Abstract
Context:
The liver, one of the most important organs of the body, is known to be responsible for several functions. The functional contribution of the liver to the metabolism of carbohydrates, protein, drugs and toxins, fats and cholesterol and many other biological processes are still unknown. Liver disorders are classified into two types: acute and chronic. Different drugs are used in liver diseases to treat and control pain. Most pain relief medications such as opioids are metabolized via the liver; therefore, the adverse reactions of drugs are probably higher for patients with liver disease. The current study aimed to evaluate the effects of opioid drugs on patients with liver disease; therefore, it is necessary to select suitable opioids for such patients.Evidence Acquisition:
This review was written by referring to research literature including 70 articles and four textbooks published from 1958 to 2015 on various reputable sites. Searches were carried out on the key phrases of narcotic pain relievers (opioids), acute and chronic hepatic failure, opioid adverse drug reactions, drug-induced liver injury (DILI) and other similar keywords. References included a variety of research papers (descriptive and analytical), intervention and review articles.Results:
In patients with liver disease, administration of opioid analgesics should be observed, accurately. As a general rule, lower doses of drugs should be administered at regular intervals based on the signs of drug accumulation. Secondly, the interactions of opioid drugs with different levels of substrates of the P450 cytochrome enzyme should be considered.Conclusions:
Pain management in patients with liver dysfunction is always challenging to physicians because of the adverse reactions of drugs, especially opioids. Opioids should be used cautiously since they can cause sedation, constipation and sudden encephalopathy effects. Since the clearance of these drugs in patients with hepatic insufficiency is decreased, the initial dose must be decreased, the intervals between doses should be increased and some patients need to be continuously assessed.Keywords
1. Context
The liver is one of the most important organs of the body since it plays important roles in several functions (1, 2). The metabolism of carbohydrates (glycogen storage and control), protein (metabolism of albumin and many other proteins which play essential roles in homeostasis and the immune system), drugs and toxins (metabolism based on the activity of cytochrome enzymes, etc.) and fats and cholesterol as well as many other biological processes, some of which are still unknown (3, 4). Obviously, hepatic impairments are vast and complicated.
Liver disease is the tenth most common cause of death in the United States leading to 25000 deaths every year (5, 6). Liver disorders are classified into two groups: acute and chronic. As disease initiates, liver cells are damaged or destroyed. If the injury is mild and reversible, then liver cells are reconstructed and the liver returns to its normal state; however, if the damage is severe, reconstruction does not happen and the damage to the liver is permanent. Permanent injuries cause fibrosis, liver destruction, loss of function, bleeding disorders, high portal pressure and damage, and or hepatic encephalopathy (7).
In terms of etiology, the most important causes of acute liver disease in the world include viral infections and alcohol or drug toxicity (especially in developed countries) (5). Viral hepatitis B and C, alcohol, autoimmune hepatitis and genetic disorders are major causes of chronic liver dysfunction (1, 4). The slow and prolonged causes of liver disease lead to increased number of patients. Since liver disease causes several systemic problems, it is necessary to look at the treatment type and particularly their pharmacodynamics. Cirrhosis is the twelfth most common cause of death in America. Patients with advanced chronic liver failure (i.e. patients with cirrhosis) take numerous complications in many biological systems including coagulation disorders, gastrointestinal bleeding, esophageal varices, gynecomastia and testicular atrophy, albumin and cholesterol metabolism disorders, thrombocytopenia and leukopenia, anemia, hyponatremia, renal dysfunction (hepatorenal syndrome), impaired lung function (hepatopulmonary syndrome), nausea, anorexia, spontaneous bacterial peritonitis, etc., all of which evidence the vital role of liver (7-9). Because of the mentioned problems, patients with liver diseases are treated with several drugs. Moreover, they are periodically treated with surgery and endoscopic procedures which require the use of many analgesics, including opioids. Based on the importance of this issue for internists, a detailed discussion is formed known as drug-induced liver injury or drug-induced liver injury (DILI) (10).
Another important problem which patients with liver disease face is that unlike other diseases such as kidney failure, there is no numerical measure (such as glomerular filtration rate) or specific guidelines to determine the severity of the liver failure. Some classifications are provided according to serum albumin, bilirubin, coagulation time and the presence of ascites, but a comprehensive protocol is not developed yet (4, 10). Additionally, much of the research relies on the pharmacokinetic properties of drugs (even at low doses), but sufficient knowledge about the potential harmful effects of drugs, particularly opioids, is not available. In fact, comprehensive information regarding pharmacodynamics is not available. Therefore, the administration of these drugs is more difficult (11).
Metabolic pathways of pain relief medications, including opioids, pass through the liver (oxidation, de-alkylation, conversion, and combining). Therefore, in patients with reduced hepatic function, the metabolic pathways are affected and the toxicity probability of these drugs increases. Indeed, with liver disease in which the metabolic pathways of drugs are disturbed, they are exerted lowly and accumulate in plasma, which means that the half-life of the drug will increase in the body and the adverse drug reactions of this group of drugs appear more severe (12).
Albumin is a protein which binds to and facilitates the exertion of certain drugs. Albumin synthesis is decreased with liver disease; therefore, it leads to increased serum levels of some drugs. Thus, the risk of adverse drug reactions increases (13).
Drugs are a collection of natural and chemical morphine-like substances called opioids which bind to opioid receptors in synapses. They all work as neurotransmitters in the body (endorphins) by affecting the central nervous system that causes pain relieving (13). Opioids act as analgesics through μ and κ receptors. Ability, strength, and duration of action are different in opioids, while their tendency for μ receptors and solubility in fat (lipophilicity) determines the difference level (13, 14).
1.1. Hepatic Metabolism of Opioids
There are two different types of chemical reactions in the liver metabolism of drugs. The first type is transfer-oxidation reaction that is catalyzed by the cytochrome P450 enzyme system and metabolizes most opioids. Clearance of opioids decreases in liver failure and their bioavailability increases. These changes may be considered as secondary outcomes of the reduction in liver blood flow (the limitation of primary route of metabolism) or the reduction of the cytochrome P450 enzymes levels. The second group of chemical reactions consists of conjugation and glucuronidation in the liver. The reactions are less affected, since the glucuronidase are preserved in patients with liver disease; moreover, extra-hepatic glucuronidation is less affected by the hepatic criteria, and the opioid metabolites are generally exerted by the kidneys. The reduction in the serum albumin level changes the quality of opioid distribution volumes that either increases or decreases the accumulation of drugs. Although there is no practical method to test or predict the clinical observations, at least a part of most opiates are metabolized by the liver. Therefore, the administration of opioids to patients with liver failure is high risk and requires precaution be taken to minimize their side effects (15, 16).
The current study used articles that population (P) were over the age of eighteen and had liver disease, intervention (I) was use of opioid drugs and outcome (O) was: whether or not to use opioids in patients with liver disease.
2. Evidence Acquisition
2.1. Data Sources
The present study is a systematic review. The research literature included 70 papers and four books published from 1958 to 2015 at various reliable data bases (PubMed, Medline (Ovid), Cochrane).
