

Roberto Alves Lourençoa,b; Virgílio Garcia Moreiraa,b; Renato Gorga Bandeira de Melloa,c; Itamar de Souza Santosa,d; Sumika Mori Lina,d; Ana Lúcia Fiebrantz Pintoa,e; Lygia Paccini Lustosaa,f; Yeda Aparecida de Oliveira Duartea,d; Juliana Alcântara Ribeiroa,e; Clarice Câmara Correiaa,g; Henrique Novaes Mansura,h; Euler Ribeiroa,i; Roberta Rigo Dalla Cortea,c; Eduardo Ferriollia,j; Carlos André Ueharaa,k; Ana Maedaa,k; Tamara Petronia,k; Terezinha Silva Limaa,i; Sergio Falcão Durãoa,l; Ivan Aprahamiana,m; Carla Maria Avesania,b; Wilson Jacob Filhoa,d
DOI: 10.5327/Z2447-211520181800023
ABSTRACT
The aim of the present study was to describe the conceptual and operational definitions of the frailty syndrome recommended by the Brazilian Consensus on Frailty in Older People. In 2015, a task force consisting of Brazilian specialists on human aging conducted a bibliographical review on frailty among older people in Brazil and established a consensus on the main findings through periodic meetings. A total of 72 articles were included in the analysis, comprising one systematic review, two conceptual discussions, two methodological descriptions, four longitudinal studies focusing on mortality and worsening of the frailty profile, eight cross-cultural adaptation studies, and 55 cross-sectional or prevalence studies. Forty-five studies (62.5%) used the Cardiovascular Health Study (CHS) frailty scale, of which seven (15.2%) used unadjusted cut-off points for their samples and 17 (36.9%) modified at least one of the five items of the instrument. The prevalence of frailty varied between 6.7 and 74.1%. When the CHS frailty scale was used, the wide range of prevalence — from 8 to 49.3% — depended on the cut-off points used to classify changes in gait speed and handgrip strength, as well as the research setting. The studies were based on four major conceptual models of frailty. Frailty in older people represents a state of physiological vulnerability and should not be confused with disabilities or multi-morbidities. In the Brazilian population, the prevalence of frailty has not yet been adequately estimated, and the cut-off points of the items of the frailty scales should be adapted to the parameters of this population.
Keywords: aging; aged; health of the elderly; health vulnerability; frail elderly.
RESUMO
O objetivo do presente trabalho foi descrever as definições conceitual e operacional da síndrome de fragilidade recomendadas pelo Consenso Brasileiro de Fragilidade em Idosos. Em 2015, uma força-tarefa composta de especialistas brasileiros em envelhecimento humano conduziu uma revisão bibliográfica sobre fragilidade em idosos no Brasil e estabeleceu um consenso acerca dos principais achados por meio de reuniões periódicas. No total, 72 artigos foram incluídos para análise, entre os quais, uma revisão sistemática, duas discussões conceituais, duas descrições metodológicas, quatro estudos longitudinais focando mortalidade e piora do perfil de fragilidade, oito estudos de adaptação transcultural e 55 estudos transversais ou de prevalência. O Quarenta e cinco estudos (62,5%) utilizaram a escala de fragilidade do Cardiovascular Health Study (EFCHS), dos quais sete (15,2%) usaram pontos de corte não ajustados para a amostra e 17 (36,9%) modificaram pelo menos um dos cinco itens que compõem o instrumento. A prevalência de fragilidade variou entre 6,7 e 74,1%. Quando utilizada a EFCHS, a ampla variação de prevalência — de 8 a 49,3% — dependeu dos pontos de corte empregados para classificar as alterações na velocidade de marcha e na força de preensão palmar, bem como do cenário de investigação. Os estudos foram baseados em quatro grandes modelos conceituais de fragilidade. A fragilidade em idosos representa um estado de vulnerabilidade fisiológica e não deve ser confundida com incapacidades ou multimorbidades. Na população brasileira, a prevalência de fragilidade ainda não está adequadamente estimada, e os pontos de corte dos itens que compõem as escalas de fragilidade devem ser adaptados aos parâmetros dessa população.
Palavras-chave: envelhecimento; idoso; saúde do idoso; vulnerabilidade; fragilidade; idoso fragilizado.
INTRODUCTION
Frailty is a nonspecific state of increased risk of mortality and adverse health events such as dependence, disability, falls and injuries, acute illness, slow recovery from illness, hospitalization, and long-term institutionalization.1,2 In the elderly population, frail individuals are those most in need of health care, and, thus, frailty can be used as a potential organizer for older people health management.3
Given the rapidly aging population in our country, a consequence of demographic and epidemiological transitions, the number of frail individuals is increasing rapidly.4 In high-income countries, depending on the population evaluated, 10-25% of people aged 65 or over may be classified as frail,5 and many forms of geriatric healthcare, such as comprehensive evaluations, preventive interventions and multidisciplinary care, are targeted for frail individuals, since, in this group, these proceedings have better cost-effectiveness. Thus, when establishing investment priorities that align financial and quality of life conditions, the frail individual should be considered the primary target of health policies directed at the elderly population.6-9
Among the various conceptual models of frailty,10 reduced functional reserve, which involves multiple organ systems, has gained better acceptance among researchers in the field.11 In this model, frailty represents a state of heightened physiological vulnerability of heterogeneous presentation that is associated with chronological age and reflects multisystemic physiological changes that affect homeostatic adaptability. The most commonly used scale for instrumentalizing this definition consists of items that assess nutritional status, energy expenditure, physical activity, mobility and muscle strength.11
Another conceptual model is deficit accumulation, which is based on the sum of limitations and diseases and emphasizes the number of disorders rather than their nature. The instrument based on this model defines frailty using at least 30 variables, including disabilities and comorbidities.12
The third conceptual model is multidimensional, characterizing the condition as a dynamic state of loss that affects one or more areas, such as cognitive, physical and social domains.13-17 Finally, another series of measurement instruments are primarily based on functional disability.18,19
In Brazil, the diversity of conceptual and operational models has produced questions among those involved in geriatric health issues. Such questions include: areas of research — how best to investigate frailty; teaching — how to inform undergraduate and graduate students and health professionals; and care — how to identify and treat frail individuals in public and private health care networks.
