prospects for the future. Int. J. Nanomed. 2017, 12, 1227–1249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krasnok, A.E.; Maksymov, I.S.; Denisyuk, A.I.; Belov, P.A.; Miroshnichenko, A.E.; Simovski, C.R.; Kivshar, Y.S. Optical nanoantennas. Phys. Uspekhi 2013, 56, 539–564. [Google Scholar] [CrossRef]
- Siew, W.O.; Yap, S.S.; Ladam, C.; Dahl, Ø.; Reenaas, T.W.; Tou, T.Y. Nanosecond laser ablation and deposition of silicon. Appl. Phys. A 2011, 104, 877–881. [Google Scholar] [CrossRef] [Green Version]
- Gongalsky, M.B.; Osminkina, L.A.; Pereira, A.; Manankov, A.A.; Fedorenko, A.A.; Vasiliev, A.N.; Solovyev, V.V.; Kudryavtsev, A.A.; Sentis, M.; Kabashin, A.V.; et al. Laser-synthesized oxide-passivated bright Si quantum dots for bioimaging. Sci. Rep. 2016, 6, 24732. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zekic, A.A.; Popovic, D.M.; Kushima, A.; Bogdanovic, M.I.; Chai, J.S. Continuous wave laser for tailoring the photoluminescence of silicon nanoparticles produced by laser ablation in liquid. J. Appl. Phys. 2017, 122, 113107. [Google Scholar] [CrossRef]
- Werwa, E.; Seraphin, A.A.; Chiu, L.A.; Zhou, C.; Kolenbrander, K.D. Synthesis and processing of silicon nanocrystallites using a pulsed laser ablation supersonic expansion method. Appl. Phys. Lett. 1994, 64, 1821–1823. [Google Scholar] [CrossRef]
- Makimura, T.; Kunii, Y.; Ono, N.; Murakami, K. Silicon nanoparticles embedded in SiO2 films with visible photoluminescence. Appl. Surf. Sci. 1998, 127–129, 388–392. [Google Scholar] [CrossRef]
- Movtchan, I.A.; Marine, W.; Dreyfus, R.W.; Le, H.C.; Sentis, M.; Autric, M. Optical spectroscopy of emission from Si—SiOx nanoclusters formed by laser ablation. Appl. Surf. Sci. 1996, 96–98, 251–260. [Google Scholar] [CrossRef]
- Patrone, L.; Nelson, D.; Safarov, V.I.; Sentis, M.; Marine, W.; Giorgio, S. Photoluminescence of silicon nanoclusters with reduced size dispersion produced by laser ablation. J. Appl. Phys. 2000, 87, 3829–3837. [Google Scholar] [CrossRef]
- Suzuki, N.; Makino, T.; Yamada, Y.; Yoshida, T.; Onari, S. Structures and optical properties of silicon nanocrystallites prepared by pulsed-laser ablation in inert background gas. Appl. Phys. Lett. 2000, 76, 1389–1391. [Google Scholar] [CrossRef]
- Kabashin, A.V.; Sylvestre, J.-P.; Patskovsky, S.; Meunier, M. Correlation between photoluminescence properties and morphology of laser-ablated Si/SiOx nanostructured films. J. Appl. Phys. 2002, 91, 3248–3254. [Google Scholar] [CrossRef] [Green Version]
- Kruusing, A. Underwater and water-assisted laser processing: Part 1—General features, steam cleaning and shock processing. Opt. Lasers Eng. 2004, 41, 307–327. [Google Scholar] [CrossRef]
- Krivonosov, A.; Zuev, D.; Kaputkina, S.; Mikhailovskii, V.; Egorova, E.; Ageev, E.; Odintsova, G. Evolution of size distribution of Si nanoparticles produced by pulsed laser ablation in water. Opt. Quantum Electron. 2020, 52, 158. [Google Scholar] [CrossRef]
- González-Castillo, J.R.; Rodriguez, E.; Rodríguez, D.; De Sá, G.F.; Almeida, D.B.; Cesar, C.L.; Johnes, R.; Ibarra, J.C. Synthesis of Ag @ Silica Nanoparticles by Assisted Laser Ablation. Nanoscale Res. Lett. 2015, 10, 399. [Google Scholar] [CrossRef] [Green Version]
- Intartaglia, R.; Bagga, K.; Brandi, F. Study on the productivity of silicon nanoparticles by picosecond laser ablation in water: Towards gram per hour yield. Opt. Express 2014, 22, 8350–8356. [Google Scholar] [CrossRef]
