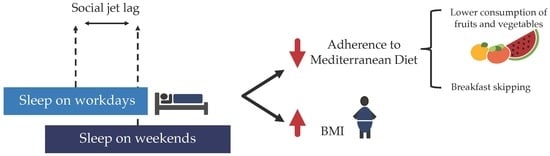
Social Jet Lag Associates Negatively with the Adherence to the Mediterranean Diet and Body Mass Index among Young Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Settings, Participants and Protocol
2.2. Data Collection
2.3. Anthropometric Parameters
2.4. Adherence to the Mediterranean Diet
2.5. Sleep Duration
2.6. Social Jet Lag
2.7. Chronotype
2.8. Physical Activity
2.9. Statistical Analyses
3. Results
3.1. Participants’ Characteristics, Social Jet Lag and Adherence to the Mediterranean Diet
3.2. Higher Social Jet Lag Is Associated with a Lower Adherence to the Mediterranean Diet and Higher BMI
3.3. Social Jet Lag Is Associated with Lower Intake of Fruits, Vegetables and Breakfast Skipping
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nelson, M.C.; Story, M.; Larson, N.I.; Neumark-Sztainer, D.; Lytle, L.A. Emerging Adulthood and College-aged Youth: An Overlooked Age for Weight-related Behavior Change. Obesity (Silver Spring) 2008, 16, 2205–2211. [Google Scholar] [CrossRef] [PubMed]
- Serra-Majem, L.; Ribas, L.; Ngo, J.; Ortega, R.M.; García, A.; Pérez-Rodrigo, C.; Aranceta, J. Food, youth and the Mediterranean diet in Spain. Development of KIDMED, Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2004, 7, 931–935. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P.; Dutil, C. Lack of sleep as a contributor to obesity in adolescents: Impacts on eating and activity behaviors. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 174. [Google Scholar] [CrossRef] [PubMed]
- CIHEAM/FAO. Mediterranean Food Consumption Patterns and Health; A White Paper Priority 5 of Feeding Knowledge Programme; Food and Agriculture Organization of the United Nations: Rome, Italy, 2015. [Google Scholar]
- Stok, F.M.; Renner, B.; Clarys, P.; Lien, N.; Lakerveld, J.; Deliens, T. Understanding Eating Behavior during the Transition from Adolescence to Young Adulthood: A Literature Review and Perspective on Future Research Directions. Nutrients 2018, 10, 667. [Google Scholar] [CrossRef] [PubMed]
- Arcila-Agudelo, A.M.; Ferrer-Svoboda, C.; Torres-Fernández, T.; Farran-Codina, A. Determinants of Adherence to Healthy Eating Patterns in a Population of Children and Adolescents. Nutrients 2019, 11, 854. [Google Scholar] [CrossRef] [PubMed]
- Bendall, C.L.; Mayr, H.L.; Opie, R.S.; Bes-Rastrollo, M.; Itsiopoulos, C.; Thomas, C.J. Central obesity and the Mediterranean diet: A systematic review of intervention trials. Crit. Rev. Food Sci. Nutr. 2018, 58, 3070–3084. [Google Scholar] [CrossRef]
- Donini, L.M.; Serra-Majem, L.; Bulló, M.; Gil, A.; Salas-Salvadó, J. The Mediterranean diet: Culture, health and science. Br. J. Nutr. 2015, 113, S1–S3. [Google Scholar] [CrossRef]
- Ríos-Hernández, A.; Alda, J.A.; Farran-Codina, A.; Ferreira-García, E.; Izquierdo-Pulido, M. The Mediterranean Diet and ADHD in Children and Adolescents. Pediatrics 2017, 139, 20162027. [Google Scholar] [CrossRef]
- Potter, G.D.M.; Skene, D.J.; Arendt, J.; Cade, J.E.; Grant, P.J.; Hardie, L.J. Circadian Rhythm and Sleep Disruption: Causes, Metabolic Consequences, and Countermeasures. Endocr. Rev. 2016, 37, 584–608. [Google Scholar] [CrossRef] [Green Version]
- Wong, P.M.; Hasler, B.P.; Kamarck, T.W.; Muldoon, M.F.; Manuck, S.B. Social Jetlag, Chronotype, and Cardiometabolic Risk. J. Clin. Endocrinol. Metab. 2015, 100, 4612–4620. [Google Scholar] [CrossRef]
- Roenneberg, T.; Allebrandt, K.V.; Merrow, M.; Vetter, C. Social Jetlag and Obesity. Curr. Biol. 2012, 23, 737. [Google Scholar] [CrossRef]
- Moreno, J.P.; Crowley, S.J.; Alfano, C.A.; Hannay, K.M.; Thompson, D.; Baranowski, T. Potential circadian and circannual rhythm contributions to the obesity epidemic in elementary school age children. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 25. [Google Scholar] [CrossRef] [PubMed]
