Published online Jun 26, 2023. doi: 10.4330/wjc.v15.i6.309
Peer-review started: December 9, 2022
First decision: March 15, 2023
Revised: March 30, 2023
Accepted: May 19, 2023
Article in press: May 19, 2023
Published online: June 26, 2023
ST-elevation myocardial infarction (STEMI) is the result of transmural ischemia of the myo
To determine the incidence of fibrinolytic therapy during the COVID-19 pandemic and its effects on STEMI clinical outcomes.
PubMed, Google Scholar, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials were queried from January 2020 up to February 2022 to identify studies investigating the effect of fibrinolytic therapy on the prognostic outcome of STEMI patients during the pandemic. Primary outcomes were the incidence of fibrinolysis and the risk of all-cause mortality. Data were meta-analyzed using the random effects model to derive odds ratios (OR) and 95% confidence intervals. Quality assessment was carried out using the Newcastle-Ottawa scale.
Fourteen studies including 50136 STEMI patients (n = 15142 in the pandemic arm; n = 34994 in the pre-pandemic arm) were included. The mean age was 61 years; 79% were male, 27% had type 2 diabetes, and 47% were smokers. Compared with the pre-pandemic period, there was a significantly increased overall incidence of fibrinolysis during the pandemic period [OR: 1.80 (1.18 to 2.75); I2= 78%; P = 0.00; GRADE: Very low]. The incidence of fibrinolysis was not associated with the risk of all-cause mortality in any setting. The countries with a low-and middle-income status reported a higher incidence of fibrinolysis [OR: 5.16 (2.18 to 12.22); I2 = 81%; P = 0.00; GRADE: Very low] and an increased risk of all-cause mortality in STEMI patients [OR: 1.16 (1.03 to 1.30); I2 = 0%; P = 0.01; GRADE: Very low]. Meta-regression analysis showed a positive correlation of hyperlipidemia (P = 0.001) and hypertension (P < 0.001) with all-cause mortality.
There is an increased incidence of fibrinolysis during the pandemic period, but it has no effect on the risk of all-cause mortality. The low- and middle-income status has a significant impact on the all-cause mortality rate and the incidence of fibrinolysis.
Core Tip: The guideline-recommended time goals for primary percutaneous coronary intervention (PPCI) could not be met during the coronavirus disease 2019 (COVID-19) pandemic for the treatment of ST-elevation myocardial infarction (STEMI) patients. Leading cardiology societies recommended considering a new fibrinolytic-based reperfusion strategy during the time of the COVID-19 pandemic; however, previous large-scale studies have indicated that fibrinolytic therapy may offer a reduced prognostic value and poor survival outcomes in patients with STEMI compared to PPCI. We investigated the differential prevalence of the use of fibrinolytic therapy by healthcare systems belonging to countries with distinct income status, and its effect on the risk of all-cause mortality in STEMI patients.
- Citation: Khedr A, Hennawi HA, Khan MK, Elbanna M, Jama AB, Proskuriakova E, Mushtaq H, Mir M, Boike S, Rauf I, Eissa A, Urtecho M, Koritala T, Jain N, Goyal L, Surani S, Khan SA. Effect of fibrinolytic therapy on ST-elevation myocardial infarction clinical outcomes during the COVID-19 pandemic: A systematic review and meta-analysis. World J Cardiol 2023; 15(6): 309-323
- URL: https://www.wjgnet.com/1949-8462/full/v15/i6/309.htm
- DOI: https://dx.doi.org/10.4330/wjc.v15.i6.309
ST-elevation myocardial infarction (STEMI) is a severe form of coronary artery disease caused by tra
The preferred treatment for STEMI is primary percutaneous coronary intervention (PPCI)[3]. However, the coronavirus disease 2019 (COVID-19) pandemic placed a significant strain on healthcare resources and providers, leading some experts to recommend changes in STEMI management. Fibrinolytic therapy was suggested as an alternative treatment for patients with severe resource limitations, a shortage of personal protective equipment, low-risk STEMI, systems of care delays, and the inability to provide PPCI in a timely fashion[4-8]. In a recent systematic review and meta-analysis conducted by Kamarullah and colleagues, it was found that the performance of STEMI care declined and clinical outcomes deteriorated in STEMI patients during the COVID-19 pandemic[9]. Despite this, the impact of fibrinolytic therapy on clinical outcomes during the pandemic remains largely unknown.
Therefore, the aim of this systematic review is to examine the significance of the increase in fibrinolytic therapy in adult STEMI patients during the COVID-19 pandemic compared to the pre-COVID-19 era, and to assess the impact of this treatment strategy on clinical outcomes, particularly the risk of all-cause mortality, in comparison to patients who received standard-care before or during the pandemic.
To ensure transparent reporting, this systematic review and meta-analysis follow the PRISMA guide
PubMed, Google Scholar, Scopus, Web of Science, and Cochrane Central Register of Controlled Trials were searched systematically for articles in the English language between the time when severe acute respiratory syndrome coronavirus 2 was declared a Public Health emergency of international concern-PHIEC (January 2020) up until February 2022. We used the following keywords: STEMI, fibrinolysis, and COVID-19. We utilized minimum keywords to maximize the initial scope of research in order to ensure the largest number of articles recorded. Complete search strategies used for all electronic databases were developed by an experienced librarian and are reported in the Supplementary material. Reference mining included scanning reference lists of relevant papers, included studies, and systematic reviews published during the analysis of literature.
Our study population consisted of patients with confirmed STEMI. We included studies that reported the impact of the COVID-19 pandemic on STEMI care. We searched for clinical trials, cohort studies, case-control studies, and case series. Animal studies, expert opinions, literature reviews, news articles, letters, editorials, case reports, guidelines, and any studies that did not mention the timing, population, intervention, and outcomes of interest were excluded.
We imported articles retrieved from the systematic search and exported them to EndNote reference library software (Thomson Reuters), where duplicates were identified and removed. Initially, articles were screened based on titles and abstracts by two independent reviewers (H.A.H. and E.P), then filtered relevant articles underwent full-text screening by another two reviewers working independently (H.A.M. and A.B.J). Another reviewer (A.K.) was consulted for decisions regarding any discrepancies during screening.
Data were extracted in a standardized data extraction form. We extracted data related to the following: (1) Summary of the included studies: Authors, year, timing, country, study design, sample size, inclusion criteria, duration of symptoms to intervention, study arms, and duration of follow up; (2) baseline characteristics of the included patients for regression purpose: Age, gender, race, body mass index, comorbidities, smoking status, and type of STEMI; and (3) the study outcomes as stated below. Any disagreements during data extraction were discussed to reach a consensus.
The Newcastle–Ottawa Scale for observational studies was used by two independent reviewers (M.E. and M.K.K.) to evaluate quality on three diverse characteristics: Selection of study groups, comparability of groups, and ascertainment of the outcome of interest[12]. Each article was given a score that indicated how biased it was. Studies with a total score of seven or above were regarded to have a minimal probability of bias. If a study had a total score of six or less, it was determined to have a significant risk of bias. Disagreements in quality ratings were solved by a third reviewer (A.K.).
We included studies that reported the incidence of the use of fibrinolytic therapy for STEMI patients during the pandemic compared to the timeline before the pandemic. The primary outcomes were the incidence of fibrinolysis and all-cause mortality.
The analysis was performed in a sequence of calculations; the odds ratio (OR) of the incidence of fibrinolysis was calculated, followed by the subgrouping of studies based on significant increase in the incidence of fibrinolysis, no change in the incidence of fibrinolysis, and economic status of the countries where the studies were carried out, respecting the World Bank’s classification of developed and developing countries into high-income and low- and middle-income countries (HICs and LMICs), respectively[13]. The effect sizes and the corresponding 95% confidence intervals (CIs) were calculated from raw data and variability measures or extracted directly from the studies. The outcomes were calculated using the DerSimonian and Laird random-effects model. The Higgin I2 test was used to evaluate the heterogeneity between studies, and higher percentages indicated higher heterogeneity. The summation effect measures were calculated as OR with 95%CIs. Statistical significance was set at < 0.05 for all calculations.