- Zhang, D.; Gökce, B.; Barcikowski, S. Laser Synthesis and Processing of Colloids: Fundamentals and Applications. Chem. Rev. 2017, 117, 3990–4103. [Google Scholar] [CrossRef]
- Yang, S.; Cai, W.; Zhang, H.; Xu, X.; Zeng, H. Size and Structure Control of Si Nanoparticles by Laser Ablation in Different Liquid Media and Further Centrifugation Classification. J. Phys. Chem. C 2009, 113, 19091–19095. [Google Scholar] [CrossRef]
- Intartaglia, R.; Bagga, K.; Genovese, A.; Athanassiou, A.; Cingolani, R.; Diaspro, A.; Brandi, F. Influence of organic solvent on optical and structural properties of ultra-small silicon dots synthesized by UV laser ablation in liquid. Phys. Chem. Chem. Phys. 2012, 14, 15406–15411. [Google Scholar] [CrossRef]
- Abderra, K.; Calzada, G.; Gongalsky, M.B.; Su, I.; Abarques, R.; Chirvony, V.S.; Timoshenko, V.Y.; Ib, R. Silicon Nanocrystals Produced by Nanosecond Laser Ablation in an Organic Silicon Nanocrystals Produced by Nanosecond Laser Ablation in an Organic Liquid. J. Phys. Chem. C 2011, 115, 5147–5151. [Google Scholar] [CrossRef]
- Mansour, N.; Momeni, A.; Karimzadeh, R.; Amini, M. Blue-green luminescent silicon nanocrystals fabricated by nanosecond pulsed laser ablation in dimethyl sulfoxide. Opt. Mater. Express 2012, 2, 740–748. [Google Scholar] [CrossRef]
- Taheri, M.; Mansour, N. Silicon Nanoparticles Produced by Two-Step Nanosecond Pulsed Laser Ablation in Ethanol for Enhanced Blue Emission Properties. Silicon 2020, 12, 789–797. [Google Scholar] [CrossRef]
- Sportelli, M.C.; Izzi, M.; Volpe, A.; Clemente, M.; Picca, R.A.; Ancona, A.; Lugarà, P.M.; Palazzo, G.; Cioffi, N. The Pros and Cons of the Use of Laser Ablation Synthesis for the Production of Silver Nano-Antimicrobials. Antibiotics 2018, 7, 67. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaleard, C.; Detalle, V.; Kocon, S.; Lacour, J.-L.; Mauchien, P.; Meynadier, P.; Nouvellon, C.; Palianov, P.; Perdrix, M.; Petite, G.; et al. Influence of laser pulse duration on the ablation efficiency of metals. In Proceedings of the ALT’97 International Conference on Laser Surface Processing, Limoges, France, 8–12 September 1997; Pustovoy, V.I., Ed.; SPIE: Bellingham, WA, USA, 1998; Volume 3404, pp. 441–448. [Google Scholar]
- Nathala, C.S.R.; Ajami, A.; Husinsky, W.; Farooq, B.; Kudryashov, S.I.; Daskalova, A.; Bliznakova, I.; Assion, A. Ultrashort laser pulse ablation of copper, silicon and gelatin: Effect of the pulse duration on the ablation thresholds and the incubation coefficients. Appl. Phys. A 2016, 122, 107. [Google Scholar] [CrossRef] [Green Version]
- Giguère, D.; Olivié, G.; Vidal, F.; Toetsch, S.; Girard, G.; Ozaki, T.; Kieffer, J.-C.; Nada, O.; Brunette, I. Laser ablation threshold dependence on pulse duration for fused silica and corneal tissues: Experiments and modeling. J. Opt. Soc. Am. A Opt. Image Sci. Vis. 2007, 24, 1562–1568. [Google Scholar] [CrossRef]
- Tsuji, T.; Tsuboi, Y.; Kitamura, N.; Tsuji, M. Microsecond-resolved imaging of laser ablation at solid–liquid interface: Investigation of formation process of nano-size metal colloids. Appl. Surf. Sci. 2004, 229, 365–371. [Google Scholar] [CrossRef]
- Evlyukhin, A.B.; Novikov, S.M.; Zywietz, U.; Eriksen, R.L.; Reinhardt, C.; Bozhevolnyi, S.I.; Chichkov, B.N. Demonstration of magnetic dipole resonances of dielectric nanospheres in the visible region. Nano Lett. 2012, 12, 3749–3755. [Google Scholar] [CrossRef]