2.2. Study Selection
Searches were performed on keywords such as opioid pain relievers (opioids), hepatic failure, acute and chronic opioid adverse drug reactions, drug-induced liver injury (DILI) and other similar keywords.
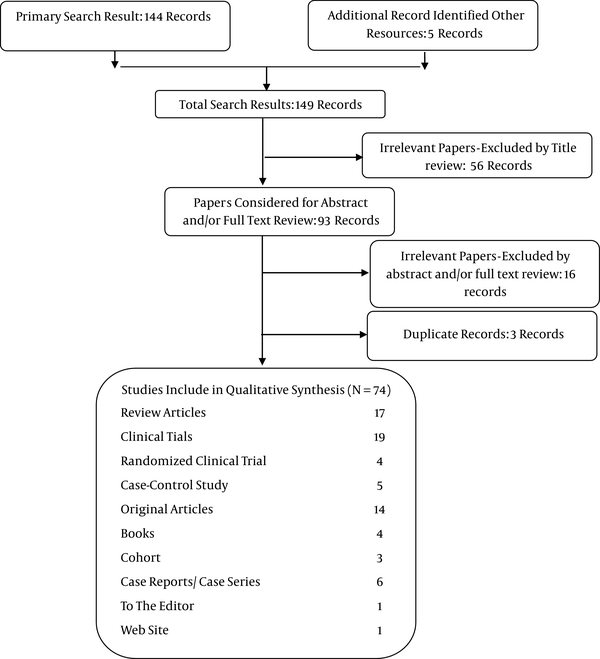
The primary search resulted in 145 articles and four books. The irrelevant data including 75 irrelevant abstracts or full-text review, duplicate records and lack of access to the full-text of the articles or books were excluded. Resources included 17 review articles, 19 clinical trials, four randomized clinical trials, five case-control, four books, three cohort studies, six case reports or case series, one to the editor and one web site.
2.3. Data Extraction and Quality Assessment
Two independent authors managed and ran the data extraction and quality assessment. The quality of clinical trials, cohort studies and case control studies were assessed using CASP (critical appraisal skills program) with their checklists. Furthermore, for cross sectional studies STROBE (strengthening the reporting of observational studies in epidemiology) was used. Studies scoring more than 50% were included in the review.
3. Results
In the current study, after the initial search and based on the titles found, a total of 93 potentially relevant papers were selected. After removing three duplicate studies, the abstracts of these papers were carefully studied and 16 papers were excluded as they did not meet the inclusion criteria. Finally 74 studies were included in the study (Figure 1), (Tables 1, 2, 3, 4, 5, and 6).
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Flowchart of the Study Selection Procedure
Drugs (Part 1)
| Drug | Year |
|---|---|
| Morphine | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Chandok and Watt (16) | 2010 |
| Rhee and Broadbent (17) | 2007 |
| Ferslew et al. (18) | 2015 |
| Dzierlenga et al. (19) | 2015 |
| Chen et al. (20) | 2010 |
| Shinagawa et al. (21) | 2008 |
| Razaq et al. (22) | 2007 |
| Kim and Harbott (23) | 2004 |
| Kotb et al. (24) | 1997 |
| Hasselstrom et al. (25) | 1990 |
| Crotty et al. (26) | 1989 |
| Mazoit et al (27) | 1987 |
| Patwardhan et al. (28) | 1981 |
| Imani et al. (29) | 2014 |
| Hydrocodone (Hydromorphone) | |
| Harrison (4) | 2012 |
| Lewis and Stine (11) | 2013 |
| Swetz et al. (14) | 2010 |
| Chandok and Watt (16) | 2010 |
| Razaq et al. (22) | 2007 |
| Imani et al. (29) | 2014 |
| Mort et al. (30) | 2011 |
| Oxycodone | |
| Lewis and Stine (11) | 2013 |
| Chandok and Watt (16) | 2010 |
| Mort et al. (30) | 2011 |
| Bosilkovska et al. (31) | 2012 |
Drugs (Part 2)
| Drug | Year |
|---|---|
| Codeine | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Golzari et al. (15) | 2014 |
| Chandok and Watt (16) | 2010 |
| Imani et al. (29) | 2014 |
| Tegeder et al. (32) | 2011 |
| Meperidine, (Pethidine) | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Chandok and Watt (16) | 2010 |
| Bosilkovska et al. (31) | 2012 |
| Katzung and Antony (32) | 2010 |
| Tegeder et al. (33) | 1999 |
| Grewal et al. (34) | 1997 |
| Danziger et al. (35) | 1994 |
| Pond et al. (36) | 1981 |
| Dwyer et al. (37) | 2014 |
| Methadone | |
| Lewis and Stine (11) | 2013 |
| Chandok and Watt (16) | 2010 |
| Katzung and (32) | 2010 |
| Tegeder et al. (33) | 1999 |
| Dwyer et al. (37) | 2014 |
| Tintinalli et al. (38) | 2010 |
| Murphy (39) | 2005 |
| Saxon et al. (40) | 2013 |
Drugs (Part 3)
| Drug | Year |
|---|---|
| Tramadol | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Chandok and Watt (16) | 2010 |
| Bosilkovska et al. (31) | 2012 |
| Website (41) | 2011 |
| Katzung and Antony (32) | 2010 |
| Tegeder et al. (33) | 1999 |
| Dwyer et al. (37) | 2014 |
| Tintinalli et al. (38) | 2010 |
| Murphy (39) | 2005 |
| Frank et al. (42) | 2012 |
| Loughrey et al. (43) | 2003 |
| Koth et al. (44) | 2008 |
| Buprenorphine | |
| Tegeder et al. (33) | 1999 |
| Dwyer et al. (37) | 2014 |
| Murphy (39) | 2005 |
| Frank et al. (42) | 2012 |
| Zuin et al (45) | 2008 |
| Taura et al. (46) | 2003 |
| Donaher and Welsh (47) | 2006 |
| Soyka et al. (48) | 2014 |
| Eiden et al. (49) | 2013 |
| Ciccozzi et al. (50) | 2012 |
| Saxon et al. (40) | 2013 |
| Reddy et al. (51) | 2007 |
| Bruce and Altice (52) | 2007 |
| Deybach and Blanlœil (53) | 1989 |
| Juby et al. (54) | 1994 |
Drugs (Part 4)
| Drugs | Year |
|---|---|
| Pentazocine | |
| Tegeder et al. (13) | 1999 |
| Katzung and Antony (32) | 2010 |
| Tegeder et al. (33) | 1999 |
| Frank et al. (42) | 2012 |
| Pond et al. (55) | 1980 |
| Dextropropoxyphene | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Mort et al. (30) | 2011 |
| Katzung and Antony (32) | 2010 |
| Frank et al. (39) | 2005 |
| Frank et al. (42) | 2012 |
| Bergeron et al. (56) | 2002 |
| Rosenberg et al. (57) | 1993 |
Drug (Part 5)
| Drug | Year |
|---|---|
| Fentanyl | |
| Lewis and Stine (11) | 2013 |
| Tegeder et al. (13) | 1999 |
| Swetz et al. (14) | 2010 |
| Chandok and Watt (16) | 2010 |
| Bosilkovska et al.(31) | 2012 |
| Katzung and Antony (32) | 2010 |
| Tintinalli et al.(38) | 2010 |
| Murphy (39) | 2005 |
| Ko et al. (58) | 2012 |
| Haberer et al. (59) | 1982 |
| Jin et al. (60) | 2011 |
| Pouraghaei et al. (61) | 2014 |
| Remifentanil | |
| Soleimanpour et al. (2) | 2015 |
| Lewis and Stine (11) | 2013 |
| Bosilkovska et al. (31) | 2012 |
| Murphy (39) | 2005 |
| Frank et al. (42) | 2012 |
| Servin (62) | 2003 |
| Hagiwara et al. (63) | |
| McCammon et al. (64) | 1978 |
| Dershwitz and Rosow (65) | 1996 |
| Dumont et al. (66) | 1998 |
| Wilhelm and Kreuer (67) | 2008 |
Drugs (Part 6)
| Drugs | Year |
|---|---|
| Sufentanil | |
| Tegeder et al.(13) | 1999 |
| Soleimanpour et al. (2) | 2015 |
| Lewis and Stine (11) | 2013 |
| Bosilkovska et al. (31) | 2012 |
| Tegeder et al. (33) | 1999 |
| Murphy (39) | 2005 |
| Frank et al. (42) | 2012 |
| Pouraghaei et al. (61) | 2014 |
| Wilhelm and Kreuer (67) | 2008 |