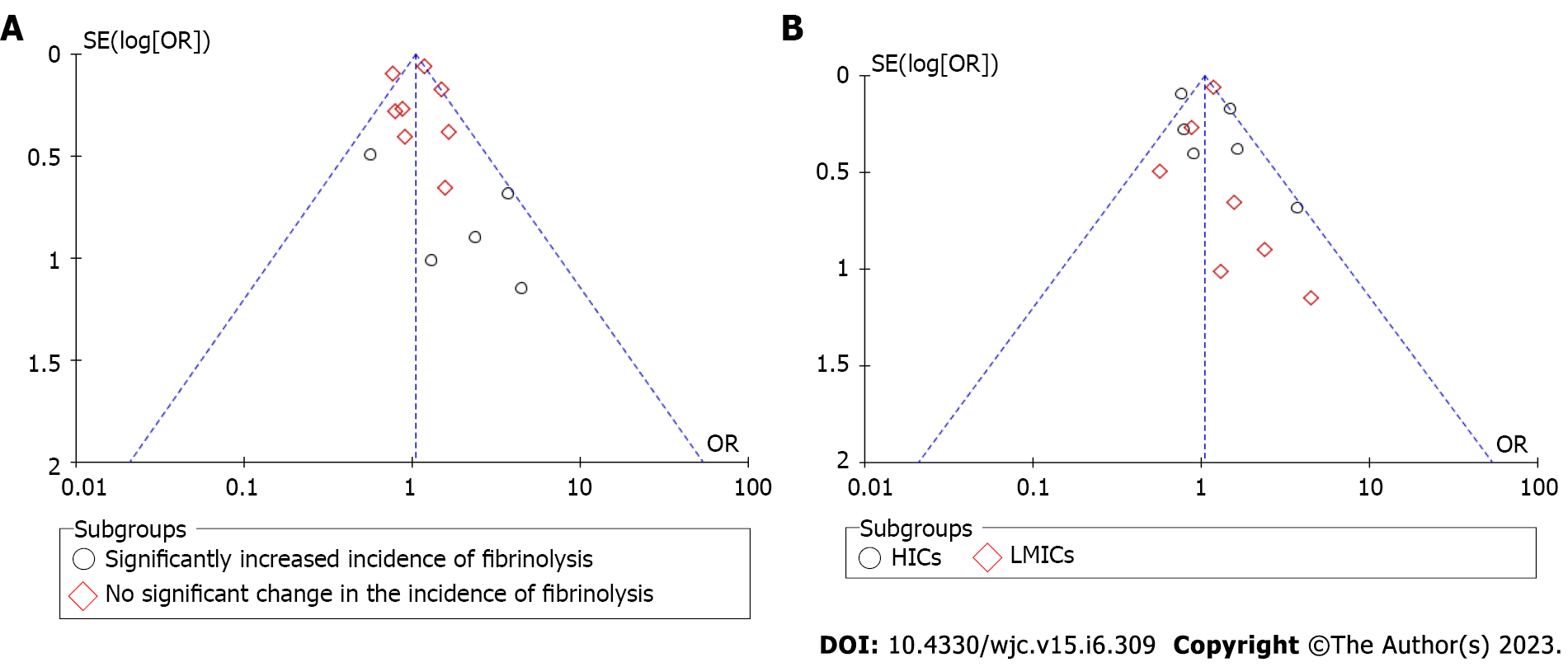
Publication bias was assessed using the Begg funnel plot test[14]. Sensitivity analysis was performed by adding and removing studies one after another. Meta-regression analysis was executed for all-cause mortality. Two covariates having significant correlation among all the tested ones were displayed in the results. MetaXL version 5.3 (Epigear) add-on for Microsoft Excel 365 and Review Manager 5.4 was used to perform all analyzes. The statistical methods of the study were reviewed by a biomedical statistician.
A summary of estimated effects and the certainty of each piece of evidence was produced using the GRADE approach (Supplementary Table 1). The GRADE criteria categorize the certainty of evidence as High, Moderate, Low, and Very low. The rating process followed the GRADE manual. GRADEpro GDT was used to construct the certainty of evidence and the summary of findings table.
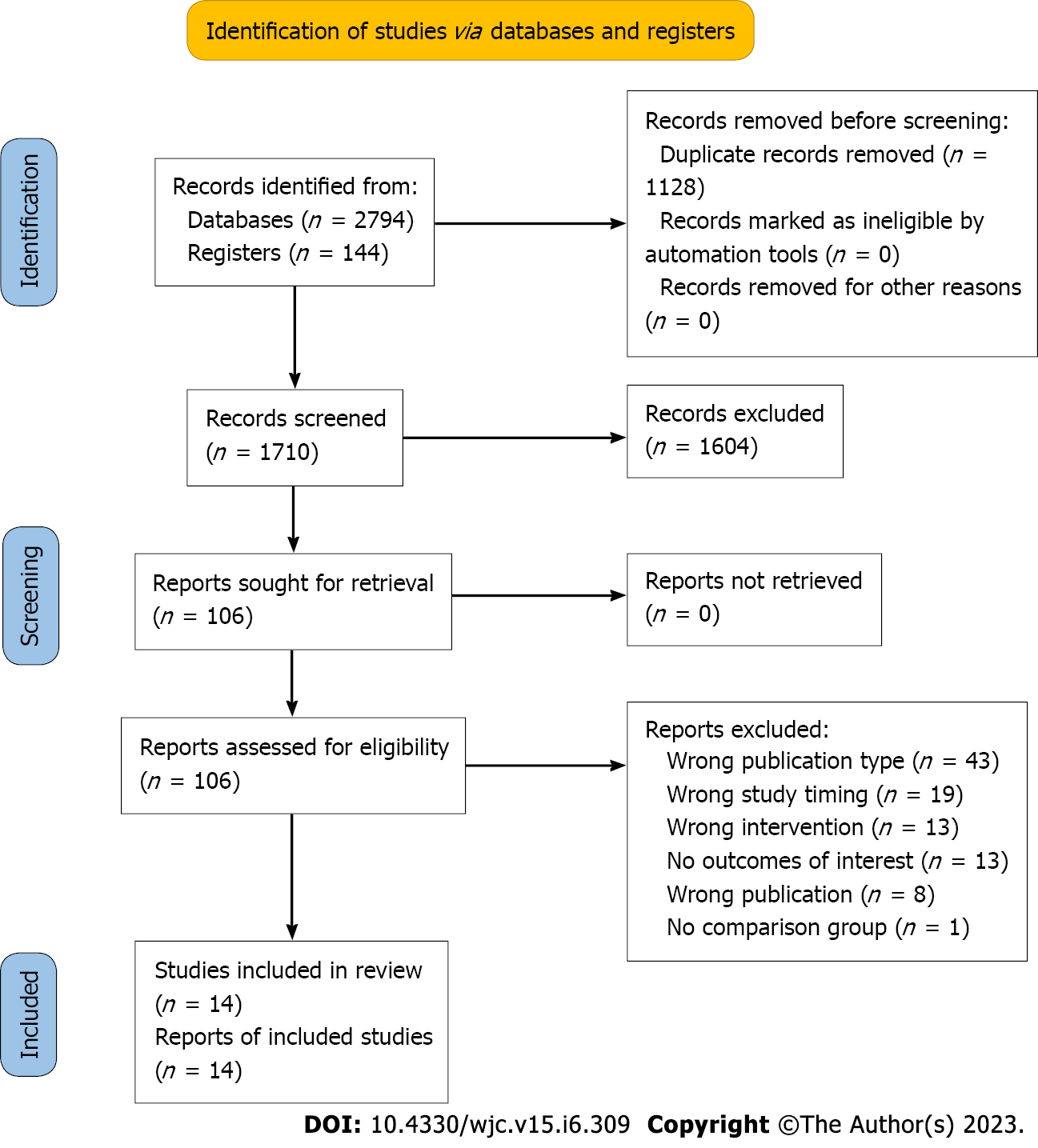
The process of study selection and the characteristics of the included studies are summarized in Figure 1 and Tables 1 and 2, respectively. A total of 2938 studies were initially identified through database searches, and after removing duplicates, 14 studies were found to be eligible for inclusion in this meta-analysis[15-28]. These studies involved 50136 adult STEMI patients, with 15142 patients receiving fibrinolytic therapy during the pandemic era and 34994 patients receiving standard of care before or during the pre-pandemic era. Our meta-analysis assessed the impact of fibrinolytic therapy on clinical outcomes, particularly the risk of all-cause mortality, in comparison to standard-care before or during the pandemic.