- Zywietz, U.; Evlyukhin, A.B.; Reinhardt, C.; Chichkov, B.N. Laser printing of silicon nanoparticles with resonant optical electric and magnetic responses. Nat. Commun. 2014, 5, 3402. [Google Scholar] [CrossRef]
- Zywietz, U.; Reinhardt, C.; Evlyukhin, A.B.; Birr, T.; Chichkov, B.N. Generation and patterning of Si nanoparticles by femtosecond laser pulses. Appl. Phys. A 2014, 114, 45–50. [Google Scholar] [CrossRef]
- Levoska, J.; Tyunina, M.; Leppävuori, S. Laser ablation deposition of silicon nanostructures. Nanostruct. Mater. 1999, 12, 101–106. [Google Scholar] [CrossRef]
- Zhou, R.; Huang, T.T.; Lin, S.D. Synthesis of nanoparticles by pulsed laser ablation in air: A versatile means for flexible synthesis and separation. In Proceedings of the Advanced Laser Processing and Manufacturing, Beijing, China, 13 October 2016; Zhong, M., Lawrence, J., Hong, M., Liu, J., Eds.; SPIE: Bellingham, WA, USA, 2016; Volume 10018, pp. 33–39. [Google Scholar]
- Zhai, X.; Song, B.; Chu, B.; Su, Y.; Wang, H.; He, Y. Highly fluorescent, photostable, and biocompatible silicon theranostic nanoprobes against Staphylococcus aureus infections. Nano Res. 2018, 11, 6417–6427. [Google Scholar] [CrossRef]
- Qi, G.; Li, L.; Yu, F.; Wang, H. Vancomycin-modified mesoporous silica nanoparticles for selective recognition and killing of pathogenic gram-positive bacteria over macrophage-like cells. ACS Appl. Mater. Interfaces 2013, 5, 10874–10881. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xu, Y.; Wang, R.; Zhao, B.; Zhang, X.; Zhao, H. Detection of Staphylococcus aureus using acridine orange-doped silica nanoparticles as a fluorescent label. RSC Adv. 2015, 5, 54338–54344. [Google Scholar] [CrossRef]
- Wang, Q.-Y.; Kang, Y.-J. Bioprobes Based on Aptamer and Silica Fluorescent Nanoparticles for Bacteria Salmonella typhimurium Detection. Nanoscale Res. Lett. 2016, 11, 150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, J.; Chu, B.; Wang, J.; Song, B.; Su, Y.; Wang, H.; He, Y. Multifunctional nanoagents for ultrasensitive imaging and photoactive killing of Gram-negative and Gram-positive bacteria. Nat. Commun. 2019, 10, 4057. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Carmona, M.; Izquierdo-Barba, I.; Colilla, M.; Vallet-Regí, M. Concanavalin A-targeted mesoporous silica nanoparticles for infection treatment. Acta Biomater. 2019, 96, 547–556. [Google Scholar] [CrossRef] [PubMed]
- González, B.; Colilla, M.; Díez, J.; Pedraza, D.; Guembe, M.; Izquierdo-Barba, I.; Vallet-Regí, M. Mesoporous silica nanoparticles decorated with polycationic dendrimers for infection treatment. Acta Biomater. 2018, 68, 261–271. [Google Scholar] [CrossRef]
- Pedraza, D.; Díez, J.; Isabel-Izquierdo-Barba; Colilla, M.; Vallet-Regí, M. Amine-Functionalized Mesoporous Silica Nanoparticles: A New Nanoantibiotic for Bone Infection Treatment. Biomed. Glasses 2018, 4, 1–12. [Google Scholar] [CrossRef] [Green Version]
- Koneru, B.; Shi, Y.; Wang, Y.; Chavala, S.; Miller, M.; Holbert, B.; Conson, M.; Ni, A.; Di Pasqua, A. Tetracycline-Containing MCM-41 Mesoporous Silica Nanoparticles for the Treatment of Escherichia coli. Molecules 2015, 20, 19690–19698. [Google Scholar] [CrossRef] [Green Version]
- Subramaniam, S.; Thomas, N.; Gustafsson, H.; Jambhrunkar, M.; Kidd, S.P.; Prestidge, C.A. Rifampicin-Loaded Mesoporous Silica Nanoparticles for the Treatment of Intracellular Infections. Antibiotics 2019, 8, 39. [Google Scholar] [CrossRef] [Green Version]
