Case Report Open Access
Bouveret Syndrome: A Case Report and Review
Anurag Mishra*, Ankit Jain, Pawanindra Lal and Hadke NS
Maulana Azad Medical College, New Delhi, India
- *Corresponding Author:
- Anurag Mishra
Maulana Azad Medical College
New Delhi, India
Tel: +919899797734
E-mail: anurag.alok@gmail.com
Received date: July 22, 2013; Accepted date: August 24, 2013; Published date: August 27, 2013
Citation: Mishra A, Jain A, Lal P, Hadke NS (2013) Bouveret Syndrome: A Case Report and Review. J Gastroint Dig Syst 3:133. doi:10.4172/2161-069X.1000133
Copyright: © 2013 Mishra A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Bouveret syndrome is an uncommon complication of very common disease, gallstones. It refers to gastric outlet due to proximal migration of gallstone through a cholecysto-enteric fistula. Here we describe one such case and a review of literature on this rare disease entity. The case was diagnosed pre operatively using clinico-radiological data and was managed surgically.
Keywords
Gastric outlet obstruction; Gall stone; Intestinal obstruction; Vomiting
Introduction
Bouveret syndrome refers to gastric outlet obstruction caused by the migration of a gallstone through a cholecyst-enteric fistula into the proximal duodenum. It is a very rare phenomenon and has been reported most commonly in elderly female. We present a case of Bouveret syndrome in a middle aged man, who was managed surgically.
Case Report
A 45yrs old Asian male presented to surgical clinic in with complaints of pain right upper abdomen for 5-6 months duration which was gradual, dull aching and associated with occasional episodes of fever. The pain aggrevated for last two days and was associated with fever. There was no history of jaundice, nausea or vomiting. The abdomen was soft, non tender with no palpable organomegaly.
Ultrasonography showed features suggestive of stone in gall bladder. Rest of the organs including the common bile duct was reported normal. Blood investigations were essentially normal. A diagnosis of cholelithiasis with acute or chronic cholecystitis was made and the patient was treated with intravenous antibiotics and an open cholecystectomy was planned after 6 weeks. At operation, a densely adherent mass was encountered with inseparable adhesions between Gall bladder, omentum and duodenum. Biopsy was taken from gall bladder mass and cholecystectomy was abandoned. The patient made uneventful recovery. Biopsy was suggestive of Xanthogranulomatous cholecystitis. It was then decided to allow the dense inflammation to subside and elective surgery was deferred for 4-5 months.