This article describes the results of the discussions by Brazilian specialists in human aging organized on the Brazilian Consensus on Frailty in Older People (Consenso Brasileiro de Fragilidade em Idosos — CBFI) task force. The objective was to establish a national consensus about indicators for determining the epidemiological frequency of frailty syndrome in Brazil, as well as conceptual and operational definitions that could guide care, teaching and research by Brazilian geriatrics and gerontology professionals.
METHODS
Creation of the Brazilian Consensus on Frailty in Older People
The CBFI was created by a decision of ten academic institutions in geriatrics and gerontology that had been meeting in monthly teleconferences (TeleGero) since July 2005 to discuss issues related to human aging. During the September 2015 TeleGero meeting, based on a proposal by one member that was unanimously accepted, a committee of experts was formed to define the CBFI’s working methodology.
Following this meeting, a task force was formed with a variable number of members from each academic institution participating in TeleGero, as well as professionals from other institutions whose professional interest and/or care, teaching, research or management activities were related to frailty syndrome in older people.
The task force developed its activities through monthly teleconferences, electronic message exchange and a face-to-face meeting in 2016 in Fortaleza, Ceará, Brazil, during the XX Brazilian Congress of Geriatrics and Gerontology.
The problem to be addressed and the objectives of the CBFI task force
The criteria and conceptual and operational diversity of the instruments used to screen/diagnose the frailty syndrome are reflected in the following areas:
• healthcare: the difficulties that public and private health managers have in selecting population screening instruments;
• teaching: the difficulties in adequately training specialized professionals in geriatrics and gerontology;
• research: the difficulties in comparing results among different research settings and populations that inhabit Brazil.
Division of CBFI by theme
The members of the task force were subdivided into five groups, each responsible for one of the following thematic areas: conceptual definition; epidemiology; physiopathology; evaluation and diagnostic tools; prevention and treatment. Initially, each group worked independently and, subsequently, virtual meetings were held to integrate the information.
Narrative review and expert opinion
It was decided to conduct a narrative review of the five thematic areas by searching for articles published in scientific journals between January 2009 and August 2017 that addressed frailty syndrome in Brazilian population samples. The main reference databases — PubMed and the Scientific Electronic
Library Online — were searched using the (English) MeSH keywords frail, aged, frail elderly, elderly, Brazil, elders, older, and older adults, connected by the Boolean operators AND and OR.
The task force members discussed the main findings and conclusions until reaching a consensus about each theme. These positions were discussed during the development of this report until the final text was produced, which involves some of the epidemiological and conceptual questions and assessment instruments pertinent to national scientific research and production. A future document will describe the other aspects of the thematic areas addressed by the task force.
RESULTS AND DISCUSSION
Epidemiological aspects
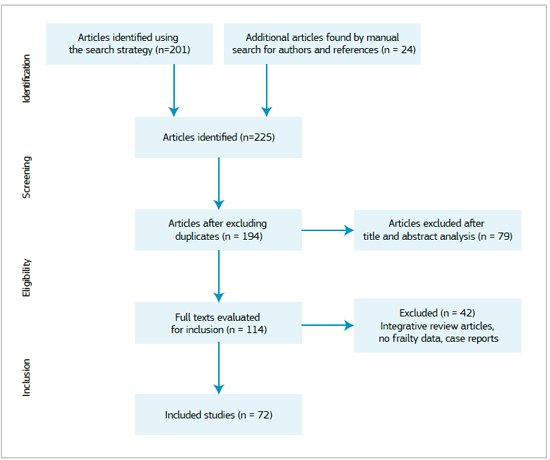
The database search found 201 articles, while a manual search for authors with publications in the field of aging and previously known bibliographic references identified another 24. Of this total, 193 articles (Figure 1) met the initial screening criteria. After title and abstract analysis, 79 of these were excluded, leaving 115 articles for full text assessment. Of these, 42 were excluded for one of the following reasons: being integrative reviews, being case reports or lacking descriptive data on frailty. Thus, a total of 72 articles were included in the analysis, including one systematic review, two conceptual discussions, two methodological descriptions, four longitudinal studies focusing on mortality and worsening of the frailty profile, eight cross-cultural adaptation studies and 55 cross-sectional or prevalence studies (Annex 1).