| Ref. | Country | Study design/Sa | Study group/time period of study / sample size |
| Daoulah et al[15] | Saudi Arabia | Retrospective Cohort/500 | Pandemic period STEMI/01/01/2020–30/04/2020/500 |
| Pre-pandemic period STEMI/2018–2019/1285 | |||
| Leng et al[16] | China | Retrospective Cohort | Pandemic period STEMI/23/01/2020–30/04/2020/164 |
| Pre-pandemic period STEMI/Equivalent period in 2019/240 | |||
| Song et al[17] | China | Retrospective Cohort | Pandemic period STEMI/24/01/2020–31/03/2020/73 |
| Pre-pandemic period STEMI/24/01/2019–31/03/2019/95 | |||
| Wang et al[18] | China | Retrospective Cohort | Pandemic period STEMI/23/01/2020–20/03/2020/37 |
| Pre-pandemic period STEMI/01/09/2019–02/12/2019/41 | |||
| Wu et al[19] | England | Retrospective Cohort | Pandemic period STEMI/01/01/2019/1600 |
| Pre-pandemic period STEMI/22/05/2020/15646 | |||
| Xiang et al[20] | China | Retrospective Cohort | Pandemic period STEMI/20/02/2020/10516 |
| Pre-pandemic period STEMI/27/12/2019/14634 | |||
| Zhang et al[21] | China | Retrospective Cohort | Pandemic period STEMI/01/01/2020–31/03/2020/119 |
| Pre-pandemic period STEMI/2018 and 2019/276 | |||
| Huang et al[22] | China | Retrospective Cohort | Pandemic period STEMI/01/02/2020–15/04/2020/31 |
| Pre-pandemic period STEMI/01/01/2019–31/12/2019/31 | |||
| Erol et al[23] | Turkey | Retrospective Cohort | Pandemic period STEMI/2020/485 |
| Pre-pandemic period STEMI/2018/711 | |||
| Mesnier et al[24] | France | Retrospective Cohort | Pandemic period STEMI/16/03/2020–12/02/2020/252 |
| Pre-pandemic period STEMI/17/02/2020–15/03/2020/331 | |||
| Balghith[25] | Saudi Arabia | Retrospective Cohort | Pandemic period STEMI/01/2020–05/2020/81 |
| Pre-pandemic period STEMI/08/2019-12/2019/92 | |||
| Clifford et al[26] | Canada | Retrospective Cohort | Pandemic period STEMI/17/03/2020–16/07/2020/193 |
| Pre-pandemic period STEMI/15/11/2019–16/03/2020/238 | |||
| Rodríguez-Leor et al[27] | Spain | Retrospective Cohort | Pandemic period STEMI/16/03/2020–14/04/2020/1009 |
| Pre-pandemic period STEMI/01/04/2019–30/04/2019/1305 | |||
| Calvão et al[28] | Portugal | Retrospective Cohort | Pandemic period STEMI/03/2020–04/2020/71 |
| Pre-pandemic period STEMI/03/2020–04/2020/80 |
| Ref. | Study group | Age, years (SD) | Male, n (%) | Hypertension, n (%) | Diabetes mellitus, n (%) | Hyperlipidemia, n (%) | Smoking, n (%) |
| Daoulah et al[15] | Pandemic period STEMI | 55.4 (11.8) | 454 (90.8) | 229 (46.7) | 257 (52.1) | 190 (38.9) | 213 (43) |
| Pre-pandemic period STEMI | 56.5 (12.8) | 1123 (87.5) | 599 (47.6) | 632 (50.4) | 450 (35.8) | 318 (41.6) | |
| Leng et al[16] | Pandemic period STEMI | 63.13 (13.6) | 131 (79.9) | N/A | N/A | N/A | N/A |
| Pre-pandemic period STEMI | 62.21 (13.14) | 178 (73.9) | N/A | N/A | N/A | N/A | |
| Song et al[17] | Pandemic period STEMI | 61.6 (13.1) | 59 (80.82) | 43 (58.9) | 16 (21.9) | 39 (53.4) | 36 (49.3) |
| Pre-pandemic period STEMI | 60.6 (13.9) | 68 (71.57) | 56 (59) | 22 (23.2) | 51 (53.7) | 55 (57.9) | |
| Wang et al[18] | Pandemic period STEMI | 59.29 (11.46) | 33 (89.18) | 20 (54.05) | 6 (16.21) | 13 (35.13) | 37 (100) |
| Pre-pandemic period STEMI | 55.49 (11.89) | 35 (85.36) | 18 (43.90) | 5 (12.19) | 15 (36.58) | 31 (75.60) | |