- Kwon, E.J.; Skalak, M.; Bertucci, A.; Braun, G.; Ricci, F.; Ruoslahti, E.; Sailor, M.J.; Bhatia, S.N. Porous Silicon Nanoparticle Delivery of Tandem Peptide Anti-Infectives for the Treatment of Pseudomonas aeruginosa Lung Infections. Adv. Mater. 2017, 29, 1701527. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parasuraman, P.; Antony, A.P.; Sharan, A.; Siddhardha, B.; Kasinathan, K.; Bahkali, N.A.; Dawoud, T.M.; Syed, A. Antimicrobial photodynamic activity of toluidine blue encapsulated in mesoporous silica nanoparticles against Pseudomonas aeruginosa and Staphylococcus aureus. Biofouling 2019, 35, 89–103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Guo, Y.; Rogelj, S.; Zhang, P. Rose Bengal-decorated silica nanoparticles as photosensitizers for inactivation of gram-positive bacteria. Nanotechnology 2010, 21, 65102. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, A.W.; Worley, B.V.; Slomberg, D.L.; Schoen, M.H. Dual Action Antimicrobials: Nitric Oxide Release from Quaternary Ammonium-Functionalized Silica Nanoparticles. Biomacromolecules 2012, 13, 3334–3342. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jeong, H.E.; Kim, I.; Karam, P.; Choi, H.-J.; Yang, P. Bacterial recognition of silicon nanowire arrays. Nano Lett. 2013, 13, 2864–2869. [Google Scholar] [CrossRef] [PubMed]
- Cousins, B.G.; Allison, H.E.; Doherty, P.J.; Edwards, C.; Garvey, M.J.; Martin, D.S.; Williams, R.L. Effects of a nanoparticulate silica substrate on cell attachment of Candida albicans. J. Appl. Microbiol. 2007, 102, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Gaidhani, S.; Singh, R.; Singh, D.; Patel, U.; Shevade, K.; Yeshvekar, R.; Ananda Chopade, B. Biofilm disruption activity of silver nanoparticles synthesized by Acinetobacter calcoaceticus PUCM 1005. Mater. Lett. 2013, 108, 324–327. [Google Scholar] [CrossRef]
- Lu, T.K.; Collins, J.J. Dispersing biofilms with engineered enzymatic bacteriophage. Proc. Natl. Acad. Sci. USA 2007, 104, 11197–11202. [Google Scholar] [CrossRef] [Green Version]
- Ghaffari, A.; Miller, C.C.; McMullin, B.; Ghahary, A. Potential application of gaseous nitric oxide as a topical antimicrobial agent. Nitric Oxide Biol. Chem. 2006, 14, 21–29. [Google Scholar] [CrossRef]
- Hasanzadeh Kafshgari, M.; Delalat, B.; Harding, F.J.; Cavallaro, A.; Mäkilä, E.; Salonen, J.; Vasilev, K.; Voelcker, N.H. Antibacterial properties of nitric oxide-releasing porous silicon nanoparticles. J. Mater. Chem. B 2016, 4, 2051–2058. [Google Scholar] [CrossRef]
- Mosselhy, D.A.; Granbohm, H.; Hynönen, U.; Ge, Y.; Palva, A.; Nordström, K.; Hannula, S.-P. Nanosilver-Silica Composite: Prolonged Antibacterial Effects and Bacterial Interaction Mechanisms for Wound Dressings. Nanomaterials 2017, 7, 261. [Google Scholar] [CrossRef]
- Fellahi, O.; Sarma, R.K.; Das, M.R.; Saikia, R.; Marcon, L.; Coffinier, Y.; Hadjersi, T.; Maamache, M.; Boukherroub, R. The antimicrobial effect of silicon nanowires decorated with silver and copper nanoparticles. Nanotechnology 2013, 24, 495101. [Google Scholar] [CrossRef]
- Smirnov, N.A.; Kudryashov, S.I.; Nastulyavichus, A.A.; Rudenko, A.A.; Saraeva, I.N.; Tolordava, E.R.; Gonchukov, S.A.; Romanova, Y.M.; Ionin, A.A.; Zayarny, D.A. Antibacterial properties of silicon nanoparticles. Laser Phys. Lett. 2018, 15, 105602. [Google Scholar] [CrossRef]