The patient again presented to surgical emergency three months later with complaints of repeated episodes of vomiting increasing in frequency over the past two weeks. The vomitus contained food particles ingested 3-4 hrs back. There was no history of heart burn, heaviness, weight loss and anorexia. Clinically, the patient was dehydrated and showed tachycardia. Abdominal examination revealed a dull fullness in the upper abdomen, with a distinct succusion splash. Rest of the abdomen was soft and non tender.
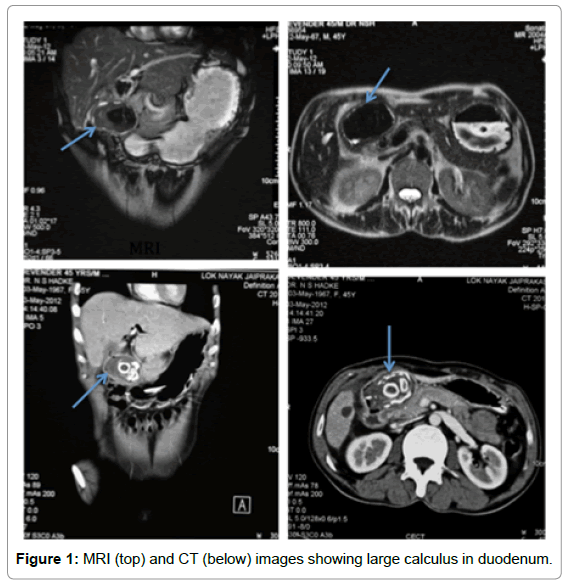
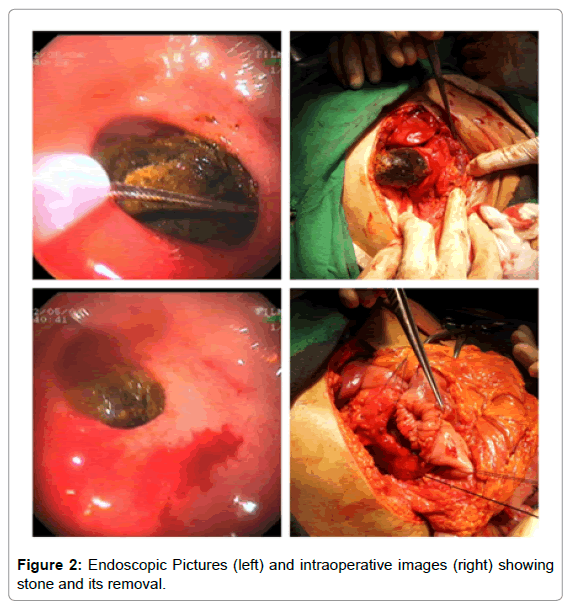
Abdominal X-ray was unremarkable except for a 2×2 cm calcified circular opacity at the level of L2-L 3 (Figure 1). All the Blood investigations and arterial blood gases showed hypokalemia. Rest of the investigation was within normal limits. A clincal diagnosis of gastric outlet obstruction was made and the patient was managed by nasogastric aspiration with correction of dehydration and electrolyte imbalances. Contrast enhanced CT (CECT) showed a distended thick walled gall bladder containing multiple radio opaque calculi with the presence of air within the biliary tree suggestive of pnuemo-bilia (Figure 1). Gastro-duodenoscopy showed a normal stomach and pylorus with a large stone filling the whole lumen of the first part of duodenum preventing any further negotiation of the scope. Retrieval of stone was attempted endoscopically at the same sitting, but was unsuccessful due to massive size of stone limiting any endoscopic manipulation (Figure 2). MRCP confirmed a contracted gall bladder and a large hypointense filling defect in the first part of duodenum with proximal dilation of stomach (Figure 1).
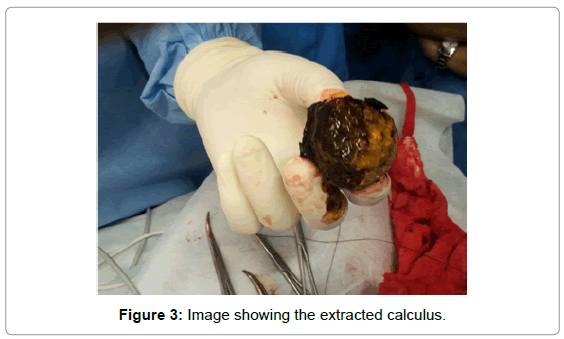
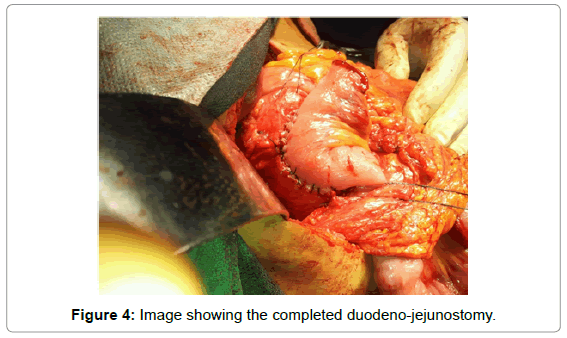
A diagnosis of Bouveret syndrome was made and an open cholecystectomy with surgical removal of the stone was planned. After pre-anaesthetic clearance, patient was taken for surgery. Peritoneum was entered through the previous right subcostal incision. A large 8 cm stone was palpated and confirmed in the first part of the duodenum obliterating and stretching the duodenal wall which was densely adherent to the right lobe of liver and the gall bladder. Gall bladder was shrunken and fibrosed to a size of 3 cm. Anatomy of the Calot’s triangle was obscured due to the fibrosis and inflammation. Only a nibble of gall bladder was visible. An eight cm longitudinal duodenotomy was made overlying the stone in the first part of the duodenum and the stone was extracted from its lumen (Figure 2). Duodenum was thick walled with leathery mucosa. The duodenotomy was closed with a Roux en Y duodeno-jejunostomy in two layers (Figure 2). The patient made uneventful recovery and was discharged on the 7th day and is doing well at present.