| Wu et al[19] | Pandemic period STEMI | 65.1 (13.6) | 1181 (73.81) | 581 (36.31) | 309 (19.31) | 368 (23) | 450 (28.12) |
| Pre-pandemic period STEMI | 65.76 (13.44) | 11263 (71.98) | 6060 (38.73) | 3005 (19.20) | 3645 (23.29) | 4704 (30.06) | |
| Xiang et al[20] | Pandemic period STEMI | 61.59 (13.10) | 7986 (75.94) | N/A | N/A | N/A | N/A |
| Pre-pandemic period STEMI | 62.86 (12.33) | 11019 (75.29) | N/A | N/A | N/A | N/A | |
| Zhang et al[21] | Pandemic period STEMI | N/A | N/A | N/A | N/A | N/A | N/A |
| Pre-pandemic period STEMI | N/A | N/A | N/A | N/A | N/A | N/A | |
| Huang et al[22] | Pandemic period STEMI | 61 | 25 (80.6) | 16 (51.6) | 8 (25.8) | 7 (22.6) | 18 (58.1) |
| Pre-pandemic period STEMI | 60 | 25 (80.6) | 18 (58.1) | 6 (19.4) | 8 (25.8) | 20 (64.5) | |
| Erol et al[23] | Pandemic period STEMI | 59 (13) | 552 (77.63) | 221 (45.56) | 151 (31.13) | 108 (22.26) | 248 (50.30) |
| Pre-pandemic period STEMI | 60 (14) | 387 (79.79) | 273 (38.39) | 201 (28.27) | 67 (9.4) | 401 (56.39) | |
| Mesnier et al[24] | Pandemic period STEMI | 63.4 (12.5) | 357 (74) | 116 (24.11) | 35 (7.27) | N/A | 96 (19.95) |
| Pre-pandemic period STEMI | 64.4 (13.6) | 509 (74) | 139 (20.26) | 55 (8.01) | N/A | 131 (19.09) | |
| Balghith[25] | Pandemic period STEMI | 57.2 (12.6) | 83 (90.21) | 44 (54.32) | 45 (48.91) | 36 (39.13) | 41 (44.56) |
| Pre-pandemic period STEMI | 51.3 (11.5) | 81 (100) | 38 (41.3) | 41 (44.56) | 31 (33.69) | 35 (38.04) | |
| Clifford et al[26] | Pandemic period STEMI | 65 (12) | 169 (71) | 99 (51.29) | 55 (28.49) | 86 (44.55) | 53 (27.46) |
| Pre-pandemic period STEMI | 64 (13) | 135 (70) | 123 (51.68) | 54 (22.68) | 99 (41.5) | 93 (39.07) | |
| Rodríguez-Leor et al[27] | Pandemic period STEMI | 63.1 (12.5) | 786 (78.4) | 520 (51.9) | 226 (22.6) | 466 (46.7) | 442 (44.6) |
| Pre-pandemic period STEMI | 63.7 (13.2) | 1023 (78.4) | 647 (50) | 224 (25.2) | 592 (45.8) | 581 (45.7) | |
| Calvão et al[28] | Pandemic period STEMI | 63.3 (12.7) | 56 (78.9) | 49 (69.01) | 23 (32.39) | 38 (53.52) | 40 (56.33) |
| Pre-pandemic period STEMI | 65.7 (12.8) | 60 (75) | 48 (60) | 26 (32.5) | 49 (57.5) | 39 (48.75) |
To assess the quality of the included studies, we used the Newcastle-Ottawa Scale for observational studies. Out of the 14 included studies, two were cohort studies, while the remaining 12 were case-control studies. Five studies had a low risk of bias (total score: 7-9), while the remaining studies were found to have a moderate risk of bias (total score: 4-6). None of the included studies had a high risk of bias (total score: 0-3). The detailed quality assessment of each study is provided in the (Supple
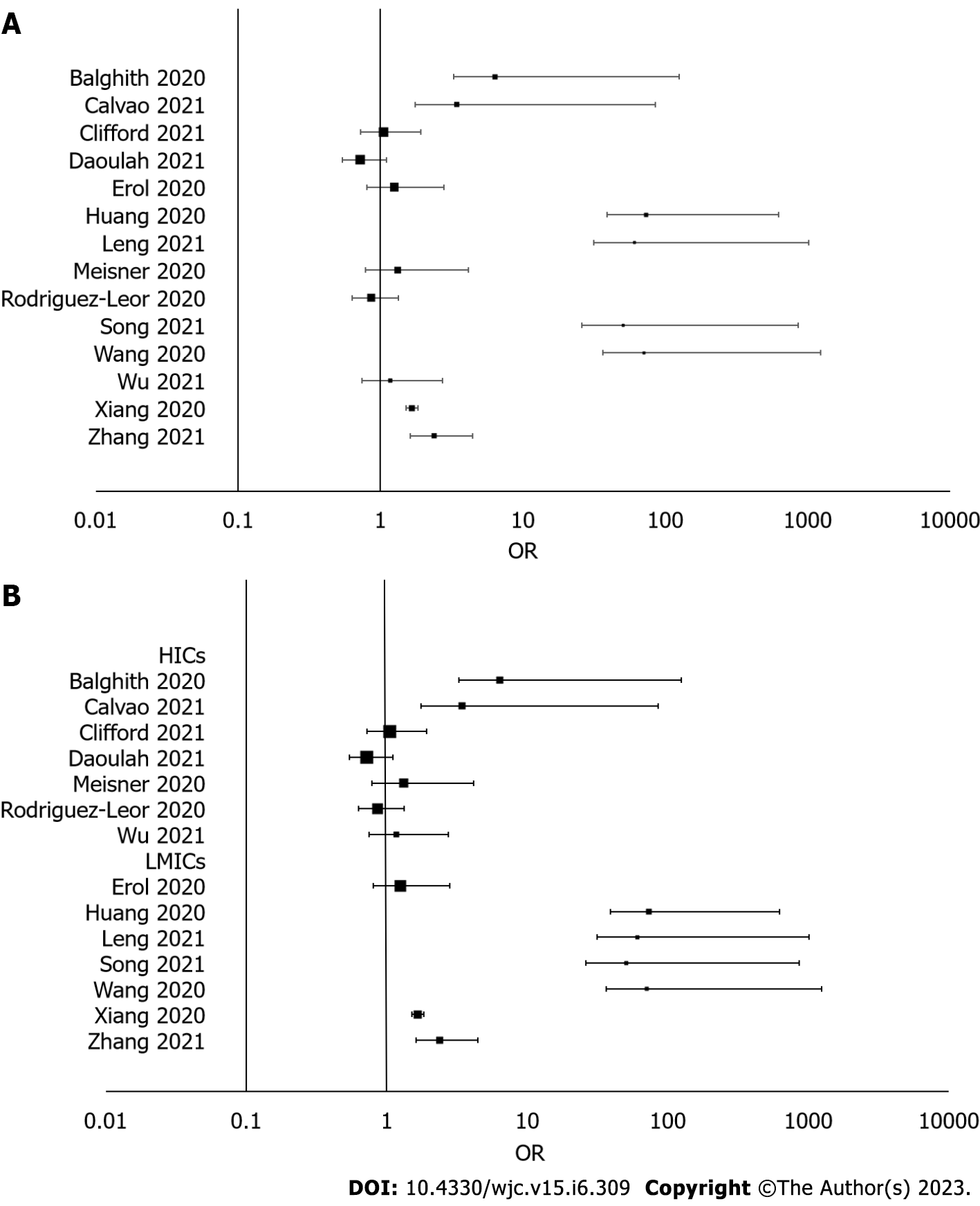
All 14 studies included in this meta-analysis investigated the frequency of fibrinolytic therapy in adult STEMI patients during the COVID-19 pandemic compared to the pre-pandemic era. Our analysis revealed a significantly higher incidence of fibrinolytic therapy during the pandemic [OR: 1.80 (95%CI: 1.18-2.75); I2 = 78%; P = 0.00; GRADE: Very low] (Figure 3A). Moreover, we observed that patients treated in LMICs had a higher probability of receiving fibrinolytic therapy [OR: 5.16 (95%CI: 2.18-12.22); I2 = 81%; P = 0.00; GRADE: Very low] (Figure 3B).