- Kudryashov, S.I.; Nastulyavichus, A.A.; Ivanova, A.K.; Smirnov, N.A.; Khmelnitskiy, R.A.; Rudenko, A.A.; Saraeva, I.N.; Tolordava, E.R.; Kharin, A.Y.; Zavestovskaya, I.N.; et al. High-throughput laser generation of Si-nanoparticle based surface coatings for antibacterial applications. Appl. Surf. Sci. 2019, 470, 825–831. [Google Scholar] [CrossRef]
- Bonse, J.; Höhm, S.; Kirner, S.V.; Rosenfeld, A.; Krüger, J. Laser-Induced Periodic Surface Structures—A Scientific Evergreen. IEEE J. Sel. Top. Quantum Electron. 2017, 23. [Google Scholar] [CrossRef]
- Reif, J.; Costache, F.; Henyk, M.; Pandelov, S.V. Ripples revisited: Non-classical morphology at the bottom of femtosecond laser ablation craters in transparent dielectrics. Appl. Surf. Sci. 2002, 197–198, 891–895. [Google Scholar] [CrossRef]
- Kudryashov, S.I.; Nguyen, L.V.; Kirilenko, D.A.; Brunkov, P.N.; Rudenko, A.A.; Busleev, N.I.; Shakhmin, A.L.; Semencha, A.V.; Khmelnitsky, R.A.; Melnik, N.N.; et al. Large-Scale Laser Fabrication of Antifouling Silicon-Surface Nanosheet Arrays via Nanoplasmonic Ablative Self-Organization in Liquid CS2 Tracked by a Sulfur Dopant. ACS Appl. Nano Mater. 2018, 1, 2461–2468. [Google Scholar] [CrossRef]
- Saraeva, I.N.; Tolordava, E.R.; Nastulyavichus, A.A. A bacterial misericorde: Laser-generated silicon nanorazors with embedded biotoxic nanoparticles combat the formation of durable biofilms. Laser Phys. Lett. 2020, 17, 025601. [Google Scholar] [CrossRef]
- Papavlu, A.P.; Dinca, V.; Filipescu, M.; Dinescu, M. Matrix-Assisted Pulsed Laser Evaporation of Organic Thin Films: Applications in Biology and Chemical Sensors. In Laser Ablation; Itina, T.E., Ed.; IntechOpen: Rijeka, Croatia, 2017. [Google Scholar]
- Chrisey, D.B.; Piqué, A.; McGill, R.A.; Horwitz, J.S.; Ringeisen, B.R.; Bubb, D.M.; Wu, P.K. Laser deposition of polymer and biomaterial films. Chem. Rev. 2003, 103, 553–576. [Google Scholar] [CrossRef]
- Mihaiescu, D.E.; Cristescu, R.; Dorcioman, G.; Popescu, C.E.; Nita, C.; Socol, G.; Mihailescu, I.N.; Grumezescu, A.M.; Tamas, D.; Enculescu, M.; et al. Functionalized magnetite silica thin films fabricated by MAPLE with antibiofilm properties. Biofabrication 2013, 5, 15007. [Google Scholar] [CrossRef] [Green Version]
- Kögler, M.; Ryabchikov, Y.V.; Uusitalo, S.; Popov, A.; Popov, A.; Tselikov, G.; Välimaa, A.-L.; Al-Kattan, A.; Hiltunen, J.; Laitinen, R.; et al. laser-synthesized Au-based nanoparticles as nondisturbing surface-enhanced Raman scattering probes for bacteria identification. J. Biophotonics 2018, 11, e201700225. [Google Scholar] [CrossRef] [Green Version]









© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Carmona, M.; Vallet-Regí, M. Advances in Laser Ablation Synthesized Silicon-Based Nanomaterials for the Prevention of Bacterial Infection. Nanomaterials 2020, 10, 1443. https://doi.org/10.3390/nano10081443
Martínez-Carmona M, Vallet-Regí M. Advances in Laser Ablation Synthesized Silicon-Based Nanomaterials for the Prevention of Bacterial Infection. Nanomaterials. 2020; 10(8):1443. https://doi.org/10.3390/nano10081443
Chicago/Turabian StyleMartínez-Carmona, Marina, and María Vallet-Regí. 2020. "Advances in Laser Ablation Synthesized Silicon-Based Nanomaterials for the Prevention of Bacterial Infection" Nanomaterials 10, no. 8: 1443. https://doi.org/10.3390/nano10081443