| Chauvin et al. (68) | 1989 |
| Alfentanil | |
| Tegeder et al. (13) | 1999 |
| Bosilkovska et al. (31) | 2012 |
| Katzung and Antony (32) | 2010 |
| Tegeder et al. (33) | 1999 |
| Murphy (Murphy 2005) | 2005 |
| Frank et al. (42) | 2012 |
| Pouraghaei et al.(61) | 2014 |
| Wilhelm and Kreuer (67) | 2008 |
| Baririan et al.(69) | 2007 |
| Davis et al. (70) | 1989 |
The metabolism, effects, and adverse reactions of each opioid are discussed in the following paragraphs.
3.1. Morphine
Morphine is a very potent opioid. It is obtained from opium which is the most effective compound. Morphine mimics the body’s endorphins through µ and k receptors in the central nervous system (CNS) (11, 13).
Medicinal morphine products are available in three forms: oral (tablets and capsules), parenteral (intravenous, subcutaneous, and intramuscular) and suppositories. Utilization through inhalation is also possible. Ninety percent of morphine is metabolized by the liver and excreted by the kidneys. Morphine is metabolized into two main metabolites through the glucuronidation pathways: morphine-3-glucuronide (M3G) (60%) and morphine-6-glucuronide (M6G). M6G is an active quencher, which is a more potent analgesic than morphine; M3G has no analgesic effect, but it leads to neurotic adverse drug reactions (neurotoxicity) such as confusion. Morphine may also be metabolized into small amounts of neuro-morphine, codeine and hydro-morphine. Reducing morphine clearance from plasma and increasing the half-life of the drug in the blood are reported as consequences of its concentration (16, 17).
Using morphine increases the levels of fasting bile acids in patients with nonalcoholic steatohepatitis; although metabolism of morphine does not change in these patients, morphine is eventually accumulated and leads to morphine poisoning (18, 19). The amount of morphine for pain relief was significantly lower in group three among the following three groups of patients who underwent surgery. Groups included: 1, kidney transplant donors; 2, patients with liver cirrhosis and hepatitis B or C; 3, patients with end-stage liver disease (20). In one case, the use of slow-release oral morphine for pain relief led to hepatic encephalopathy in a patient with cirrhosis and liver cancer (21). It was found that opioids, especially morphine and hydromorphone should be used with caution in older patients due to reduced liver and kidney function and underlying diseases (22). It was found that morphine and fentanyl can be easily used in a child with cirrhosis who was a candidate for liver transplantation (23). Slow-release morphine can be used with minimal doses and long intervals for pain relief in patients with liver cirrhosis due to hepatitis B and C treated by sclerotherapy (24). The half-life of oral and intravenous morphine is increased in patients with severe hepatic cirrhosis; hence, it should be cautiously used in such patients (25). Hepatic excretion of morphine is changed in patients with cirrhosis (26). The final half-life of unchanged morphine (not metabolized) is also longer in patients with liver cirrhosis (27). Removal of morphine storage is not affected by moderate and severe cirrhosis. However, morphine leads to mild sedation in these people, it does not lead to hepatic coma (28). In patients with liver disease, the minimum dose of the drug should be used with the usual dose of medicine at regular intervals in the early stages. If the liver failure is progressive, the usual dose should still be used, but the medication interval should be extended (29).
3.2. Hydrocodone, Hydromorphone
Hydrocodone belongs to the group of long-acting or slow sustained release opioid analgesics. It is a semi-synthetic drug derived from codeine and is used as an analgesic antitussive (4, 11, 14). Its drug products are available only in oral form or in combination with non-opioid drugs such as acetaminophen. Hydrocodone is a pre-drug that is metabolized into hydromorphone and oxymorphone by Cyp2D6 in the liver. Hydrocodone dosage titration is limited due to its non-narcotic composition (16, 22, 29).
In patients with hepatic failure, the half-life of hydromorphone is increased; therefore, overuse of these drugs can certainly be toxic for the liver (17). In patients with severe liver disease, the initial dose of both drugs should be reduced to 50% the standard dose; if the disease is not advanced, then increasing the dose distances may be necessary (15, 30, 71).
3.3. Oxycodone
Oxycodone is a semi-synthetic opioid which acts through κ and µ opioid receptors (k-opioid receptors). Its pharmaceutical products are provided in the oral (tablets) and parenteral (intramuscular, intravenous) forms. Oxycodone is metabolized into α and β oxycodone metabolites by the CYP3A4 and CYP2d6 pathways in the liver. However, none of these metabolites show considerable quencher activity. In advanced liver failure, the plasma concentration of oxycodone is increased up to 40%, half-life of quick release of the drug is increased to 6.4 to 24.6 hours with an average of 14 hours, and its useful half-life is raised to 3.5 hours (11, 16). Oxycodone is administered in combination with paracetamol and its consumption leads to liver dysfunction (30). Bioavailability of hydromorphone and oral oxycodone in patients with liver problems is dramatically increased; therefore, their doses should be reduced or the interval between administrations should be increased (31). The initial dose of oxycodone in patients with severe hepatic insufficiency should be reduced to 30% - 50% of the standard starting dose (15, 71).
3.4. Codeine
Codeine, or 3-methylmorphine, is an opioid which acts as an analgesic, antitussive, anti-hypertensive, anti-anxiety and sedative, and it has hypnotic effects. Its oral, suppository, or injection (subcutaneous and intramuscular) medication forms are available (11, 13, 15).