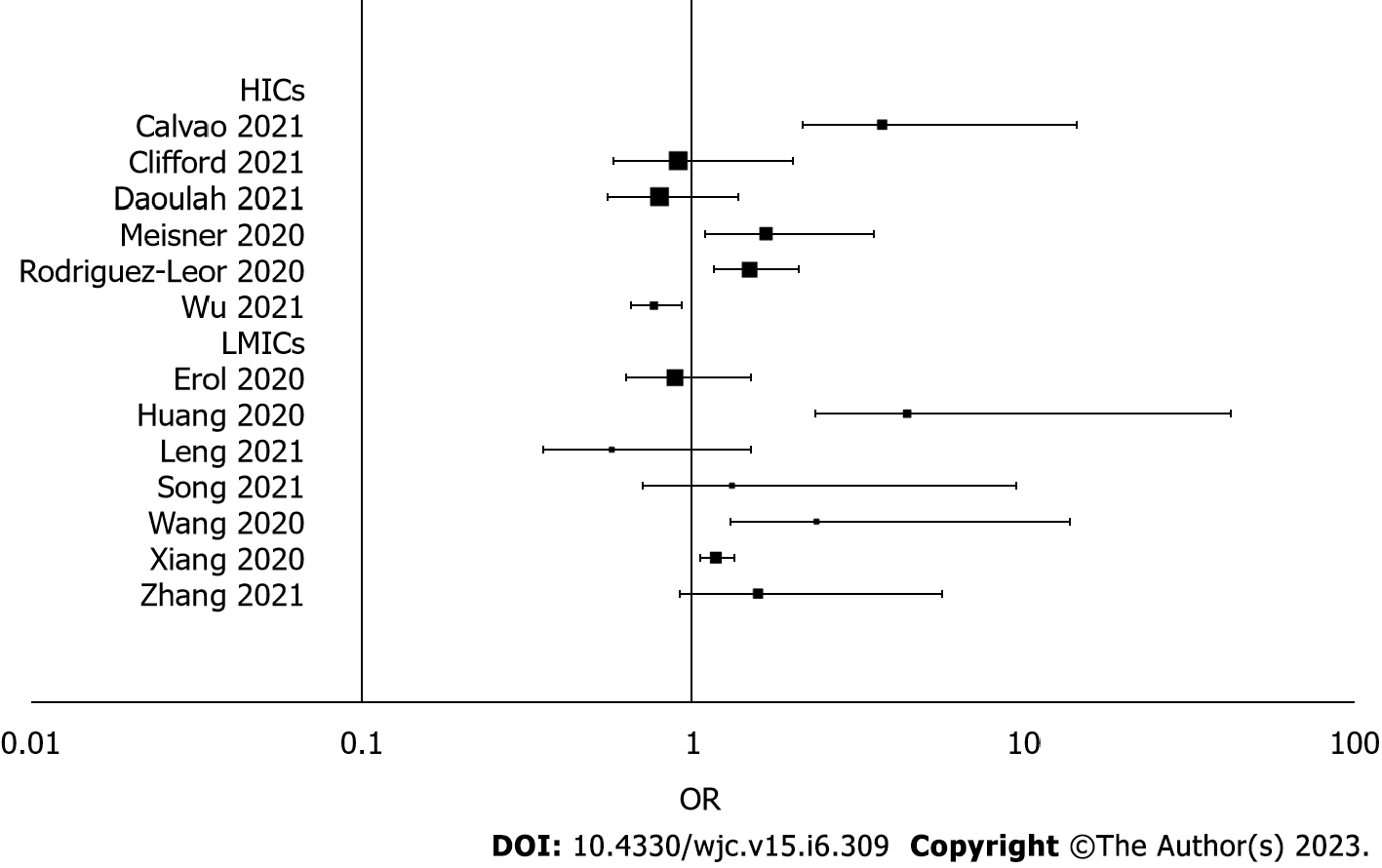
We evaluated all-cause mortality in 13 of the included studies. The increased incidence of fibrinolytic therapy was not found to be associated with an increased risk of all-cause mortality [OR: 1.65 (95%CI: 0.67-4.06); I2 = 40%; P = 0.27; GRADE: Very low] (Figure 4). However, patients who received fibrinolytic therapy in LMICs were at a higher risk of all-cause mortality [OR: 1.16 (95%CI: 1.03-1.30); I2 = 0%; P = 0.01; GRADE: Very low]. Overall, we found no significant association between the all-cause mortality rate and the incidence of fibrinolytic therapy [OR: 1.09 (95%CI: 0.87-1.37); I2 = 58%; P = 0.47; GRADE: Very low] (Figure 5).
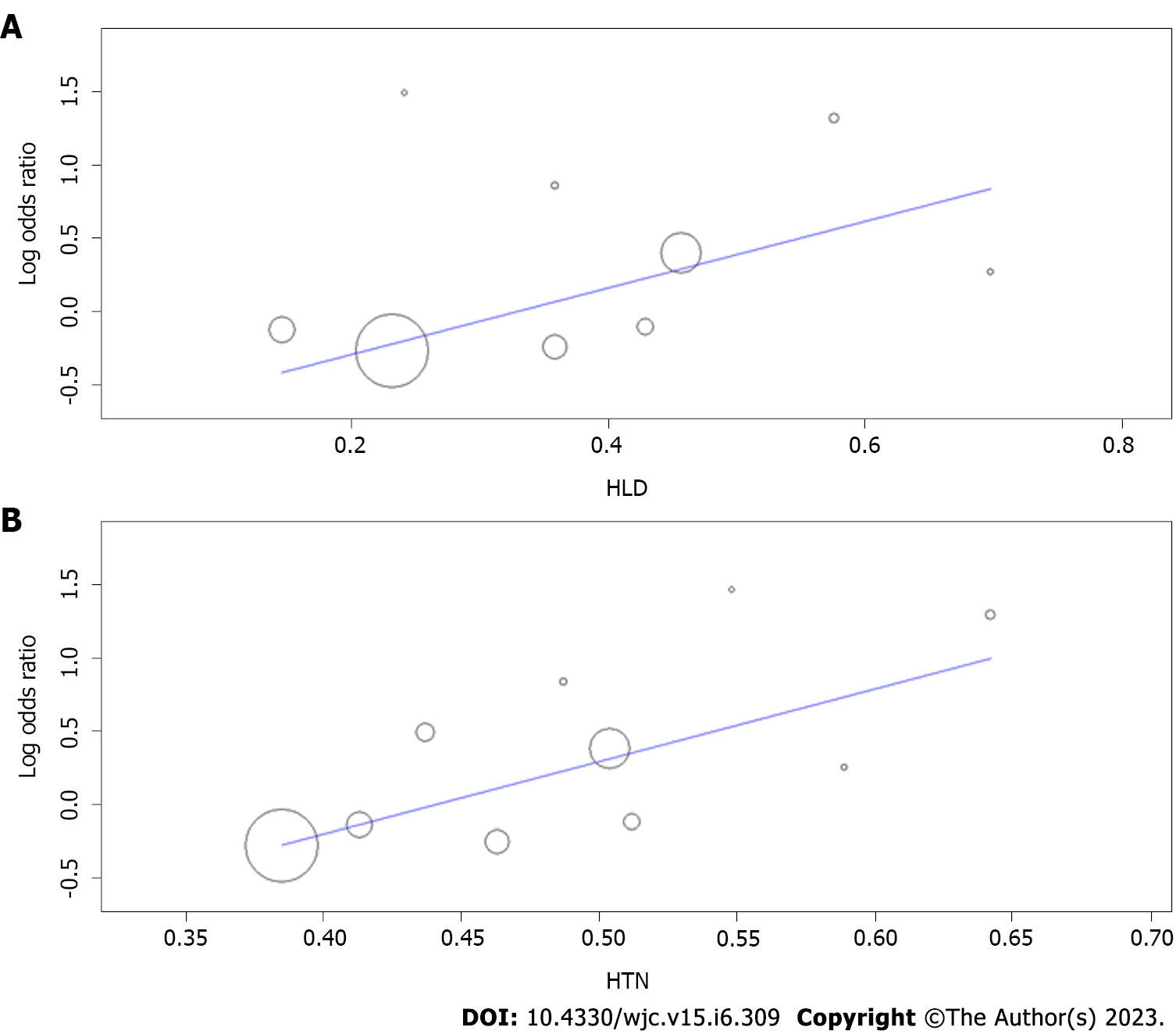
Meta-regression of heterogeneity was performed for the outcome of all-cause mortality, as it is one of our primary outcomes and more clinically relevant. Hyperlipidemia (reported in 9 studies[15,17-19,22,23,24-28]) and hypertension (reported in 10 studies[15,17-19,22-28]) were tested as covariates. The meta-regression analysis provide evidence that hyperlipidemia is associated with an increased risk of all-cause mortality (P = 0.001) (Figure 6A). The meta-regression analysis further revealed that hypertension is also a significant predictor of all-cause mortality (P < 0.001) (Figure 6B). These findings suggest that managing hyperlipidemia and hypertension may be crucial for reducing the risk of all-cause mortality.
After conducting a thorough meta-analysis, we observed a significant increase in the use of fibrinolytic reperfusion in STEMI cases during the COVID-19 pandemic. Interestingly, we found no significant association between fibrinolysis and all-cause mortality rates. However, our analysis revealed that countries with lower-middle-income and low-income status reported a higher incidence of fibrinolysis, which in turn was associated with an elevated risk of all-cause mortality for STEMI patients.
In our meta-regression analysis, we found out that patients having hyperlipidemia and hypertension tend have an increased risk of all-cause mortality. Hyperlipidemia decreases the stability of plaques that are most likely to rupture and decreases endothelial function[29]. It also promotes the formation of platelet thromboses at the site of the injury[30]. LIPID trial also showed a decrease in the risk of mortality for those patients who were treated for hypercholesteremia with the help of Statins therapy[31]. hypertension is also a crucial prognostic factor for STEMI. Hypertension reduces the elastic ability of blood vessels and causes atherosclerosis[32].