The study samples were selected from several settings. Three came from long-term care institutions for older people, five from hospital units, eight from outpatient clinics and 52 from community-dwelling populations. No research scenarios were presented in the four papers on methodology and concepts.
Regarding the instruments used to evaluate frailty, one study used a frailty index, one used the Clinical-Functional Vulnerability Index-20, one used an instrument developed by the Brazilian Ministry of Health, one used a self-report instrument, three used the Tilburg Frailty Indicator, three used the Kihon Checklist, three used the FRAIL scale (FS) and nine used the Edmonton Frail scale. Forty-five studies (62.5%) used the Cardiovascular Health Study (CHS) frailty scale, of which seven (15.2%) used unadjusted cut-off points for their sample and 17 (36.9%) modified at least one of the items of the instrument (Annex 1).
The prevalence of frailty in a 2016 systematic review ranged from 7.7 to 42.6%.20 In our review, this number was between 6.7 and 74.1%. The main sources of variation were the instrument used to classify individuals as frail and the assessment setting. When the CHS frailty scale was used, the broad prevalence range — from 8 to 49.3% — depended on the cutoff points used to classify the research setting (community, hospital, ambulatory or long-term care), changes in gait speed and handgrip strength.
Conceptual aspects
The instruments identified in this report used four major conceptual models of frailty and, corroborating the international literature, the CHS frailty scale was the most commonly applied instrument in Brazilian studies. The use of so many different instruments led to uniformity difficulties among the prevalence rates. The significant variation indicates that there is an expressive limitation on the results and the comparisons that can be made between them. The need for standardizing the model, and especially the diagnostic tool, is one of the challenges to identifying the frail elderly, and, in the light of the present consensus, still needs scrutiny. However, all of the studies, regardless of the model used, were unanimous in pointing out the urgent need to identify frailty syndrome, given its innumerable negative outcomes.
Evaluation instruments
Among the instruments observed in the present study, some valued the multidimensional aspects of older people (social, psychological, and cognitive), while others dealt exclusively with the physical elements of frailty. A clear distinction could be seen between these instruments and, from the point of view of definition, two major models were used: the vulnerability and the physiological frailty models. This issue permeated the discussion while this study was being prepared and will be the exclusive subject of a subsequent publication. In simplified terms, it was concluded that vulnerability is a comprehensive term that encompasses numerous dynamic dimensions — physiological, psychological, cultural and social.21 Physiological frailty, as defined by Buchner and Wagner,22 is a state of organic vulnerability, associated with aging and triggered by stressful events, in which an imbalance of homeostatic mechanisms occurs, promoting a negative spiral of undesirable events. With advancing age, the prevalence of comorbidities and limitations to functional capacity increases. Although these conditions usually accompany physiological frailty, they are distinct from it.23
Regarding instruments based on the physiological frailty model, especially the CHS frailty scale, it was observed that, even with five well-defined criteria — handgrip strength, gait speed, feeling of exhaustion, caloric expenditure and weight loss
— many studies resorted to cut-off points that were not adapted to their respective studies, specifically for the first two criteria. In addition, other studies chose to use only four of the five proposed criteria due to the existing limitations and diagnostic difficulties for this condition. Modifying these items leads to even further limitations in adequately identifying frailty in clinical practice.
CONCLUSIONS
The task force agreed on the following definitions and recommendations for care, teaching and research:
• frailty represents an age-related physiological vulnerability, produced by diminished homeostatic reserve and the organism’s reduced ability to cope with a variety of negative health outcomes, including hospital admissions, falls, and functional loss, which increases the likelihood of mortality;
• frailty should not be confused with disability, non-physiological vulnerability or multimorbidity;
• every health professional who assists older people must be familiar with frailty syndrome and its consequences;
• there is insufficient evidence to establish population strategies for frailty syndrome screening in the general elderly population. However, the task force considers that recognition of this syndrome is important, since it identifies elderly individuals at greater risk of unfavorable outcomes and, consequently, can impact individualized care;
• the FS and CHS frailty scale address frailty syndrome. The Edmonton, Tilburg and Kihon scales involve the concept of vulnerability. Studies should apply instruments that are relevant to their research objective: to identify the frail elderly or the vulnerable elderly;
• although normative data are not available for the Brazilian population, the cut-off points of frailty scale items, such as gait velocity and handgrip grip strength, should be adapted for the study population.
• Brazilian researchers should investigate simpler methods of identifying frailty syndrome that facilitate use in both specialized care settings, such as geriatrics clinics, and primary health care.
ACKNOWLEDGEMENTS
The ideas expressed in this document represent views of the members of the CBFI task force; they do not necessarily coincide with those of the consultants (listed below). The authors would like to thank the professionals, professors and researchers who have lent their time and knowledge in expressing their expert opinions.
Consultants: Anita Liberalesso Neri, José Elias Pinheiro, Tarso Mosci, Sergio Telles Ribeiro Filho, Elisabeth Vianna de Freitas, Luiz Garcez-Leme, Marcos Aparecido Sarria Cabrera, João Bastos Freire, Paulo Villas Boas, Einstein Camargos.
CONFLICT OF INTERESTS
The authors declare no conflicts of interest.