Codeine is converted to morphine by cytochrome p450 Cyp2D6 enzymes in the liver. Since codeine is not metabolized in patients with hepatic failure (due to the reduced capacity of the enzyme), its analgesic effects may not appear in this group of patients; therefore, patients with hepatic failure should avoid taking these drugs (16, 29). Another analgesic instead of codeine is recommended to control pain in patients with liver failure (13, 71). Although codeine is frequently used to treat patients with liver failure, especially patients with cirrhosis, because of its conversion to morphine, serum levels can be highly variable (71). Codeine can cause respiratory depression called morphinemia in patients with liver failure because of the accumulation of its metabolite (29, 41).
3.5. Meperidine (Pethidine)
Pethidine is a synthetic opioid. It has lower addictive properties than morphine. It has an analgesic effect via the μ-opioid receptors. Oral (tablets) and parenteral (intravenous, intramuscular) medication forms are available (11, 13, 32).
Pethidine is converted to norpethidine through methylation, and becomes pethidine acid through hydrolyzing by CYP3A4 and CYP2B6. Norpethidine is responsible for more than 50% of the analgesic effect in pethidine. In liver disease, the clearance of meperidine is reduced, and its half-life is prolonged. Seizure is a common adverse drug reaction of meperidine and normeperidine which may occur even at reduced dosages in patients with hepatic insufficiency (15, 16). In addition, this compound is responsible for the neurotoxic effects of hallucinogens and seizures of pethidine. Most pethidine metabolites are excreted in the form of glucuronic acid from the kidney; therefore, a more neurotoxic effect appears in kidney failures (16, 31, 32). In renal failure, meperidine can cause seizure due to accumulation of its toxic metabolites i e, normeperidine, but it should be cautiously administered in liver failure (33). In patients with lysosomal storage diseases such as Niemann-Pick, meperidine can be used for sedation of children to examine diagnosis and biopsy (34). Normeperidine is the toxic metabolite of meperidine, excreted through the kidneys; therefore, it increases in patients with renal failure and cancer. In patients with liver cirrhosis, meperidine is decreased; thus its accumulation causes CNS suppression and hepatic encephalopathy (35). Meperidine administration mode does not affect its metabolism. Meperidine production is lower in patients with cirrhosis due to impaired liver function and its toxic effects are lower, but its toxic effects appear due to cumulative effect and its narcotic effects on the CNS increase (36).
3.6. Methadone
Methadone is a potent synthetic opiate drug which is less addictive than morphine and heroin. It is utilized as a maintenance drug for heroin addiction inhibition (11, 32).
It has oral, parenteral (intravenous, intramuscular), suppositories, inhalation and subcutaneous medicinal forms. It is metabolized by enzymes cyp3A4 and 1A2 in the liver; therefore, its clearance is reduced in severe hepatic insufficiency. Although methadone is a drug with a high affinity for binding to protein, it does not produce toxic metabolites (32, 37, 38). Thus, it is better tolerated in patients with liver failure. If standard and regular doses of methadone are utilized, information shows no change in patients with mild to moderate hepatic insufficiency (16, 33). However, in patients with severe hepatic failure, the half-life of the drug increases, and it should be taken with caution (13, 38). In patients with hypoalbuminemia, the lowest dose should be given (29). Methadone is contraindicated in severe liver disease (39).
3.7. Tramadol
Tramadol is known with the trade names Tramal, Tram and Biomadole. It is an opium-like pain killer that is considered as an opioid. Tramadol is administrated for relief of moderate to severe pain. Tramadol is an agonist for the μ opioid receptor and noradrenergic and serotonergic systems receptors that increase serotonin release and inhibit norepinephrine reuptake. The medicinal forms of this drug are available as tablets (retard), drops, injections and suppositories (11, 16, 38).
Tramadol is metabolized by cyp3A4 and cyp2D6 in the liver, and it is excreted in the urine. When receiving 100 mg of tramadol, the blood level of the drug reaches maximum amounts in two hours. Thirty percent of tramadol remains unchanged, and 60% of it is excreted in the urine as broken metabolites in the liver. The half-life of the drug is four to six hours. The compounds are metabolized to active metabolites in the liver which show the quencher effects. Since the metabolic enzymes of the liver are reduced in patients with liver failure, the drug may not be metabolized to its active metabolites that reduce the effects of the enzymes. Basically, the use of alternative materials for pain relief is recommended (13, 31, 41). Similar side effects of other opium-like drugs are also observed in tramadol (nausea, dizziness, drowsiness, dry mouth, delayed ejaculation, constipation, hypotension, sweating and itching). However, the risk of respiratory depression, which is the most fatal complication of these drugs, appears less with oral tramadol than with morphine (32, 33, 37). The consumption of this drug causes nausea more than the consumption of other opioids because of the increased levels of serotonin. For people without physical dependency to opioids, the consumption of more than 400 mg of tramadol will be dangerous. Seizure is one of the rare but serious adverse reactions of tramadol. Seizure is usually caused by utilizing too much of the drug in patients with epilepsy and brain injury, those who have kidney or liver problems, or people who are addicted to alcohol. In some studies, it is suggested that tramadol is one of the opiates administered in patients with severe and persistent pain of cirrhosis (Its effects on peripheral pain pathways for inhibition of relative serotonin reuptake are low affinity for opioid receptors). Constipation appears because of the anticholinergic effects of tramadol. The use of tramadol in patients with liver failure has led to challenges (32, 38, 41, 42). High doses of tramadol caused the death of a 67-year-old male with a painful rib fracture. Pathology revealed that it was because of acute liver failure due to fulminant liver necrosis. It was the first report of tramadol-induced hepatic failure (43).
Oral tramadol can be used for patients with primary cancer or metastatic liver cancer, provided that administration intervals are more, therefore, a dose of 50 mg every 12 hours can be effective and safe (44).
3.8. Buprenorphine
Buprenorphine is a semi-synthetic opioid derived from the baine. It is a partial agonist of µ receptors, and is also a potent antagonist of k receptors. This drug is also useful to treat drug addicts (32, 42).
The medicinal forms of buprenorphine include injectable (intravenous, intramuscular), suppositories, sublingual, intranasal and transdermal forms. It is metabolized in the liver, processed by cyp2c8 and cyp3A4 to norbuprenorphine, and excreted through the kidneys and bile. In patients with severe cholestasis, the clearance of drugs which are metabolized in the liver, such as buprenorphine, are threatened (33, 37, 39). Buprenorphine is a semi-synthetic opioid, more often used to treat heroin dependency withdrawal. Liver threatening complications are reported at therapeutic doses in a few patients with hepatitis C. Pathologic study revealed that mitochondria are mostly affected by toxic effects of buprenorphine (45). In patients with hepatitis B or C, opioids may be used to reduce pain; however, in this group of patients liver function should be evaluated through tests (46). Particularly in patients with hepatitis C, repeated intravenous administrations of buprenorphine will definitely cause liver damage (47). A 12-month study revealed that although treatment with buprenorphine or naloxone can lead to increased liver enzymes in the treatment of opioid dependents, it will not lead to liver damage, therefore, it can be used safely (48). The use of nasal buprenorphine is increasing and one case was reported to cause hepatitis and renal failure (49). Higher doses of buprenorphine can be used in end stage ill patients with progressive liver failure (50). A study revealed that the use of buprenorphine in the first six months in patients with underlying hepatitis B and C slightly affects the increased serum levels of liver enzymes (40). Transdermal buprenorphine can be effective in the treatment of pruritus in patients with primary biliary disease, but does not exacerbate liver complications (51). Liver enzymes level are increased in patients with hepatitis C who are treated with buprenorphine; however, buprenorphine treatment is well tolerated by such patients and enzyme levels return to normal level after cessation of treatment (52). Buprenorphine can be used for patients with hepatic porphyria, and has no effect on their liver function (53). Buprenorphine should be cautiously used in patients with severe hepatic pruritus due to cholestasis (54).