The COVID-19 pandemic has added to the already existing challenges of chronically strained healthcare systems worldwide. Among the many areas of healthcare that have been impacted, primary cardiac interventions for STEMI patients have also faced significant obstacles[33]. In high-income countries, meeting the recommended time goals for such interventions was difficult even before the pandemic, with only 25%-50% of patients receiving PPCI within the recommended time frame of 120 minutes from first medical contact (FMC) to balloon[34]. Unfortunately, the pandemic has further exacerbated delays in symptoms-to-FMC and door-to-balloon time, creating an additional challenge for healthcare systems to provide timely and effective care to STEMI patients. A study reported that the mean time from symptoms to intervention was longer during the COVID-19 pandemic compared to the previous year[35]. The need to screen for COVID-19, which includes procedures such as chest radio
The response to the COVID-19 pandemic has been rapidly evolving and may differ between countries based on their ability to adapt to the situation[40]. While previous studies have shown relatively consistent outcomes during the pandemic compared to the pre-pandemic period, our latest meta-analysis suggests a potential increase in the use of fibrinolytic therapy among countries with lower economic status, particularly in the eastern regions. Our subgroup analyses, which adjusted for income status, revealed that LMICs faced a higher incidence of fibrinolytic therapy and increased mortality rates for STEMI during the pandemic. Even before the pandemic, nearly three-quarters of myocardial infarction patients in such countries were treated with fibrinolytic therapy[41]. These findings raise concerns about the challenges faced by LMICs during the pandemic, as their lack of modern infrastructure may hinder their ability to provide timely reperfusion and cope with the pandemic's impact on STEMI care. Conversely, countries with high-income status and well-organized emergency systems have been able to continue using PPCI as the preferred treatment for patients requiring urgent intervention[42].
The fundamental principle of STEMI therapy is to achieve immediate, complete, and microvascular reperfusion to limit the extent of myocardial damage. Although PPCI remains the recommended reperfusion therapy by the American College of Cardiology and the Society for Cardiovascular Angiography and Interventions, it must be performed by an experienced team within a specific time frame to achieve the best outcomes. Compared to fibrinolytic therapy, PPCI significantly improves survival and reduces the risk of major adverse cardiovascular events, reinfarction, and intracranial hemorrhage[43]. However, if PPCI cannot be delivered promptly, there is a sharp increase in mortality rates. In response to the pandemic, an interim guideline from China suggested the use of fibrinolytic therapy for STEMI patients presenting to healthcare facilities within 12 h of symptom onset[44]. As the saying goes, 'Time is muscle', emphasizing the importance of prompt treatment to preserve viable myocardium.
Regarding the clinical relevance of our findings, our results suggest that there may have been a decrease in the use of PCI during the COVID-19 pandemic, which could have important implications for patient outcomes. PCI is generally considered the preferred treatment for STEMI, as it has been shown to reduce mortality and the risk of complications compared to fibrinolysis. Therefore, any reduction in the use of PCI should be carefully evaluated to ensure that patient care is not compromised. Overall, the results of our study highlight the impact of the COVID-19 pandemic on the incidence, treatment, and outcomes of STEMI. These findings have important implications for clinical practice, as they underscore the need for continued efforts to promote timely recognition and treatment of STEMI, even in the midst of a pandemic. Strategies such as public education campaigns, telemedicine, and streamlined healthcare delivery systems may help to mitigate the impact of the pandemic on the management of STEMI and improve patient outcomes.
This meta-analysis has some limitations that warrant consideration. Firstly, it is possible that the use of diverse fibrinolytic agents might have had an impact on our findings, thus confounding the results. Secondly, some of the outcomes in our study displayed high heterogeneity and wide confidence intervals, indicating low certainty. This could be due to the fact that the results were based on small sample sizes with varied outcomes. Additionally, the restriction of the review to English-language studies might have resulted in the exclusion of data published in other languages, which could have affected the findings.
Fibrinolysis-based reperfusion was found to be a major reperfusion strategy during the pandemic period, but the hypothesis of an association between overall all-cause mortality and the incidence of fibrinolysis was nullified. The present analysis of non-randomized studies was suggestive of a high casual association in populations living in LMICs. These results should remain an important focus of public health initiatives. The non-randomized selection process in individual studies could have contributed bias to the current meta-analysis.
ST-elevation myocardial infarction (STEMI) is a severe form of coronary artery disease with high morbidity and mortality rates. The preferred treatment is primary percutaneous coronary intervention, but the coronavirus disease 2019 (COVID-19) pandemic led to changes in STEMI management, including the use of fibrinolytic therapy as an alternative treatment.
The COVID-19 pandemic placed a significant strain on healthcare resources and providers, leading to changes in STEMI management. However, the impact of fibrinolytic therapy on clinical outcomes during the pandemic remains largely unknown.
The aim of this systematic review is to examine the significance of the increase in fibrinolytic therapy in adult STEMI patients during the COVID-19 pandemic compared to the pre-COVID-19 era and to assess the impact of this treatment strategy on clinical outcomes, particularly the risk of all-cause mortality, in comparison to patients who received standard-care before or during the pandemic.
This study analyzed the incidence of fibrinolytic therapy and all-cause mortality for STEMI patients during the COVID-19 pandemic compared to the pre-pandemic period. Data synthesis and analysis were performed using the DerSimonian and Laird random-effects model, subgrouping studies based on changes in fibrinolysis incidence and economic status of countries. The study used sensitivity analysis, meta-regression analysis, and Begg’s funnel plot test to assess publication bias and heterogeneity. Statistical significance was set at < 0.05.
This meta-analysis of 14 studies revealed a significantly higher incidence of fibrinolytic therapy in adult STEMI patients during the COVID-19 pandemic compared to the pre-pandemic era. Patients in low- and middle-income countries (LMICs) were more likely to receive fibrinolytic therapy, and those who received it in LMICs had a higher risk of all-cause mortality. However, overall, there was no significant association between the all-cause mortality rate and the incidence of fibrinolytic therapy. Meta-regression analysis showed that hyperlipidemia and hypertension were significant predictors of all-cause mortality, indicating that managing these conditions may be crucial in reducing mortality risk.
The incidence of fibrinolytic therapy for STEMI patients increased during the COVID-19 pandemic, particularly in LMICs. However, there was no significant association between fibrinolysis and all-cause mortality. The findings of this study have important implications for public health initiatives.
Fibrinolytic therapy was more frequently used during the COVID-19 pandemic, particularly in LMICs, but no significant association was found between the incidence of fibrinolysis and overall all-cause mortality.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Chest Physician.