REFERENCES
1. Bilotta C, Nicolini P, Casè A, Pina G, Rossi S, Vergani C. Frailty syndrome diagnosed according to the Study of Osteoporotic Fractures (SOF) criteria and adverse health outcomes among community-dwelling older outpatients in Italy. A one-year prospective cohort study. Arch Gerontol Geriatr. 2012;54(2):e23-8. https://doi.org/10.1016/j.archger.2011.06.037
2. Winograd CH, Gerety MB, Chung M, Goldstein MK, Dominguez F Jr, Vallone R. Screening for frailty: criteria and predictors of outcomes. J Am Geriatr Soc. 1991;39(8):778-84.
3. Tello-Rodríguez T, Varela-Pinedo L. [Frailty in older adults: detection, community-based intervention, and decision-making in the management of chronic illnesses]. Rev Peru Med Exp Salud Publica. 2016;33(2):328-34.
4. Brasil. Instituto Brasileiro de Geografia e Estatística. Síntese de indicadores sociais: uma análise das condições de vida da população brasileira - 2015 [Internet]. Rio de Janeiro: Instituto Brasileiro de Geografia e Estatística, 2015 [citado em 12 mai. 2017]. Disponível em: http://biblioteca.ibge.gov.br/visualizacao/livros/liv95011.pdf
5. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487-92. https://doi.org/10.1111/j.1532-5415.2012.04054.x
6. Bock JO, Konig HH, Brenner H, Haefeli WE, Quinzler R, Matschinger H, et al. Associations of frailty with health care costs--results of the ESTHER cohort study. BMC Health Serv Res. 2016;16:128. https://doi.org/10.1186/s12913-016-1360-3
7. Sirven N, Rapp T. The cost of frailty in France. Eur J Health Econ. 2017;18(2):243-53. https://doi.org/10.1007/s10198-016-0772-7
8. Ekdahl AW, Alwin J, Eckerblad J, Husberg M, Jaarsma T, Mazya AL, et al. Long-term evaluation of the ambulatory geriatric assessment: a frailty intervention trial (AGe-FIT): clinical outcomes and total costs after 36 months. J Am Med Dir Assoc. 2016;17(3):263-8. https://doi.org/10.1016/j.jamda.2015.12.008
9. Comans TA, Peel NM, Hubbard RE, Mulligan AD, Gray LC, Scuffham PA. The increase in healthcare costs associated with frailty in older people discharged to a post-acute transition care program. Age Ageing. 2016;45(2):317-20. https://doi.org/10.1093/ageing/afv196
10. Aguayo GA, Donneau AF, Vaillant MT, Schritz A, Franco OH, Stranges S, et al. Agreement between 35 published frailty scores in the general population. Am J Epidemiol. 2017;186(4):420-34. https://doi.org/10.1093/aje/kwx061
11. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146-57. https://doi.org/10.1093/gerona/56.3.M146
12. Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. 2001;1:323-36. https://doi.org/10.1100/tsw.2001.58
13. Fabrício-Wehbe SC, Cruz IR, Haas VJ, Diniz MA, Dantas RA, Rodrigues RA. Reproducibility of the Brazilian version of the Edmonton Frail Scale for elderly living in the community. Rev Lat Am Enfermagem. 2013;21(6):1330-6. http://dx.doi.org/10.1590/0104-1169.2933.2371
14. Watanabe SM, Nekolaichuk C, Beaumont C, Johnson L, Myers J, Strasser F. A multicenter study comparing two numerical versions of the Edmonton Symptom Assessment System in palliative care patients. J Pain Symptom Manage. 2011;41(2):456-68. https://doi.org/10.1016/j.jpainsymman.2010.04.020
15. Fabrício-Wehbe SC, Schiaveto FV, Vendrusculo TR, Haas VJ, Dantas RA, Rodrigues RA. Cross-cultural adaptation and validity of the ‘Edmonton Frail Scale - EFS' in a Brazilian elderly sample. Rev Lat Am Enfermagem. 2009;17(6):1043-9.
16. Santiago LM, Luz LL, Mattos IE, Gobbens RJ, van Assen MA. Psychometric properties of the Brazilian version of the Tilburg frailty indicator (TFI). Arch Gerontol Geriatr. 2013;57(1):39-45. https://doi.org/10.1016/j.archger.2013.03.001
17. Santiago LM, Luz LL, Mattos IE, Gobbens RJ. [Cross-cultural adaptation of the Tilburg Frailty Indicator (TFI) for use in the Brazilian population]. Cad Saúde Pública. 2012;28(9):1795-801. http://dx.doi.org/10.1590/S0102-311X2012000900018
18. Hentschel L, Rentsch A, Lenz F, Hornemann B, Schmitt J, Baumann M, et al. A Questionnaire Study to Assess the Value of the Vulnerable Elders Survey, G8, and Predictors of Toxicity as Screening Tools for Frailty and Toxicity in Geriatric Cancer Patients. Oncol Res Treat. 2016;39(4):210-6. https://doi.org/10.1159/000445365
19. Moraes EN, Carmo JA, Moraes FL, Azevedo RS, Machado CJ, Montilla DE. Clinical-Functional Vulnerability Index-20 (IVCF-20): rapid recognition of frail older adults. Rev Saúde Pública. 2016;50:81. http://dx.doi.org/10.1590/s1518-8787.2016050006963
20. Da Mata FA, Pereira PP, Andrade KR, Figueiredo AC, Silva MT, Pereira MG. Prevalence of Frailty in Latin America and the Caribbean: A Systematic Review and Meta-Analysis. PLoS One. 2016;11(8):e0160019. https://doi.org/10.1371/journal.pone.0160019
21. Ayres JRCM, França Júnior I, Calazans GJ, Saletti Filho HC. [The vulnerability concept and the practices of health: new perspectives and challenges]. In: Czeresnia D, Freitas CM, Eds. Promoção da saúde: conceitos, reflexões, tendências [monografia]. Rio de Janeiro: Fundação Oswaldo Cruz; 2003.