3.9. Pentazocine
Pentazocine is a synthetic drug which is the agonist or antagonist of opioids. Its drug forms include oral and intravenous (IV) (42).
The metabolism of pentazocine is hepatic, and it is excreted through the urine. It is more likely to cause illusions than morphine. In patients with the precedent of addiction, it causes withdrawal symptoms. The doses of this drug should be reduced in patients with hepatic insufficiency (13, 33). It is required to administer pentazocine cautiously in patients with diseases of the gallbladder and bile ducts (32, 55). Bioavailability of meperidine and pentazocine is increased in patients with liver cirrhosis; therefore, oral doses of these medications should be reduced in these patients, and when there is a need to repeat the dose in oral or intravenous mode, intervals should be prolonged between doses or repeated dose should be less than the initial dose (55).
3.10. Dextropropoxyphene
Dextropropoxyphene is a synthetic and weak opioid analgesic which affects μ receptors and is metabolized in the liver (32, 42).
The only drug product of dextropropoxyphene is the oral form available in combination with non-opioid drugs such as acetaminophen (11, 13). Evaluation of four patients showed that dextropropoxyphene and paracetamol combination can cause hepatotoxicity and can occur in form of cholestasis or cytolytic hepatitis or cholangitis, but the outcome of these patients is better as the discontinuation of the medication will lead to disappearance of the changes (56). A study of 90 patients showed that dextropropoxyphene will cause hepatotoxicity; biopsies of patients demonstrated that the drug can cause centrilobular cholestasis (57). The blood level of this drug increases in chronic liver disease which intensifies its effects (30, 39, 42).
3.11. Fentanyl
Fentanyl is an opioid with a high absorption coefficient of the liver that binds to serum albumin. Fentanyl is available in TD, intramuscular (IM), intravenous (IV), oral, transmucosal, sublingual and buccal medicinal forms.
This drug is mainly metabolized by the liver and is excreted through the kidneys (11, 14). Moreover, less than 8% of the drug is excreted through the kidneys without being metabolized in the liver (32, 38). Fentanyl is primarily metabolized by cyp3A4 and is distributed in the muscle and fat immediately after administration. Although the duration of its half-life, dose repetition and single-dose were prolonged, the single-dose pharmacokinetics of intravenous fentanyl in patients with liver failure did not change (39). There is no information about its continuous infusion consumption (13, 16). Transdermal fentanyl is not adequately studied for the treatment of hepatic failure; however, it is assumed that liver failure can alter the permeability of the skin and drug absorption. The clinical relevance of this, however, has not been determined (17, 48). Although pharmacokinetics of phenyl pyridines such as fentanyl, sufentanil and remifentanil is not affected in patients with liver failure, all of them can cause hepatic encephalopathy, particularly in patients with severe liver failure (31). In patients with liver cirrhosis who undergo general anesthesia, fentanyl pharmacokinetics is not initially affected (58). Most opioids are metabolized in liver through glucuronidation, but fentanyl is cleared by the hydrolysis of ester (59). It was found that morphine and fentanyl can be easily used in a child with cirrhosis who was a candidate for liver transplantation (23). Some experts recommend fentanyl as a proper opioid for liver failure, but that is an entirely empirical judgment (60, 61, 71).
3.12. Remifentanil
Remifentanil is an ultra-short-acting synthetic drug and also a potent agonist for µ receptors. It contains all pharmacokinetic properties of this class of drugs (analgesic, hemodynamic stability, respiratory depression, muscle tightness, itching, nausea and vomiting) (11, 42, 62).
It is available as an intravenous drug form. Unlike other opioids, Remifentanil has no hepatic metabolism; it is metabolized by nonspecific tissue and plasma esterase and is broken to remifentanil (42, 62). Since histamine is released during the drug administration, an antihistamine drug should be administered simultaneously (2, 39). Although pharmacokinetics of phenyl pyridines such as fentanyl, sufentanil and remifentanil are not affected in patients with liver failure, all of them can cause hepatic encephalopathy, particularly in patients with severe liver failure (31). In a report about a 74-year-old female with underlying liver and kidney problems who underwent hepatectomy, it was found that remifentanil can be quite effective and used safely (63). In patients with severe impairment of the hepatic metabolism, remifentanil remains unchanged and does not cause hepatic encephalopathy. Therefore, it could be a good post-operative analgesic (64, 65). Remifentanil can be used for patients with severe liver dysfunction (66, 67).
3.13. Sufentanil
Sufentanil is a synthetic opioid that is 5- to 10-times more potent than fentanyl. It is available in IV, IM, subcutaneous (sub-Q), epidural, intrathecal, and transdermal patch (in clinical trials) drug forms. This drug is metabolized in the liver (2, 11, 13, 42). The half-life of an intravenous single dose of sufentanil does not change in liver failure (61).
Although pharmacokinetics of phenyl pyridines such as fentanyl, sufentanil and remifentanil are not affected in patients with liver failure, all of them can cause hepatic encephalopathy, particularly in patients with severe liver failure (31, 33). Sufentanil should be cautiously utilized in patients with hepatic insufficiency, similar to fentanyl and alfentanil (39). This is also true regarding the continuous consumption of its infusion in the ICU (61, 68). Sufentanil can have a similar effect in a single dose on patients with uncomplicated liver cirrhosis and patients with normal liver function (67, 68).
3.14. Alfentanil
Alfentanil has a short-term effect, synthetic opioid fentanyl is 4 times faster than fentanyl. It affects μ receptors and causes less cardiovascular complications than fentanyl and remifentanil (13, 31, 39). It is available as an intravenous medicinal form. Alfentanil is metabolized in the liver (32, 42).
In patients with mild to moderate cirrhosis, the miosis created by alfentanil can be an alternative measure of the pharmacokinetic alfentanil (69). In children with cholestatic liver disease, alfentanil can be easily used as an analgesic and the dose is similar to normal people and should not be changed (70). A lower dose of this drug must be administrated to patients with chronic liver failure due to the reduced clearance of alfentanil and its concentration in the blood (33, 61, 67).