Discussion and Review
While the majority of patients with gallstones do well, a small percentage of patients (approximately 6%) develop complications including such rare complications as cholecystoduodenal fistulas [1]. Fistula formation is thought to occur as a result of adhesions between the gallbladder and the bowel wall from chronic inflammation, impaired arterial blood supply and decreased venous drainage [2]. Ensuing fistula formation can occur from pressure necrosis and compression of a gallstone against the gallbladder wall, and subsequent passage of gallstones via the fistula can then result in gallstone ileus [3].
Gallstone ileus, although rare is an important cause of mechanical intestinal obstruction. Migration of a gallstone occurs through a cholecystenteric fistula to the distal ileum leads to impaction of the stone and subsequent symptoms of intestinal obstruction. Although gallstone ileus is a cause of only 14% of intestinal obstructions in the general population, the incidence increases in the elderly accounting for 25% of nonstrangulated small bowel obstructions [4]. Females are affected up to six times more often than males. The site of obstruction is most commonly the terminal ileum (50-70%), where the small bowel is at its narrowest. Less common locations of impaction include the distal jejunum (9%), the colon (4%), the rectum (4%), and the duodenum (1-3%) [4].
In contrast to gallstone ileus where stone moves distally along peristalsis, Bouveret syndrome is characterized by the cephalad or proximal migration of a gallstone into the duodenum resulting in a gastric outlet obstruction. The syndrome was first described by Beaussier in 1770 and was subsequently named after the French physician Leon Bouveret after he published two case reports in Revue de Medecin in 1896 [5].
Bouveret syndrome accounts for 1-3% of duodenal obstruction cases [4]. As in gallstone ileus, there is a higher incidence of the disease in women than in men, [6] with a female-to-male sex ratio of 1.86. It is also a disease of the elderly with a mean age of 74.1 [+ or -] 11.1 (SD) years [6].
The clinical presentation of Bouveret’s syndrome is usually nonspecific and rarely diagnostic, most common symptoms being nausea and vomiting (86%), and abdominal pain (71%). Less commonly, patients can present with hematemesis, weight loss, and anorexia [6]. Physical examination usually reveals abdominal tenderness, abdominal distention, and dehydration. Gastro-duodenoscopy is of great help in making the diagnosis of Bouveret’s syndrome. In about 69% of patients the stone and fistula is visualized obstructing duodenal lumen [6]. However in the remaining cases, the stone may not actually be visualized because it is compressing the lumen and only partially visualized through the duodenal wall. Other endoscopic findings described include excessive retained food or fluid in the stomach and inflammation, edema, or ulcer at the impacted site [7]. Radiologic imaging tests can often confirm the diagnosis of Bouveret’s syndrome. X-rays may pick calcified gallstones and also shows features of gastric outlet obstruction. CT usually identifies the presence of the duodenal fistula but its role in identifying the stone is limited as 15-25% of gallstones is attenuating and not well visualized on CT. In such cases, magnetic resonance cholangiopancreatography (MRCP) may be useful, because it more clearly delineates fluid from calculi.
Various modalities including surgical and endoscopic managements have been successfully tried for management of obstruction due to gall stone. For more proximal gallstone obstruction Endoscopic extraction, endoscopic laser lithotripsy (ILL), extracorporeal shockwave lithotripsy (ESWL), and intracorporeal electrohydraulic lithotripsy (IEHL) have all been recommended whereas surgery is routinely advised for individuals with impaction of the gallstone more distally (gallstone ileus).
Extracorporeal shockwave lithotripsy (ESWL) has also been used with success in treating patients with Bouveret’s syndrome [8]. Limitations of using ESWL include the need for several return sessions, in addition to eventual endoscopy. Also, ESWL may be difficult to perform in obese patients or if there are gas-containing bowel loops interposed between the gallstone and the abdominal wall [8].