22. Buchner DM, Wagner EH. Preventing frail health. Clin Geriatr Med. 1992;8(1):1-17.
23. Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc. 2006;54(6):991-1001. https://doi.org/10.1111/j.1532-5415.2006.00745.x
24. Tribess S, Virtuoso Júnior JS, Oliveira RJ. Physical activity as a predictor of absence of frailty in the elderly. Rev Assoc Med Bras (1992). 2012;58(3):341-7.
25. Costa TB, Neri AL. [Indicators of physical activity and frailty in the elderly: data from the FIBRA study in Campinas, Sao Paulo State, Brazil]. Cad Saúde Pública. 2011;27(8):1537-50.
26. Miguel R de C, Dias RC, Dias JM, da Silva SL, Menicucci Filho PR, Ribeiro TM. Frailty syndrome in the community-dwelling elderly with osteoarthritis. Rev Bras Reumatol. 2012;52(3):331-47.
27. Andrade NA, Fernandes MGM, Nóbrega MML, Garcia TR, Costa KNFM. Análise do conceito fragilidade em idosos. Texto & Contexto - Enferm. 2012;21(4):748-56. http://dx.doi.org/10.1590/S0104-07072012000400004
28. Bastos-Barbosa RG, Ferriolli E, Coelho EB, Moriguti JC, Nobre F, Lima NK. Association of frailty syndrome in the elderly with higher blood pressure and other cardiovascular risk factors. Am J Hypertens. 2012;25(11):1156-61. https://doi.org/10.1038/ajh.2012.99
29. Macuco CR, Batistoni SS, Lopes A, Cachioni M, da Silva Falcão DV, Neri AL, et al. Mini-Mental State Examination performance in frail, pre-frail, and non-frail community dwelling older adults in Ermelino Matarazzo, São Paulo, Brazil. Int Psychogeriatr. 2012;24(11):1725-31. https://doi.org/10.1017/S1041610212000907
30. Santiago LM, Luz LL, Mattos IE, Gobbens RJJ. Adaptação transcultural do instrumento Tilburg Frailty Indicator (TFI) para a população brasileira. Cad Saúde Pública. 2012;28(9):1795-801. http://dx.doi.org/10.1590/S0102-311X2012000900018
31. Sousa AC, Dias RC, Maciel AC, Guerra RO. Frailty syndrome and associated factors in community-dwelling elderly in Northeast Brazil. Arch Gerontol Geriatr. 2012;54(2):e95-101.
32. Yassuda MS, Lopes A, Cachioni M, Falcao DV, Batistoni SS, Guimaraes VV, et al. Frailty criteria and cognitive performance are related: data from the FIBRA study in Ermelino Matarazzo, São Paulo, Brazil. J Nutr Health Aging. 2012;16(1):55-61.
33. Fattori A, Santimaria MR, Alves RM, Guariento ME, Neri AL. Influence of blood pressure profile on frailty phenotype in community-dwelling elders in Brazil - FIBRA study. Arch Gerontol Geriatr. 2013;56(2):343-9. https://doi.org/10.1016Zj.archger.2012.08.004
34. Lenardt MH, Carneiro NH, Betiolli SE, Ribeiro DK, Wachholz PA. Prevalence of pre-frailty for the component of gait speed in older adults. Rev Lat Am Enfermagem. 2013;21(3):734-41. http://dx.doi.org/10.1590/S0104-11692013000300012
35. Borges CL, Silva MJ, Clares JWB, Bessa MEP, Freitas MC. Avaliação da fragilidade de idosos institucionalizados. Acta Paul Enferm. 2013;26(4):318-22. http://dx.doi.org/10.1590/S0103-21002013000400004
36. Faria CA, Lourenço RA, Ribeiro PC, Lopes CS. [Cognitive performance and frailty in older adults clients of a private health care plan]. Rev Saúde Pública. 2013;47(5):923-30. http://dx.doi.org/10.1590/S0034-8910.2013047004451
37. Neri AL, Yassuda MS, Araújo LF, Eulálio M do C, Cabral BE, Siqueira ME, et al. [Methodology and social, demographic, cognitive, and frailty profiles of community-dwelling elderly from seven Brazilian cities: the FIBRA Study]. Cad Saúde Pública. 2013;29(4):778-92. http://dx.doi.org/10.1590/S0102-311X2013000400015
38. Perez M, Lourenço RA. Rede FIBRA-RJ: fragilidade e risco de hospitalização em idosos da cidade do Rio de Janeiro, Brasil. Cad Saúde Pública. 2013;29(7):1381-91. http://dx.doi.org/10.1590/S0102-311X2013000700012