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Tan X, China; Tumminello G, Italy; Yu F, China S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Makar AB, McMartin KE, Palese M, Tephly TR. Formate assay in body fluids: application in methanol poisoning. Biochem Med. 1975;13:117-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 88] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Steg PG, Goldberg RJ, Gore JM, Fox KA, Eagle KA, Flather MD, Sadiq I, Kasper R, Rushton-Mellor SK, Anderson FA; GRACE Investigators. Baseline characteristics, management practices, and in-hospital outcomes of patients hospitalized with acute coronary syndromes in the Global Registry of Acute Coronary Events (GRACE). Am J Cardiol. 2002;90:358-363. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 394] [Cited by in F6Publishing: 431] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 3. | Ibanez B. And fibrinolysis became pharmacoinvasive. Eur Heart J. 2020;41:855-857. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Daniels MJ, Cohen MG, Bavry AA, Kumbhani DJ. Reperfusion of ST-Segment-Elevation Myocardial Infarction in the COVID-19 Era: Business as Usual? Circulation. 2020;141:1948-1950. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 65] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 5. | Dervan E, Bhattacharyya DD, McAuliffe JD, Khan FH, Glynn SA. Ancient Adversary - HERV-K (HML-2) in Cancer. Front Oncol. 2021;11:658489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 6. | Gambaro A, Ho HH, Kaier TE, Pires-Morais G, Patel JA, Ansari Ramandi MM. Management of Acute Coronary Syndrome in the COVID-19 Era: Voices From the Global Cardiology Community. JACC Case Rep. 2020;2:1429-1432. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 7. | Kerkar PG, Naik N, Alexander T, Bahl VK, Chakraborty RN, Chatterjee SS, Chopra HK, Dani SI, Deb PK, Goswami KC, Guha S, Gupta R, Gupta V, Hasija PK, Jayagopal PB, Justin Paul G, Kahali D, Katyal VK, Khanna NN, Mandal M, Mishra SS, Mohanan PP, Mullasari A, Mehta S, Pancholia AK, Ray S, Roy D, Shanmugasundarm S, Sharma S, Singh BP, Tewari S, Tyagi SK, Venugopal KN, Wander GS, Yadav R, Das MK. Cardiological Society of India: Document on acute MI care during COVID-19. Indian Heart J. 2020;72:70-74. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 8. | Szerlip M, Anwaruddin S, Aronow HD, Cohen MG, Daniels MJ, Dehghani P, Drachman DE, Elmariah S, Feldman DN, Garcia S, Giri J, Kaul P, Kapur NK, Kumbhani DJ, Meraj PM, Morray B, Nayak KR, Parikh SA, Sakhuja R, Schussler JM, Seto A, Shah B, Swaminathan RV, Zidar DA, Naidu SS. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) Members and Graduates. Catheter Cardiovasc Interv. 2020;96:586-597. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 123] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 9. | Kamarullah W, Sabrina AP, Rocky MA, Gozali DR. Investigating the implications of COVID-19 outbreak on systems of care and outcomes of STEMI patients: A systematic review and meta-analysis. Indian Heart J. 2021;73:404-412. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1] [Cited by in F6Publishing: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17946] [Cited by in F6Publishing: 22270] [Article Influence: 7423.3] [Reference Citation Analysis (0)] |
| 11. | Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-2012. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14425] [Cited by in F6Publishing: 15688] [Article Influence: 653.7] [Reference Citation Analysis (0)] |
| 12. | Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603-605. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8858] [Cited by in F6Publishing: 10724] [Article Influence: 766.0] [Reference Citation Analysis (0)] |
| 13. | The World Bank. World development indicators. Washington, DC: International Bank for Reconstruction and Development/The World Bank; 2014. Available from: https://openknowledge.worldbank.org/bitstream/handle/10986/18237/9781464801631.Pdf?sequence=1&isAllowed=y. [Cited in This Article: ] |
| 14. | Sterne JA, Gavaghan D, Egger M. Publication and related bias in meta-analysis: power of statistical tests and prevalence in the literature. J Clin Epidemiol. 2000;53:1119-1129. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 1386] [Cited by in F6Publishing: 1471] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 15. | Daoulah A, Hersi AS, Al-Faifi SM, Alasmari A, Aljohar A, Balghith M, Alshehri M, Youssef AA, ElSayed O, Alama MN, Refaat WA, Alzahrani B, Dahdouh Z, Khan AS, Ghani MA, Soofi MA, Alasnag M, Kazim HM, Elganady A, Hassan T, Ibrahim AM, Amellal Z, Alsmadi F, Ghazi AM, Alshehri AM, Alhulayfi MS, Ghonim AA, Algazzar AS, Al Garni TA, AlHarbi W, Jouda AA, Al-Shaibi K, Albasiri S, Abuelatta R, Tawfik W, Magdy M, Alasmari SR, Selim E, Elramly M, Abufayyah MA, Alshahrani SS, Alqahtani AH, Ahmed FA, Ahmed WA, Lotfi A. STEMI and COVID-19 Pandemic in Saudi Arabia. Curr Probl Cardiol. 2021;46:100656. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Leng WX, Yang JG, Li XD, Jiang WY, Gao LJ, Wu Y, Yang YM, Yuan JQ, Yang WX, Qiao SB, Yang YJ. Impact of the shift to a fibrinolysis-first strategy on care and outcomes of patients with ST-segment-elevation myocardial infarction during the COVID-19 pandemic-The experience from the largest cardiovascular-specific centre in China. Int J Cardiol. 2021;329:260-265. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Song C, Liu S, Yin D, Wang Y, Zhao Y, Yang W, Qiao S, Dou K, Xu B. Impact of Public Health Emergency Response to COVID-19 on Management and Outcome for STEMI Patients in Beijing-A Single-Center Historic Control Study. Curr Probl Cardiol. 2021;46:100693. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 18. | Wang N, Zhang M, Su H, Huang Z, Lin Y. Fibrinolysis is a reasonable alternative for STEMI care during the COVID-19 pandemic. J Int Med Res. 2020;48:300060520966151. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 19. | Wu J, Mamas M, Rashid M, Weston C, Hains J, Luescher T, de Belder MA, Deanfield JE, Gale CP. Patient response, treatments, and mortality for acute myocardial infarction during the COVID-19 pandemic. Eur Heart J Qual Care Clin Outcomes. 2021;7:238-246. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 54] [Cited by in F6Publishing: 68] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 20. | Xiang D, Xiang X, Zhang W, Yi S, Zhang J, Gu X, Xu Y, Huang K, Su X, Yu B, Wang Y, Fang W, Huo Y, Ge J. Management and Outcomes of Patients With STEMI During the COVID-19 Pandemic in China. J Am Coll Cardiol. 2020;76:1318-1324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 161] [Cited by in F6Publishing: 152] [Article Influence: 38.0] [Reference Citation Analysis (0)] |
| 21. | Zhang F, Song X, Dang Y. Experience of ST Segment Elevation Myocardial Infarction Management During COVID-19 Pandemic From the Mainland of China. Cardiovasc Revasc Med. 2021;28:92-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 22. | Huang B, Xu C, Liu H, Deng W, Yang Z, Wan J, Yan H, Cao G, Chen J, Jiang H. In-Hospital Management and Outcomes of Acute Myocardial Infarction Before and During the Coronavirus Disease 2019 Pandemic. J Cardiovasc Pharmacol. 2020;76:540-548. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Erol MK, Kayıkçıoğlu M, Kılıçkap M, Güler A, Yıldırım A, Kahraman F, Can V, Inci S, Baysal SS, Er O, Zeybey U, Kafkas Ç, Yayla Ç, Arin CB, Aktaş I, Yalçın AA, Genç Ö. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: A nationwide study. Anatol J Cardiol. 2020;24:334-342. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 25] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 24. | Mesnier J, Cottin Y, Coste P, Ferrari E, Schiele F, Lemesle G, Thuaire C, Angoulvant D, Cayla G, Bouleti C, Gallet de Saint Aurin R, Goube P, Lhermusier T, Dillinger JG, Paganelli F, Saib A, Prunier F, Vanzetto G, Dubreuil O, Puymirat E, Boccara F, Eltchaninoff H, Cachanado M, Rousseau A, Drouet E, Steg PG, Simon T, Danchin N. Hospital admissions for acute myocardial infarction before and after lockdown according to regional prevalence of COVID-19 and patient profile in France: a registry study. Lancet Public Health. 2020;5:e536-e542. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 115] [Cited by in F6Publishing: 151] [Article Influence: 37.8] [Reference Citation Analysis (0)] |