4. Conclusions
In patients with liver disease who need the pain medication relief, caution should be made in the administration of opioid analgesics. The correct dose of drug is the one which relieves the pain and has fewer adverse drug reactions (13, 72). As a general rule, it is necessary to use low doses of medication at regular intervals according to the signs of drug accumulation. Pain management in patients with liver problems has always been a challenge because of the effects of drugs, especially opioids (14, 71). Opioids should be used cautiously since it causes analgesia, sedation, constipation and sudden encephalopathy in patients with liver failure (39). On the other hand, pain management in patients with cirrhosis is a difficult clinical challenge for health care providers (61, 62). Safely relieving the symptoms of pain is one of the tasks of health care providers. Moreover, it is believed that these precautions should be made by all health care providers involved in the treatment. Although it is recommended that opioids be used with caution, the fear of sudden encephalopathy and the sedative effects of these drugs are facts. The appropriate management of pain therapy in patients with liver failure who are candidates for liver transplantation is important in order to improve the performance and quality of life for this group of patients. For the patients with hepatic insufficiency who are not candidates for liver transplantation, palliative treatment is sometimes necessary and some opioids can be used (13, 14). Opiates can be safely used to reduce pain and distress even in patients with advanced liver disease, advanced kidney disease, lung disease, and heart disease, as these drugs are preferred to NSAID and other pain relief medications (14, 73). In various methods, low doses of opioids such as fentanyl are routinely used intravenously (with a short half-life), oral or intravenous hydromorphone is used to relieve pain, and the researchers believe that these methods can be safe. Since clearance of these drugs is decreased in patients with hepatic insufficiency, the initial dose should be reduced while the intervals between doses increased, and in some cases there will be a need for continuous visits and control of vital signs. The adverse drug reactions of opioids can be reversed by naloxone (64, 74).
Acknowledgements
References
-
1.
Kamath PS, Kim WR, Advanced Liver Disease Study. The model for end-stage liver disease (MELD). Hepatology. 2007;45(3):797-805. [PubMed ID: 17326206]. https://doi.org/10.1002/hep.21563.
-
2.
Soleimanpour H, Safari S, Rahmani F, Jafari Rouhi A, Alavian SM. Intravenous Hypnotic Regimens in Patients With Liver Disease; A Review Article. Anesthesiology and Pain Medicine. 2015;5(1). https://doi.org/10.5812/aapm.23923.
-
3.
Murray JF, Dawson AM, Sherlock S. Circulatory changes in chronic liver disease. Am J Med. 1958;24(3):358-67. https://doi.org/10.1016/0002-9343(58)90322-x.
-
4.
Harrison principle of internal medicine. 18th. New York: MC Graw-Hill; 2012.
-
5.
Hoofnagle J. Fulminant hepatic failure: Summary of a workshop*1. Hepatology. 1995;21(1):240-52. https://doi.org/10.1016/0270-9139(95)90434-4.
-
6.
Soleimanpour H, Safari S, Rahmani F, Ameli H, Alavian SM. The Role of Inhalational Anesthetic Drugs in Patients with Hepatic Dysfunction: A Review Article. Anesthesiology and Pain Medicine. 2015;5(1). https://doi.org/10.5812/aapm.23409.
-
7.
Parker BM, Bhatia S, Younossi Z, Henderson JM, Tetzlaff JE. Autonomic dysfunction in end-stage liver disease manifested as defecation syncope: impact of orthotopic liver transplantation. Liver Transpl Surg. 1999;5(6):497-501. [PubMed ID: 10545537].
-
8.
De Wolf AM. 6/2/06 Perioperative assessment of the cardiovascular system in ESLD and transplantation. Int Anesthesiol Clin. 2006;44(4):59-78.
-
9.
Tripodi A, Mannucci PM. The coagulopathy of chronic liver disease. N Engl J Med. 2011;365(2):147-56. [PubMed ID: 21751907]. https://doi.org/10.1056/NEJMra1011170.
-
10.
Njoku DB. Drug-induced hepatotoxicity: metabolic, genetic and immunological basis. Int J Mol Sci. 2014;15(4):6990-7003.
-
11.
Lewis JH, Stine JG. Review article: prescribing medications in patients with cirrhosis–a practical guide. AP and t. 2013;37(12):1132-56.
-
12.
Zamora Nava LE, Valadez JA, Chávez-Tapia NC, Torre A. Acute-on-chronic liver failure: a review. Ther Clin Risk Manag. 2014;10.
-
13.
Tegeder I, Lotsch J, Geisslinger G. Pharmacokinetics of opioids in liver disease. Clin Pharmacokinet. 1999;37(1):17-40. [PubMed ID: 10451781]. https://doi.org/10.2165/00003088-199937010-00002.
-
14.
Swetz KM, Carey EC, Rho RH, Mauck WD, Whitford KJ, Moynihan TJ, et al. Safe use of opioids to manage pain in patients with cirrhosis. Mayo Clin Proc. 2010;85(10):959. author reply 960. [PubMed ID: 20884829]. https://doi.org/10.4065/mcp.2010.0294.
-
15.
Golzari SEJ, Soleimanpour H, Rahmani F, Mehr NZ, Safari S, Heshmat Y, et al. Therapeutic approaches for renal colic in the emergency department: a review article. Anesthesiology and pain medicine. 2014;4(1).
-
16.
Chandok N, Watt KD. Pain management in the cirrhotic patient: the clinical challenge. Mayo Clin Proc. 2010;85(5):451-8. [PubMed ID: 20357277]. https://doi.org/10.4065/mcp.2009.0534.
-
17.
Rhee C, Broadbent AM. Palliation and liver failure: palliative medications dosage guidelines. J Palliat Med. 2007;10(3):677-85. [PubMed ID: 17592979]. https://doi.org/10.1089/jpm.2006.0246.
-
18.
Ferslew BC, Johnston CK, Tsakalozou E, Bridges AS, Paine MF, Jia W, et al. Altered morphine glucuronide and bile acid disposition in patients with nonalcoholic steatohepatitis. Clinical Pharmacology & Therapeutics. 2015;97(4):419-27. https://doi.org/10.1002/cpt.66.
-
19.
Dzierlenga AL, Clarke JD, Hargraves TL, Ainslie GR, Vanderah TW, Paine MF, et al. Mechanistic Basis of Altered Morphine Disposition in Nonalcoholic Steatohepatitis. Journal of Pharmacology and Experimental Therapeutics. 2015;352(3):462-70. https://doi.org/10.1124/jpet.114.220764.
-
20.
Chen JP, Jawan B, Chen CL, Wang CH, Cheng KW, Wang CC, et al. Comparison of Postoperative Morphine Requirements in Healthy Living Liver Donors, Patients With Hepatocellular Carcinoma Undergoing Partial Hepatectomy, and Liver Transplant Recipients. Transplantation Proceedings. 2010;42(3):701-2. https://doi.org/10.1016/j.transproceed.2010.02.024.
-
21.
Shinagawa J, Hashimoto Y, Ohmae Y. [A case of hepatic encephalopathy induced by adverse effect of morphine sulfate]. Gan To Kagaku Ryoho. 2008;35(6):1025-7. [PubMed ID: 18633239].
-
22.