39. Moreira VG, Lourenço RA. Prevalence and factors associated with frailty in an older population from the city of Rio de Janeiro, Brazil: the FIBRA-RJ Study. Clinics (Sao Paulo). 2013;68(7):979-85. https://doi.org/10.6061/clinics/2013(07)15
40. Duarte MC, Fernandes M, Rodrigues RA, Nóbrega MM. [Prevalence and sociodemographic factors associated with frailty in elderly women]. Rev Bras Enferm. 2013;66(6):901-6. http://dx.doi.org/10.1590/S0034-71672013000600014
41. Vieira RA, Guerra RO, Giacomin KC, Vasconcelos KS, Andrade AC, Pereira LS, et al. [Prevalence of frailty and associated factors in community-dwelling elderly in Belo Horizonte, Minas Gerais State, Brazil: data from the FIBRA study]. Cad Saúde Pública. 2013;29(8):1631-43. http://dx.doi.org/10.1590/0102-311X00126312
42. Oliveira DR, Bettinelli LA, Pasqualotti A, Corso D, Brock F, Erdmann AL. Prevalence of frailty syndrome in old people in a hospital institution. Rev Lat Am Enfermagem. 2013;21(4):891-8. https://doi.org/10.1590/S0104-11692013000400009
43. de Andrade FB, Lebrão ML, Santos JL, Duarte YA. Relationship between oral health and frailty in community-dwelling elderly individuals in Brazil. J Am Geriatr Soc. 2013;61(5):809-14. https://doi.org/10.1111/jgs.12221
44. Alencar MA, Dias JM, Figueiredo LC, Dias RC. Frailty and cognitive impairment among community-dwelling elderly. Arq Neuropsiquiatr. 2013;71(6):362-7. https://doi.org/10.1590/0004-282X20130039
45. Fhon JR, Rosset I, Freitas CP, Silva AO, Santos JL, Rodrigues RA. Prevalence of falls among frail elderly adults. Rev Saúde Pública. 2013;47(2):266-73. https://doi.org/10.1590/S0034-8910.2013047003468
46. Ricci NA, Pessoa GS, Ferriolli E, Dias RC, Perracini MR. Frailty and cardiovascular risk in community-dwelling elderly: a population-based study. Clin Interv Aging. 2014;9:1677-85. https://doi.org/10.2147/CIA.S68642
47. Santos AA, Ceolim MF, Pavarini SCI, Neri AL, Rampazo MK. Associação entre transtornos do sono e níveis de fragilidade entre idosos. Acta Paul Enferm. 2014;27(2):120-5. http://dx.doi.org/10.1590/1982-0194201400022
48. Mansur HN, Colugnati FA, Grincenkov FR, Bastos MG. Frailty and quality of life: a cross-sectional study of Brazilian patients with pre-dialysis chronic kidney disease. Health Qual Life Outcomes. 2014;12:27. https://doi.org/10.1186/1477-7525-12-27
49. Melo DM, Falsarella GR, Neri AL. Autoavaliação de saúde, envolvimento social e fragilidade em idosos ambulatoriais. Rev Bras Geriatr Gerontol. 2014;17(3):471-84. http://dx.doi.org/10.1590/1809-9823.2014.13172
50. Santiago LM, Mattos IE. Prevalência e fatores associados à fragilidade em idosos institucionalizados das regiões Sudeste e Centro-Oeste do Brasil. Rev Bras Geriatr Gerontol. 2014;17(2):327-37. http://dx.doi.org/10.1590/S1809-98232014000200010
51. Sewo Sampaio PY, Sampaio RA, Yamada M, Ogita M, Arai H. Validation and translation of the Kihon Checklist (frailty index) into Brazilian Portuguese. Geriatr Gerontol Int. 2014;14(3):561-9. https://doi.org/10.1111/ggi.12134
52. Silva JC, Moraes ZV, Silva C, Mazon S de B, Guariento ME, Neri AL, et al. Understanding red blood cell parameters in the context of the frailty phenotype: interpretations of the FIBRA (Frailty in Brazilian Seniors) study. Arch Gerontol Geriatr. 2014;59(3):636-41. https://doi.org/10.1016/j.archger.2014.07.014
53. Vidal EI. Frailty in older adults: perspectives for research and practice in Public Health. Cad Saúde Pública. 2014;30(6):1133-5. http://dx.doi.org/10.1590/0102-311XED010614
54. Pegorari MS, Tavares DM. Factors associated with the frailty syndrome in elderly individuals living in the urban area. Rev Lat Am Enfermagem. 2014;22(5):874-82.