- Im, H.; Baek, S.; Chu, M.K.; Yang, K.I.; Kim, W.; Park, S.-H.; Thomas, R.J.; Yun, C. Association Between Weekend Catch-up Sleep and Lower Body Mass: Population-Based Study. Sleep 2018, 40, zsx089. [Google Scholar] [CrossRef] [PubMed]
- Wittmann, M.; Dinich, J.; Merrow, M.; Roenneberg, T. Social Jetlag: Misalignment of Biological and Social Time. Chronobiol. Int. 2006, 23, 497–509. [Google Scholar] [CrossRef] [PubMed]
- Roenneberg, T.; Kuehnle, T.; Pramstaller, P.P.; Ricken, J.; Havel, M.; Guth, A.; Merrow, M. A marker for the end of adolescence. Curr. Biol. 2004, 14, R1038–R1039. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parsons, M.J.; Moffitt, T.E.; Gregory, A.M.; Goldman-Mellor, S.; Nolan, P.M.; Poulton, R.; Caspi, A. Social jetlag, obesity and metabolic disorder: Investigation in a cohort study. Int. J. Obes. (Lond.) 2015, 39, 842–848. [Google Scholar] [CrossRef] [PubMed]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Fahmy, W.M.; Crispim, C.A. Social jetlag and metabolic control in non-communicable chronic diseases: A study addressing different obesity statuses. Sci. Rep. 2017, 7, 6358. [Google Scholar] [CrossRef]
- Malone, S.K.; Zemel, B.; Compher, C.; Souders, M.; Chittams, J.; Thompson, A.L.; Pack, A.; Lipman, T.H. Social jet lag, chronotype and body mass index in 14–17-year-old adolescents. Chronobiol. Int. 2016, 33, 1255–1266. [Google Scholar] [CrossRef]
- Mota, M.C.; Silva, C.M.; Balieiro, L.C.T.; Gonçalves, B.F.; Fahmy, W.M.; Crispim, C.A. Association between social jetlag food consumption and meal times in patients with obesity-related chronic diseases. PLoS ONE 2019, 14, e0212126. [Google Scholar] [CrossRef] [PubMed]
- Dobility Inc. Survey CTO. Available online: https://www.surveycto.com/ (accessed on 30 April 2019).
- Open Data Kit ODK. Available online: https://opendatakit.org/ (accessed on 30 April 2019).
- Kanerva, N.; Harald, K.; Mannisto, S.; Kaartinen, N.E.; Maukonen, M.; Haukkala, A.; Jousilahti, P. Adherence to the healthy Nordic diet is associated with weight change during 7 years of follow-up. Br. J. Nutr. 2018, 120, 101–110. [Google Scholar] [CrossRef] [Green Version]
- Ruiz-Lozano, T.; Vidal, J.; De Hollanda, A.; Canteras, M.; Garaulet, M.; Izquierdo-Pulido, M. Evening chronotype associates with obesity in severely obese subjects: Interaction with CLOCK 3111T/C. Int. J. Obes. 2016, 40, 1550–1557. [Google Scholar] [CrossRef] [PubMed]
- A Horne, J.; Ostberg, O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int. J. Chronobiol. 1976, 4, 97–110. [Google Scholar] [PubMed]
- Viñas, B.R.; Barba, L.R.; Ngo, J.; Majem, L.S. Validación en población catalana del cuestionario internacional de actividad física. Gac. Sanit. 2013, 27, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Almoosawi, S.; Palla, L.; Id, J.G.E. Long sleep duration and social jetlag are associated inversely with a healthy dietary pattern in adults: Results from the UK National diet and nutrition survey rolling programme Y1-4. Nutrients 2018, 10, 1131. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.M.; Mota, M.C.; Miranda, M.T.; Paim, S.L.; Waterhouse, J.; Crispim, C.A. Chronotype, social jetlag and sleep debt are associated with dietary intake among Brazilian undergraduate students. Chronobiol. Int. 2016, 33, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, G.P.; Mota, M.C.; Crispim, C.A. Eveningness is associated with skipping breakfast and poor nutritional intake in Brazilian undergraduate students. Chronobiol. Int. 2018, 35, 358–367. [Google Scholar] [CrossRef] [PubMed]