Razaq M, Balicas M, Mankan N. Use of hydromorphone (Dilaudid) and morphine for patients with hepatic and renal impairment. Am J Ther. 2007;14(4):414-6. [PubMed ID: 17667220]. https://doi.org/10.1097/01.pap.0000249926.89087.d8.
-
23.
Kim TW, Harbott M. The use of caudal morphine for pediatric liver transplantation. Anesth Analg. 2004;99(2):373-4. table of contents. [PubMed ID: 15271708]. https://doi.org/10.1213/01.ANE.0000122822.58156.48.
-
24.
Kotb HI, el-Kabsh MY, Emara SE, Fouad EA. Pharmacokinetics of controlled release morphine (MST) in patients with liver cirrhosis. Br J Anaesth. 1997;79(6):804-6. [PubMed ID: 9496218].
-
25.
Hasselstrom J, Eriksson S, Persson A, Rane A, Svensson JO, Sawe J. The metabolism and bioavailability of morphine in patients with severe liver cirrhosis. Br J Clin Pharmacol. 1990;29(3):289-97. [PubMed ID: 2310653].
-
26.
Crotty B, Watson KJ, Desmond PV, Mashford ML, Wood LJ, Colman J, et al. Hepatic extraction of morphine is impaired in cirrhosis. Eur J Clin Pharmacol. 1989;36(5):501-6. [PubMed ID: 2753069].
-
27.
Mazoit JX, Sandouk P, Zetlaoui P, Scherrmann JM. Pharmacokinetics of unchanged morphine in normal and cirrhotic subjects. Anesth Analg. 1987;66(4):293-8. [PubMed ID: 3565791].
-
28.
Patwardhan RV, Johnson RF, Hoyumpa AJ, Sheehan JJ, Desmond PV, Wilkinson GR, et al. Normal metabolism of morphine in cirrhosis. Gastroenterology. 1981;81(6):1006-11. [PubMed ID: 7286578].
-
29.
Imani F, Motavaf M, Safari S, Alavian SM. The therapeutic use of analgesics in patients with liver cirrhosis: a literature review and evidence-based recommendations. Hepat Mon. 2014;14(10). ee23539. [PubMed ID: 25477978]. https://doi.org/10.5812/hepatmon.23539.
-
30.
Mort JR, Shiyanbola OO, Ndehi LN, Xu Y, Stacy. J. N. Opioid-paracetamol prescription patterns and liver dysfunction: a retrospective cohort study in a population served by a US health benefits organization. Drug Saf. 2011;34(11):1079-88. https://doi.org/10.2165/1159310.
-
31.
Bosilkovska M, Walder B, Besson M, Daali Y, Desmeules J. Analgesics in patients with hepatic impairment: pharmacology and clinical implications. Drugs. 2012;72(12):1645-69.
-
32.
Katzung BG, Antony J. Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill; 2010.
-
33.
Tegeder I, Geisslinger G, Lotsch J. [Therapy with opioids in liver or renal failure]. Schmerz. 1999;13(3):183-95. [PubMed ID: 12799931]. https://doi.org/10.1007/s004829900019.
-
34.
Grewal RP, Yu KT, Barton NW, Parker RI, Bisceglie AM. Liver biopsies in patients with lysosomal storage disease: experience with effective sedation. Indian J Pediatr. 1997;64(6):887-91. [PubMed ID: 10771935].
-
35.
Danziger LH, Martin SJ, Blum RA. Central nervous system toxicity associated with meperidine use in hepatic disease. Pharmacotherapy. 1994;14(2):235-8. [PubMed ID: 8197046].
-
36.
Pond SM, Tong T, Benowitz NL, Jacob P, Rigod J. Presystemic metabolism of meperidine to normeperidine in normal and cirrhotic subjects. Clin Pharmacol Ther. 1981;30(2):183-8. [PubMed ID: 7249503].
-
37.
Dwyer JP, Jayasekera C, Nicoll A. Analgesia for the cirrhotic patient: a literature review and recommendations. J Gastroenterol Hepatol. 2014;29(7):1356-60. [PubMed ID: 24548074]. https://doi.org/10.1111/jgh.12560.
-
38.
Tintinalli JE, Krome RL, Ruiz E. Emergency Medicine: A Comprehensive Study Guide. Adv Emerg Nurs J. 2010;14(3):74.
-
39.
Murphy EJ. Acute pain management pharmacology for the patient with concurrent renal or hepatic disease. Anaesth Intensive Care. 2005;33(3):311-22. [PubMed ID: 15973913].
-
40.
Saxon AJ, Ling W, Hillhouse M, Thomas C, Hasson A, Ang A, et al. Buprenorphine/Naloxone and methadone effects on laboratory indices of liver health: A randomized trial. Drug Alcohol Depend. 2013;128(1-2):71-6. https://doi.org/10.1016/j.drugalcdep.2012.08.002.
-
41.
hepatitis. 2011. Available from: www.hepatitiswa.com.au.
-
42.
Frank G, Wall LR, Rao SP, Rama B. Toxicologic Emergencies. 2012.
-
43.
Loughrey MB, Loughrey CM, Johnston S, O’Rourke D. Fatal hepatic failure following accidental tramadol overdose. Forensic Sci Int. 2003;134(2-3):232-3. https://doi.org/10.1016/s0379-0738(03)00132-4.
-
44.
Koth HI, Fouad IA, Fares KM, Mostafa MG, Abd El-Rahman AM. Pharmacokinetics of oral tramadol in patients with liver cancer. J Opioid Manag. 2008;4(2):99-104. [PubMed ID: 18557166].
-
45.
Zuin M, Giorgini A, Selmi C, Battezzati PM, Cocchi CA, Crosignani A, et al. Acute liver and renal failure during treatment with buprenorphine at therapeutic dose. Digestive and Liver Disease. 2008;41(7):e8-e10. https://doi.org/10.1016/j.dld.2007.12.014.
-
46.
Taura P, Fuster J, Blasi A, Martinez-Ocon J, Anglada T, Beltran J, et al. Postoperative pain relief after hepatic resection in cirrhotic patients: the efficacy of a single small dose of ketamine plus morphine epidurally. Anesth Analg. 2003;96(2):475-80. table of contents. [PubMed ID: 12538199].
-
47.
Donaher PA, Welsh C. Managing opioid addiction with buprenorphine. Am Fam Physician. 2006;73(9).
-
48.
Soyka M, Backmund M, Schmidt P, Apelt S. Buprenorphine-naloxone treatment in opioid dependence and risk of liver enzyme elevation: Results from a 12-month observational study. Am J Addict. 2014;23(6):563-9. https://doi.org/10.1111/j.1521-0391.2014.12131.x.
-
49.
Eiden C, Ripault MP, Larrey D, Faillie JL, Pinzani V, Pageaux GP, et al. Acute Hepatitis and Renal Failure Related to Intranasal Buprenorphine Misuse: Case Report and Analysis of Cases Reported to the French Network for Drug Monitoring. Ann Pharmacother. 2013;47(12):1721-6. https://doi.org/10.1177/1060028013507429.