| 25. | Balghith MA. The Impact of COVID-19 Pandemic on the Presentation and Hospital Management of STEMI Patients in a Tertiary Care Center in Saudi Arabia. Heart Views. 2020;21:166-170. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 1] [Reference Citation Analysis (0)] |
| 26. | Clifford CR, Le May M, Chow A, Boudreau R, Fu AYN, Barry Q, Chong AY, So DYF. Delays in ST-Elevation Myocardial Infarction Care During the COVID-19 Lockdown: An Observational Study. CJC Open. 2020;3:565-573. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 27. | Rodríguez-Leor O, Cid-Álvarez B, Pérez de Prado A, Rossello X, Ojeda S, Serrador A, López-Palop R, Martín-Moreiras J, Rumoroso JR, Cequier Á, Ibáñez B, Cruz-González I, Romaguera R, Moreno R; Working Group on the Infarct Code of the Interventional Cardiology Association of the Spanish Society of Cardiology Investigators, Villa M, Ruíz-Salmerón R, Molano F, Sánchez C, Muñoz-García E, Íñigo L, Herrador J, Gómez-Menchero A, Gómez-Menchero A, Caballero J, Ojeda S, Cárdenas M, Gheorghe L, Oneto J, Morales F, Valencia F, Ruíz JR, Diarte JA, Avanzas P, Rondán J, Peral V, Pernasetti LV, Hernández J, Bosa F, Lorenzo PLM, Jiménez F, Hernández JMT, Jiménez-Mazuecos J, Lozano F, Moreu J, Novo E, Robles J, Moreiras JM, Fernández-Vázquez F, Amat-Santos IJ, Gómez-Hospital JA, García-Picart J, Blanco BGD, Regueiro A, Carrillo-Suárez X, Tizón H, Mohandes M, Casanova J, Agudelo-Montañez V, Muñoz JF, Franco J, Del Castillo R, Salinas P, Elizaga J, Sarnago F, Jiménez-Valero S, Rivero F, Oteo JF, Alegría-Barrero E, Sánchez-Recalde Á, Ruíz V, Pinar E, Pinar E, Planas A, Ledesma BL, Berenguer A, Fernández-Cisnal A, Aguar P, Pomar F, Jerez M, Torres F, García R, Frutos A, Nodar JMR, García K, Sáez R, Torres A, Tellería M, Sadaba M, Mínguez JRL, Merchán JCR, Portales J, Trillo R, Aldama G, Fernández S, Santás M, Pérez MPP. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev Esp Cardiol (Engl Ed). 2020;73:994-1002. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 28. | Calvão J, Amador AF, Costa CMD, Araújo PM, Pinho T, Freitas J, Amorim S, Macedo F. The impact of the COVID-19 pandemic on acute coronary syndrome admissions to a tertiary care hospital in Portugal. Rev Port Cardiol. 2022;41:147-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 29. | Regev-Avraham Z, Halabi M, Israeli Z, Hussein O, Sharabi-Nov A, Rosenfeld I. Lipid profile as a strong indicator of coronary plaques: noninvasive assessment by multislice computerized tomography. Coron Artery Dis. 2021;32:329-334. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 30. | Coenen DM, Heinzmann ACA, Karel MFA, Cosemans JMEM, Koenen RR. The multifaceted contribution of platelets in the emergence and aftermath of acute cardiovascular events. Atherosclerosis. 2021;319:132-141. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 16] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 31. | Keech A, Colquhoun D, Best J, Kirby A, Simes RJ, Hunt D, Hague W, Beller E, Arulchelvam M, Baker J, Tonkin A; LIPID Study Group. Secondary prevention of cardiovascular events with long-term pravastatin in patients with diabetes or impaired fasting glucose: results from the LIPID trial. Diabetes Care. 2003;26:2713-2721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 218] [Cited by in F6Publishing: 240] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 32. | Boutouyrie P, Chowienczyk P, Humphrey JD, Mitchell GF. Arterial Stiffness and Cardiovascular Risk in Hypertension. Circ Res. 2021;128:864-886. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 88] [Cited by in F6Publishing: 170] [Article Influence: 56.7] [Reference Citation Analysis (0)] |
| 33. | Engel Gonzalez P, Omar W, Patel KV, de Lemos JA, Bavry AA, Koshy TP, Mullasari AS, Alexander T, Banerjee S, Kumbhani DJ. Fibrinolytic Strategy for ST-Segment-Elevation Myocardial Infarction: A Contemporary Review in Context of the COVID-19 Pandemic. Circ Cardiovasc Interv. 2020;13:e009622. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 34. | Chew NWS, Ow ZGW, Teo VXY, Heng RRY, Ng CH, Lee CH, Low AF, Chan MY, Yeo TC, Tan HC, Loh PH. The Global Effect of the COVID-19 Pandemic on STEMI Care: A Systematic Review and Meta-analysis. Can J Cardiol. 2021;37:1450-1459. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 25] [Cited by in F6Publishing: 52] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 35. | McNamara DA, VanOosterhout S, Klungle D, Busman D, Parker JL, Kampfschulte A, Jovinge S, Wohns D, Madder RD. Pandemic-Associated Delays in Myocardial Infarction Presentation in Predominantly Rural Counties With Low COVID-19 Prevalence. Am J Cardiol. 2022;169:18-23. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 3] [Reference Citation Analysis (0)] |
| 36. | Keeley EC, Boura JA, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361:13-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2931] [Cited by in F6Publishing: 2685] [Article Influence: 127.9] [Reference Citation Analysis (1)] |
| 37. | Furnica C, Chistol RO, Chiran DA, Stan CI, Sargu GD, Girlescu N, Tinica G. The Impact of the Early COVID-19 Pandemic on ST-Segment Elevation Myocardial Infarction Presentation and Outcomes-A Systematic Review and Meta-Analysis. Diagnostics (Basel). 2022;12. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 38. | Oettinger V, Stachon P, Hilgendorf I, Heidenreich A, Zehender M, Westermann D, Kaier K, von Zur Mühlen C. COVID-19 pandemic affects STEMI numbers and in-hospital mortality: results of a nationwide analysis in Germany. Clin Res Cardiol. 2023;112:550-557. [PubMed] [DOI] [Cited in This Article: ] [Reference Citation Analysis (0)] |
| 39. | Solhpour A, Yusuf SW. Fibrinolytic therapy in patients with ST-elevation myocardial infarction. Expert Rev Cardiovasc Ther. 2014;12:201-215. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 40. | Osuchowski MF, Aletti F, Cavaillon JM, Flohé SB, Giamarellos-Bourboulis EJ, Huber-Lang M, Relja B, Skirecki T, Szabó A, Maegele M. SARS-CoV-2/COVID-19: Evolving Reality, Global Response, Knowledge Gaps, and Opportunities. Shock. 2020;54:416-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 33] [Cited by in F6Publishing: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 41. | Chandrashekhar Y, Alexander T, Mullasari A, Kumbhani DJ, Alam S, Alexanderson E, Bachani D, Wilhelmus Badenhorst JC, Baliga R, Bax JJ, Bhatt DL, Bossone E, Botelho R, Chakraborthy RN, Chazal RA, Dhaliwal RS, Gamra H, Harikrishnan SP, Jeilan M, Kettles DI, Mehta S, Mohanan PP, Kurt Naber C, Naik N, Ntsekhe M, Otieno HA, Pais P, Piñeiro DJ, Prabhakaran D, Reddy KS, Redha M, Roy A, Sharma M, Shor R, Adriaan Snyders F, Weii Chieh Tan J, Valentine CM, Wilson BH, Yusuf S, Narula J. Resource and Infrastructure-Appropriate Management of ST-Segment Elevation Myocardial Infarction in Low- and Middle-Income Countries. Circulation. 2020;141:2004-2025. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 38] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 42. | Tumminello G, Barbieri L, Lucreziotti S, Gentile D, Conconi B, Centola M, Mafrici A, Carugo S. Impact of COVID-19 on STEMI: Second youth for fibrinolysis or time to centralized approach? Int J Cardiol Heart Vasc. 2020;30:100600. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 43. | Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, Rokos IC, Rumsfeld JS, Henry TD. Management of Acute Myocardial Infarction During the COVID-19 Pandemic: A Position Statement From the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP). J Am Coll Cardiol. 2020;76:1375-1384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 216] [Cited by in F6Publishing: 219] [Article Influence: 54.8] [Reference Citation Analysis (0)] |
| 44. | Zeng J, Huang J, Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People's Hospital. Intensive Care Med. 2020;46:1111-1113. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 121] [Cited by in F6Publishing: 110] [Article Influence: 27.5] [Reference Citation Analysis (0)] |