- Guinter, M.A.; Park, Y.M.; Steck, S.E.; Sandler, D.P. Day-to-day regularity in breakfast consumption is associated with weight status in a prospective cohort of women. Int. J. Obes. 2019. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, D.; Takahashi, O.; Shimbo, T.; Okubo, T.; Arioka, H.; Fukui, T. High sleep duration variability is an independent risk factor for weight gain. Sleep Breath 2013, 17, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Spruyt, K.; Molfese, D.L.; Gozal, D. Sleep Duration, Sleep Regularity, Body Weight, and Metabolic Homeostasis in School-aged Children. Pediatrics 2011, 127, e345–e352. [Google Scholar] [CrossRef] [Green Version]
- He, F.; Bixler, E.O.; Liao, J.; Berg, A.; Kawasawa, Y.I.; Fernandez-Mendoza, J.; Vgontzas, A.N.; Liao, D. Habitual sleep variability, mediated by nutrition intake, is associated with abdominal obesity in adolescents. Sleep Med. 2015, 16, 1489–1494. [Google Scholar] [CrossRef] [Green Version]
- Ferranti, R.; Marventano, S.; Castellano, S.; Giogianni, G.; Nolfo, F.; Rametta, S.; Matalone, M.; Mistretta, A. Sleep quality and duration is related with diet and obesity in young adolescent living in Sicily, Southern Italy. Sleep Sci. 2016, 9, 117–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adelantado-Renau, M.; Beltran-Valls, M.R.; Esteban-Cornejo, I.; Moliner-Urdiales, D. The influence of adherence to the Mediterranean diet on academic performance is mediated by sleep quality in adolescents. Acta Paediatr. 2019, 108, 339–346. [Google Scholar] [CrossRef] [PubMed]
- Godos, J.; Ferri, R.; Caraci, F.; Cosentino, F.I.I.; Castellano, S.; Galvano, F.; Grosso, G. Adherence to the Mediterranean Diet is Associated with Better Sleep Quality in Italian Adults. Nutrients 2019, 11, 976. [Google Scholar] [CrossRef] [PubMed]
- Dashti, H.S.; Scheer, F.A.; Jacques, P.F.; Lamon-Fava, S.; Ordovás, J.M. Short Sleep Duration and Dietary Intake: Epidemiologic Evidence, Mechanisms, and Health Implications12. Adv. Nutr. 2015, 6, 648–659. [Google Scholar] [CrossRef] [PubMed]
- Golem, D.L.; Martin-Biggers, J.T.; Koenings, M.M.; Davis, K.F.; Byrd-Bredbenner, C. An Integrative Review of Sleep for Nutrition Professionals12. Adv. Nutr. 2014, 5, 742–759. [Google Scholar] [CrossRef] [PubMed]
- St-Onge, M. Sleep-obesity relation: Underlying mechanisms and consequences for treatment. Obes. Rev. 2017, 18, 34–39. [Google Scholar] [CrossRef] [PubMed]
- Randler, C.; Haun, J.; Schaal, S. Assessing the Influence of Sleep-Wake Variables on Body Mass Index (BMI) in Adolescents. PsycEXTRA Dataset 2013, 9, 339–347. [Google Scholar] [CrossRef]
- Buxton, O.M.; Cain, S.W.; Connor, S.P.O.; Porter, J.H.; Duffy, J.F.; Wang, W.; Czeisler, C.A.; Shea, S.A. Adverse Metabolic Consequences in Humans of Prolonged Sleep Restriction Combined with Circadian Disruption. Sci. Transl. Med. 2012, 4, 129ra43. [Google Scholar] [CrossRef]
- Scheer, F.A.; Hilton, M.F.; Mantzoros, C.S.; Shea, S.A. Adverse metabolic and cardiovascular consequences of circadian misalignment. Proc. Natl. Acad. Sci. USA 2009, 106, 4453–4458. [Google Scholar] [CrossRef] [Green Version]
- Arora, T.; Taheri, S. Associations among late chronotype, body mass index and dietary behaviors in young adolescents. Int. J. Obes. 2015, 39, 39–44. [Google Scholar] [CrossRef]
- Vera, B.; Dashti, H.S.; Gómez-Abellán, P.; Hernández-Martínez, A.M.; Esteban, A.; Scheer, F.A.J.L.; Saxena, R.; Garaulet, M. Modifiable lifestyle behaviors, but not a genetic risk score, associate with metabolic syndrome in evening chronotypes. Sci. Rep. 2018, 8, 945. [Google Scholar] [CrossRef] [PubMed]