-
50.
Ciccozzi MDA, Angeletti M, Baldascino MDG, Petrucci MDE, Bonetti MDC, De Santis MDS, et al. High dose of buprenorphine in terminally ill patient with liver failure: Efficacy and tolerability. J Opioid Manag. 2012;8(4):253-9. https://doi.org/10.5055/jom.2012.0123.
-
51.
Reddy L, Krajnik M, Zylicz Z. Transdermal buprenorphine may be effective in the treatment of pruritus in primary biliary cirrhosis. J Pain Symptom Manage. 2007;34(5):455-6. [PubMed ID: 17900853]. https://doi.org/10.1016/j.jpainsymman.2007.08.001.
-
52.
Bruce RD, Altice FL. Case series on the safe use of buprenorphine/naloxone in individuals with acute hepatitis C infection and abnormal hepatic liver transaminases. Am J Drug Alcohol Abuse. 2007;33(6):869-74. [PubMed ID: 17994482]. https://doi.org/10.1080/00952990701653875.
-
53.
Deybach JC, Blanlœil Y. Buprenorphine (Temgesic) can be used in hepatic porphyria. Ann Fr Anesth Reanim. 1989;8(5):525. https://doi.org/10.1016/s0750-7658(89)80022-x.
-
54.
Juby LD, Wong VS, Losowsky MS. Buprenorphine and hepatic pruritus. Br J Clin Pract. 1994;48(6):331. [PubMed ID: 7848799].
-
55.
Pond SM, Tong T, Benowitz NL, Jacob P. Enhanced bioavailability of pethidine and pentazocine in patients with cirrhosis of the liver. Aust N Z J Med. 1980;10(5):515-9. [PubMed ID: 6937164].
-
56.
Bergeron L, Guy C, Ratrema M, Beyens MN, Mounier G, Ollagnier M. [Dextropropoxyphene hepatotoxicity: four cases and literature review]. Therapie. 2002;57(5):464-72. [PubMed ID: 12611201].
-
57.
Rosenberg WMC, Ryley NG, Trowell JM, Mc Gee JO'D, Chapman RW. Dextropropoxyphene induced hepatotoxicity: a report of nine cases. Journal of Hepatology. 1993;19(3):470-4. https://doi.org/10.1016/s0168-8278(05)80560-4.
-
58.
Ko JS, Shin YH, Gwak MS, Jang CH, Kim GS, Lee SK. The Relationship between Postoperative Intravenous Patient-Controlled Fentanyl Analgesic Requirements and Severity of Liver Disease. Transplantation Proceedings. 2012;44(2):445-7. https://doi.org/10.1016/j.transproceed.2012.01.017.
-
59.
Haberer JP, Schoeffler P, Couderc E, Duvaldestin P. Fentanyl pharmacokinetics in anaesthetized patients with cirrhosis. Br J Anaesth. 1982;54(12):1267-70. [PubMed ID: 7171414].
-
60.
Jin S.J, Jung J.Y, Noh M.H, Lee S.H, Lee E.K, Choi B.M, et al. The Population Pharmacokinetics of Fentanyl in Patients Undergoing Living Donor Liver Transplantation. Clin Pharmacol Ther. 2011;90(3):423-31.
-
61.
Pouraghaei M, Moharamzadeh P, Soleimanpour H, Rahmani F, Safari S, Mahmoodpoor A, et al. Comparison Between the Effects of Alfentanil, Fentanyl and Sufentanil on Hemodynamic Status During Rapid Sequence Intubation in the Emergency Department. Anesth Pain Med. 2014;3(3). https://doi.org/10.5812/aapm.14618.
-
62.
Servin FS. Remifentanil: an update. Curr Opin Anaesthesiol. 2003;16(4):367-72. https://doi.org/10.1097/01.aco.0000084479.59960.3f.
-
63.
Hagiwara C, Mizutani K, Fukukita K, Asada A. [Use of remifentanil in a patient with renal failure and liver dysfunction undergoing hepatectomy]. Masui. 2009;58(5):623-5.
-
64.
McCammon RL, Viegas OJ, Stoelting RK, Dryden GE. Naloxone Reversal of Choledochoduodenal Sphincter Spasm Associated with Narcotic Administration. Anesthesiology. 1978;48(6):437. https://doi.org/10.1097/00000542-197806000-00011.
-
65.
Dershwitz M, Rosow CE. The pharmacokinetics and pharmacodynamics of remifentanil in volunteers with severe hepatic or renal dysfunction. JCA. 1996;8(3):S88-90. https://doi.org/10.1016/s0952-8180(96)90020-3.
-
66.
Dumont L, Picard V, Marti RA, Tassonyi E. Use of remifentanil in a patient with chronic hepatic failure. Br J Anaesth. 1998;81(2):265-7. [PubMed ID: 9813539].
-
67.
Wilhelm W, Kreuer S. The place for short-acting opioids: special emphasis on remifentanil. Critical Care. 2008;12(Suppl 3):S5.
-
68.
Chauvin M, Ferrier C, Haberer JP, Spielvogel C, Lebrault C, Levron JC, et al. Sufentanil pharmacokinetics in patients with cirrhosis. Anesth Analg. 1989;68(1):1-4. [PubMed ID: 2521279].
-
69.
Baririan N, Van Obbergh L, Desager JP, Verbeeck RK, Wallemacq P, Starkel P, et al. Alfentanil-induced miosis as a surrogate measure of alfentanil pharmacokinetics in patients with mild and moderate liver cirrhosis. Clin Pharmacokinet. 2007;46(3):261-70. [PubMed ID: 17328584]. https://doi.org/10.2165/00003088-200746030-00006.
-
70.
Davis PJ, Stiller RL, Cook DR, Brandom BW, Davis JE, Scierka AM. Effects of cholestatic hepatic disease and chronic renal failure on alfentanil pharmacokinetics in children. Anesth Analg. 1989;68(5):579-83. [PubMed ID: 2497657].
-
71.
Fairbank E. Opioid Use in LiverFailure. Available from: efairbank@swh.net.au.
-
72.
Soleimanpour H, Rahmani F, Safari S, Golzari SE. Hypothermia after cardiac arrest as a novel approach to increase survival in cardiopulmonary cerebral resuscitation: a review. Iran Red Crescent Med J. 2014;16(7). ee17497. [PubMed ID: 25237582]. https://doi.org/10.5812/ircmj.17497.
-
73.
Soleimanpour H, Hassanzadeh K, Vaezi H, Ej Golzari S, Esfanjani R, Soleimanpour M. Effectiveness of intravenous lidocaine versus intravenous morphine for patients with renal colic in the emergency department. BMC Urology. 2012;12(1):13. https://doi.org/10.1186/1471-2490-12-13.
-
74.
Mahmoodpoor A, Soleimanpour H, Nia KS, Panahi JR, Afhami M, Golzari SE, et al. Sensitivity of palm print, modified mallampati score and 3-3-2 rule in prediction of difficult intubation. Int J Prev Med. 2013;4(9):1063-9. [PubMed ID: 24130949].