55. Guedes RC, Dias RC, Pereira LS, Silva SL, Lustosa LP, Dias JM. Influence of dual task and frailty on gait parameters of older community-dwelling individuals. Braz J Phys Ther. 2014;18(5):445-52. http://dx.doi.org/10.1590/bjpt-rbf.2014.0034
56. Nóbrega PV, Maciel AC, de Almeida Holanda CM, Oliveira Guerra R, Araújo JF. Sleep and frailty syndrome in elderly residents of long-stay institutions: a cross-sectional study. Geriatr Gerontol Int. 2014;14(3):605-12. https://doi.org/10.1111/ggi.12144
57. Reis Júnior WM, Carneiro JA, Coqueiro R da, Santos KT, Fernandes MH. Pre-frailty and frailty of elderly residents in a municipality with a low Human Development Index. Rev Lat Am Enfermagem. 2014;22(4):654-61. http://dx.doi.org/10.1590/0104-1169.3538.2464
58. Alexandre TS, Corona LP, Nunes DP, Santos JL, Duarte YA, Lebrão ML. Similarities among factors associated with components of frailty in elderly: SABE Study. J Aging Health. 2014;26(3):441-57. https://doi.org/10.1177/0898264313519818
59. Azevedo da Silva SL, Viana JU, Neri AL, Ferriolli E, Lourenço RA, Dias RC. Influence of frailty phenotype items on functional capacity and falls occurrence in frail community-dwelling elderly: analysis of FIBRA Study. Top Geriatr Rehabil. 2016;32(2):74-80. http://dx.doi.org/10.1097/TGR.0000000000000096
60. Varela FR, Ciconelli RM, Campolina AG, Soarez PC. Quality of life evaluation of frail elderly in Campinas, São Paulo. Rev Assoc Med Bras (1992). 2015;61(5):423-30. https://doi.org/10.1590/1806-9282.61.05.423
61. Lourenço RA, Sanchez MA, Moreira VG, Ribeiro PCC, Perez M, Campos GC, et al. Frailty in older Brazilians - FIBRA-RJ: research methodology on frailty, cognitive disorders and sarcopenia. Rev Hospital Pedro Ernesto. 2015;14(4):13-22.
62. Pires Corona L, Drumond Andrade FC, de Oliveira Duarte YA, Lebrao ML. The relationship between anemia, hemoglobin concentration and frailty in Brazilian older adults. J Nutr Health Aging. 2015;19(9):935-40. https://doi.org/10.1007/s12603-015-0502-3
63. Falsarella GR, Gasparotto LP, Barcelos CC, Coimbra IB, Moretto MC, Pascoa MA, et al. Body composition as a frailty marker for the elderly community. Clin Interv Aging. 2015;10:1661-6. https://dx.doi.org/10.2147 %2FCIA.S84632
64. Katayama PL, Dias DP, Silva LE, Virtuoso-Junior JS, Marocolo M. Cardiac autonomic modulation in non-frail, pre-frail and frail elderly women: a pilot study. Aging Clin Exp Res. 2015;27(5):621-9. https://doi.org/10.1007/s40520-015-0320-9
65. Mansur HN, Lovisi JC, Colugnati FA, Raposo NR, Fernandes NM, Bastos MG. Association of frailty with endothelial dysfunction and its possible impact on negative outcomes in Brazilian predialysis patients with chronic kidney disease. BMC Nephrol. 2015;16:157. https://doi.org/10.1186/s12882-015-0150-1
66. Bastone AC, Ferriolli E, Teixeira CP, Dias JM, Dias RC. Aerobic fitness and habitual physical activity in frail and nonfrail community-dwelling elderly. J Phys Act Health. 2015;12(9):1304-11. https://doi.org/10.1123/jpah.2014-0290
67. Frisoli A Jr, Ingham SJ, Paes ÂT, Tinoco E, Greco A, Zanata N, et al. Frailty predictors and outcomes among older patients with cardiovascular disease: Data from Fragicor. Arch Gerontol Geriatr. 2015;61(1):1-7. https://doi.org/10.1016Zj.archger.2015.03.001
68. Sampaio PY, Sampaio RA, Yamada M, Ogita M, Arai H. Comparison of frailty among Japanese, Brazilian Japanese descendants and Brazilian community-dwelling older women. Geriatr Gerontol Int. 2015;15(6):762-9. https://doi.org/10.1111/ggi.12348
69. Parentoni AN, Mendonça VA, Dos Santos KD, Sá LF, Ferreira FO, Gomes Pereira DA, et al. Gait speed as a predictor of respiratory muscle function, strength, and frailty syndrome in community-dwelling elderly people. J Frailty Aging. 2015;4(2):64-8. https://doi.org/10.14283/jfa.2015.41
70. Lanziotti Azevedo da Silva S, Campos Cavalcanti Maciel Á, de Sousa Máximo Pereira L, Domingues Dias JM, Guimarães de Assis M, Corrêa Dias R. Transition patterns of frailty syndrome in community-dwelling elderly individuals: a longitudinal study. J Frailty Aging. 2015;4(2):50-5. https://doi.org/10.14283/jfa.2015.43
71. Nunes DP, Duarte YA, Santos JL, Lebrão ML. Screening for frailty in older adults using a self-reported instrument. Rev Saúde Pública. 2015;49:2.