The first successful endoscopic extraction was described in 1985 by Bedogni et al. [9]. Endoscopic management can be technically challenging, time-consuming, and success rates in case series have been previously reportedly to be less than 10% [10]. The results of Endoscopic treatment are better when it is adducted with lithotripsy. The drawbacks of lithotripsy procedures are the need for prolonged and multiple sessions, and the risk of converting a proximal gallstone ileus into a distal gallstone ileus (as a result of partial fragmentation of the stone). Also inadvertent focusing of the shockwaves onto the intestine wall may cause bleeding and perforation. In general, the success rate of endoscopic extraction is dependent on stone size. Stones, that are larger than 2.5 cm are more difficult to extract endoscopically. Larger stones can cause ischemic ulceration of the adjacent duodenal wall. Moreover, these stones tend to have a hard outer shell and soft inner core making mechanical fragmentation with endoscopic forceps or laser more difficult. Another complication reported is that of pulse less electrical activity (PEA) during mechanical retrieval due to the gallstone getting lodged in the esophagus; the PEA abruptly resolved when the stone was pushed back into the stomach.
Most of the cases will eventually need surgery for either failed endoscopic procedures or complications arising due to the procedures like stricture, sepsis, and residual stone in the duodenum [11]. Surgical options include a combination of enterolithotomy (removal of the stone) plus cholecystectomy and fistula repair, Laparoscopy is also an additional option for surgical treatment; Sica et al. reported, in 2005, the first case of uneventful stone removal and cholecystectomy by laparoscopy [12]. But presence of edematous duodenal mucosa as in this case makes repair of duodenal defect difficult. Such defects can be easily closed by performing Roux-en-Y doudeno-jejunostomy (Figures 3 and 4).
References
- LeBlanc KA, Barr LH, Rush BM (1983) Spontaneous biliary enteric fistulas. South Med J 76: 1249-1252.
- Langhorst J, Schumacher B, Deselaers T, Neuhaus H (2000) Successful endoscopic therapy of a gastric outlet obstruction due to a gallstone with intracorporeal laser lithotripsy: a case of Bouveret's syndrome. Gastrointest Endosc 51: 209-213.
- Pickhardt PJ, Friedland JA, Hruza DS, Fisher AJ (2003) Case report. CT, MR cholangiopancreatography, and endoscopy findings in Bouveret's syndrome. AJR Am J Roentgenol 180: 1033-1035.
- Reisner RM, Cohen JR (1994) Gallstone ileus: a review of 1001 reported cases. Am Surg 60: 441-446.
- Bouveret L (1896) Stenose du pylore adherent a la vesicule. Revue Medicale Paris.
- Bateson MC (1984) Gallbladder disease and cholecystectomy rate are independently variable. Lancet 2: 621-624.
- Cappell MS, Davis M (2006) Characterization of Bouveret's syndrome: a comprehensive review of 128 cases. Am J Gastroenterol 101: 2139-2146.
- Dumonceau JM, Delhaye M, Devière J, Baize M, Cremer M (1997) Endoscopic treatment of gastric outlet obstruction caused by a gallstone (Bouveret's syndrome) after extracorporeal shock-wave lithotripsy. Endoscopy 29: 319-321.
- Bedogni G, Contini S, Meinero M, Pedrazzoli C, Piccinini GC (1985) Pyloroduodenal obstruction due to a biliary stone (Bouveret's syndrome) managed by endoscopic extraction. Gastrointest Endosc 31: 36-38.
- Lowe AS, Stephenson S, Kay CL, May J (2005) Duodenal obstruction by gallstones (Bouveret's syndrome): a review of the literature. Endoscopy 37: 82-87.
- Moschos J, Pilpilidis I, Antonopoulos Z, Paikos D, Tzilves D, et al. (2005) Complicated endoscopic management of Bouveret's syndrome. A case report and review. Rom J Gastroenterol 14: 75-77.
- Sica GS, Sileri P, Gaspari AL (2005) Laparoscopic treatment of Bouveret's syndrome presenting as acute pancreatitis. JSLS 9: 472-475.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14142
- [From(publication date):
October-2013 - May 27, 2024] - Breakdown by view type
- HTML page views : 9775
- PDF downloads : 4367