- Maukonen, M.; Kanerva, N.; Partonen, T.; Männistö, S. Chronotype and energy intake timing in relation to changes in anthropometrics: A 7-year follow-up study in adults. Chronobiol. Int. 2019, 36, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Maukonen, M.; Kanerva, N.; Partonen, T.; Kronholm, E.; Konttinen, H.; Wennman, H.; Männistö, S. The associations between chronotype, a healthy diet and obesity. Chronobiol. Int. 2016, 33, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Maukonen, M.; Kanerva, N.; Partonen, T.; Kronholm, E.; Tapanainen, H.; Kontto, J.; Männistö, S. Chronotype differences in timing of energy and macronutrient intakes: A population-based study in adults. Obesity 2017, 25, 608–615. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Total Sample (n) | 534 |
| Gender, %F | 74.3 |
| Age, years | 21.5 (3.0) |
| BMI, kg/m2 | 21.7 (3.1) |
| Underweight, % (n) | 10.1 (54) |
| Normal weight, % (n) | 77.3 (413) |
| Overweight, % (n) | 10.5 (56) |
| Obese, % (n) | 2.1 (11) |
| Physical Activity (METs) | 2353.9 (2701.5) |
| Sleep related variables | |
| Workdays | |
| Sleep onset, hh:mm | 23:51 (00:49) |
| Sleep offset, hh:mm | 07:37 (00:58) |
| Midpoint of sleep, hh:mm | 03:45 (00:46) |
| Sleep duration, hours | 7.8 (0.9) |
| Weekends | |
| Sleep onset, hh:mm | 00:54 (01:09) |
| Sleep offset, hh:mm | 09:52 (01:14) |
| Midpoint of sleep, hh:mm | 05:23 (01:04) |
| Sleep duration, hours | 9.0 (0.9) |
| Social jet lag, hours | 1.6 (0.9) |
| Chronotype | 49.0 (9.3) |
| Evening type, % (n) | 20.6 (110) |
| Intermediate type, % (n) | 62.4 (333) |
| Morning type, % (n) | 17.0 (91) |
| Population Studied (n = 534) | |
|---|---|
| KIDMED test score total, mean (SD) | 7.0 (2.1) |
| KIDMED index, % | |
| Poor (≤3 points) | 4.9 |
| Average (4–7 points) | 50.7 |
| Good (8–12 points) | 44.4 |
| KIDMED test (%, yes) | |
| Takes a fruit of fruit juice every day | 78.1 |
| Has a second serving of fruit every day | 38.6 |
| Has fresh or cooked vegetables regularly once a day | 78.8 |
| Has fresh or cooked vegetables more than once a day | 40.3 |
| Consumes fish regularly (at least 2–3 days/week) | 61.8 |
| Goes more than once a week to a fast-food (hamburger) restaurant | 13.9 |
| Likes pulses and eats them more than once a week | 72.7 |
| Consumes pasta or rice almost every day (≥5 times/week) | 43.1 |
| Has cereals or cereal products (bread) for breakfast | 89.1 |
| Consumes nuts regularly (at least 2–3 times per week) | 44.6 |
| Uses of olive oil at home | 97.9 |
| Skips breakfast | 7.7 |
| Has a dairy product for breakfast (yogurt, milk, etc.) | 72.5 |
| Takes two yogurts and/or some cheese (40 g) daily | 40.1 |
| Has commercially baked goods or pastries for breakfast | 23.0 |
| Takes sweets and candy several times every day | 4.5 |
| Adherence to Mediterranean Diet | BMI | |||||
|---|---|---|---|---|---|---|
| β | 95% CI | pa | β | 95% CI | pa | |
| Social jet lag | −0.305 | −0.503, −0.107 | 0.003 | 0.304 | 0.021, 0.587 | 0.035 |
| Chronotype | 0.019 | −0.001, 0.038 | 0.057 | −0.028 | −0.055, −0.001 | 0.043 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zerón-Rugerio, M.F.; Cambras, T.; Izquierdo-Pulido, M. Social Jet Lag Associates Negatively with the Adherence to the Mediterranean Diet and Body Mass Index among Young Adults. Nutrients 2019, 11, 1756. https://doi.org/10.3390/nu11081756
Zerón-Rugerio MF, Cambras T, Izquierdo-Pulido M. Social Jet Lag Associates Negatively with the Adherence to the Mediterranean Diet and Body Mass Index among Young Adults. Nutrients. 2019; 11(8):1756. https://doi.org/10.3390/nu11081756
Chicago/Turabian StyleZerón-Rugerio, María Fernanda, Trinitat Cambras, and Maria Izquierdo-Pulido. 2019. "Social Jet Lag Associates Negatively with the Adherence to the Mediterranean Diet and Body Mass Index among Young Adults" Nutrients 11, no. 8: 1756. https://doi.org/10.3390/nu11081756