72. Faria GS, Ribeiro TMS, Vieira RA, Silva SLA, Dias RC. Transição entre níveis de fragilidade em idosos no município de Belo Horizonte, Minas Gerais. Rev Bras Geriatr Gerontol. 2016;19(2):335-41. http://dx.doi.org/10.1590/1809-98232016019.140232
73. Carneiro JA, Ramos GC, Barbosa AT, Mendonça JM, Costa FM, Caldeira AP. Prevalência e fatores associados à fragilidade em idosos não institucionalizados. Rev Bras Enferm. 2016;69(3):435-42. http://dx.doi.org/10.1590/0034-7167.2016690304i
74. Calado LB, Ferriolli E, Moriguti JC, Martinez EZ, Lima NK. Frailty syndrome in an independent urban population in Brazil (FIBRA study): a crosssectional populational study. Sao Paulo Med J. 2016;134(5):385-92. http://dx.doi.org/10.1590/1516-3180.2016.0078180516
75. Tavares DM, Colamego CG, Pegorari MS, Ferreira PC, Dias FA, Bolina AF. Cardiovascular risk factors associated with frailty syndrome among hospitalized elderly people: a cross-sectional study. Sao Paulo Med J. 2016;134(5):393-9. http://dx.doi.org/10.1590/1516-3180.2016.0028010616
76. Sewo Sampaio PY, Sampaio RA, Coelho Júnior HJ, Teixeira LF, Tessutti VD, Uchida MC, et al. Differences in lifestyle, physical performance and quality of life between frail and robust Brazilian community-dwelling elderly women. Geriatr Gerontol Int. 2016;16(7):829-35. https://doi.org/10.1111/ggi.12562
77. Fabrício-Wehbe SC, Rodrigues RA, Haas VJ, Fhon JR, Diniz MA. Association of frailty in hospitalized and institutionalized elderly in the community-dwelling. Rev Bras Enferm. 2016;69(4):691-6. http://dx.doi.org/10.1590/0034-7167.2016690411i
78. Lenardt MH, Carneiro NH, Binotto MA, Willig MH, Lourenço TM, Albino J. Frailty and quality of life in elderly primary health care users. Rev Bras Enferm. 2016;69(3):478-83. http://dx.doi.org/10.1590/0034-7167.2016690309i
79. Teixeira-Gasparini E, Partezani-Rodrigues R, Fabricio-Wehbe S, Silva-Fhon J, Aleixo-Diniz M, Kusumota L. Uso de tecnologías de asistencia y fragilidad en adultos mayores de 80 años y más. Enferm Univ. 2016;13(3):151-8. https://doi.org/10.1016/j.reu.2016.06.001
80. Silva SL, Neri AL, Ferrioli E, Lourenço RA, Dias RC. Fenótipo de fragilidade: influência de cada item na determinação da fragilidade em idosos comunitários - Rede Fibra. Cien Saude Colet. 2016;21(11):3483-92. http://dx.doi.org/10.1590/1413-812320152111.23292015
81. Zazzetta MS, Gomes GA, Orlandi FS, Gratão AC, Vasilceac FA, Gramani-Say K, et al. Identifying frailty levels and associated factors in a population living in the context of poverty and social vulnerability. J Frailty Aging. 2017;6(1):29-32. https://doi.org/10.14283/jfa.2016.116
82. Mello AC, Carvalho MS, Alves LC, Gomes VP, Engstrom EM. Consumo alimentar e antropometria relacionados à síndrome de fragilidade em idosos residentes em comunidade de baixa renda de um grande centro urbano. Cad Saúde Pública. 2017;33(8):e00188815. http://dx.doi.org/10.1590/0102-311x00188815
83. Marchiori GF, Tavares D. Changes in frailty conditions and phenotype components in elderly after hospitalization. Rev Lat Am Enfermagem. 2017;25:e2905. https://doi.org/10.1590/1518-8345.1417.2905
84. Santos-Orlandi AAD, Brito TRP, Ottaviani AC, Rossetti ES, Zazzetta MS, Pavarini SCI. Elderly who take care of elderly: a study on the Frailty Syndrome. Rev Bras Enferm. 2017;70(4):822-9. https://doi.org/10.1590/0034-7167-2016-0474
85. Carneiro JA, Cardoso RR, Durães MS, Guedes MCA, Santos FL, Costa FM, et al. Frailty in the elderly: prevalence and associated factors. Rev Bras Enferm. 2017;70(4):747-52. http://dx.doi.org/10.1590/0034-7167-2016-0633
86. Pereira AA, Borim FSA, Neri AL. Absence of association between frailty index and survival in elderly Brazilians: the FIBRA Study. Cad Saúde Pública. 2017;33(5):e00194115. http://dx.doi.org/10.1590/0102-311x00194115
87. Liberalesso TEM, Dallazen F Bandeira VAC, Berlezi EM. Prevalência de fragilidade em uma população de longevos na região Sul do Brasil. Saúde Debate. 2017;41(113):553-62. http://dx.doi.org/10.1590/0103-1104201711316
88. Aprahamian I, Lin SM, Suemoto CK, Apolinario D, Oiring de Castro Cezar N, Elmadjian SM, et al. Feasibility and factor structure of the FRAIL scale in older adults. J Am Med Dir Assoc. 2017;18(4):367. e11-367.e18. https://doi.org/10.1016/jjamda.2016.12.067
89. Cezar NOC, Izbicki R, Cardoso D, Almeida JG, Valiengo L, Camargo MVZ, et al. Frailty in older adults with amnestic mild cognitive impairment as a result of Alzheimer's disease: a comparison of two models of frailty characterization. Geriatr Gerontol Int. 2017;17(11):2096-102. https://doi.org/10.1111/ggi.13028
90. Aprahamian I, Cezar NOC, Izbicki R, Lin SM, Paulo DLV, Fattori A, et al. Screening for frailty with the FRAIL scale: a comparison with the phenotype criteria. J Am Med Dir Assoc. 2017;18(7):592-6. https://doi.org/10.1016/j.jamda.2017.01.009
Received in
April 10 2018.
Accepted em
April 11 2018.